Alcoholic Metabolic Syndrome Patients
advertisement

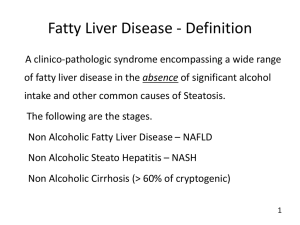
Prevalence of Metabolic Syndrome among patients with Nonalcoholic Liver Disease Peter Latimar L. Andrada M.D., Jose Tan M.D., FPCP, FPSG Metropolitan Medical Center, Department of Internal Medicine, Section of Gastroenterology ABSTRACT Objective: To determine the prevalence of metabolic syndrome among patients with nonalcoholic fatty liver disease (NAFLD). Study Design: This is a retrospective study, aiming to describe the clinical profile of 180 patients with fatty liver findings on ultrasound. Charts of selected patients seen with in the period betwwen Aug. 2004 to Aug. 2005 were reviewed. Participants: 180 patients age 19 years old and above with fatty liver findings on ultrasound were enrolled to the study. Patients who strongly denies significant alcoholic intake, intake of hepatotoxic drugs, with no history of chronic liver disease were included in the study. Results: Out of 180 only a total of 109 patients were diagnosed with NAFLD. The mean age was 47.815.6 with 70 were male (64.2%) and 39 were female (35.7%). Elevated SGPT was present in 71/108 (65.7%) subjects whereas elevated SGOT level was present in 14/42 (33.3%) subjects. Cholesterol above normal was present in 18 subjects (40.9%) and subjects with elevated triglyceride were 71 (69.6%). Obesity was the most prevalent predictor was present in 93 of 106 subjects (85.32%). Hypertension was present 66.1% (72/109) of subjects. Diabetes was also an important risk factor, is present in 47.7% (52/109) of subjects. Insulin resistance an additional risk factor for the development of NAFLD was noted in 16 out of 19 patients (84%) using the HOMA-IR index. And 51% (56/109) of the study group was noted to have Metabolic Syndrome. Conclusion: The preliminary data presented in the study showed prevalence of metabolic syndrome among patients with NAFLD at 51% (56/109) of the study group. Factors associated with metabolic syndrome among patients with NAFLD includes: obesity, hypertension, diabetes, hypertriglyceridemia. Category: Liver Article: Cross sectional Keywords: Non-alcoholic fatty liver disease or NAFLD Metabolic syndrome I-Introduction: Fatty Liver is a condition of hepatic steatosis caused by many risk factors and may progress to liver fibrosis and cirrhosis.1 It is consist of intrahepatic accumulation of lipids and the commonest liver disease accounting for abnormal function test in the majority of asymptomatic subjects.2 A common clinical condition frequently encountered on abdominal ultrasound however many clinicians often considered this as an incidental findings with scarce or no clinical significance.3 Only recently did Ludwig et al, identify a syndrome characterized by the association of fatty liver and lobular hepatitis and chronically elevated alanine aminotransferase plasma levels in patients with negligible alcohol intake. Thus the term non-alcoholic steatohepatosis (NASH) was introduced.4 The original syndrome was described predominantly in obese, 5-7 diabetics,8-10 and hyperdyslipidemics.8-12 Fatty liver is an increasingly common problem world wide and has been reported in Japan, 13-14 Australia,8 America,15-16 Europe,17 and Middle East.18 According to radiologic surveys; postmortem studies and evidence from the 3rd National Health and Nutrition Examination Survey (NHANES III), the prevalence of non-alcoholic fatty liver disease (NAFLD) of any type is from 16%-23% and the prevalence of steatohepatitis is from 2%-6% depending on diagnostic method used, both men and women are equally affected.19 Generally, the diagnosis of fatty liver should be based on the history, clinical manifestation, laboratory investigation and medical imaging. Liver biopsy is a useful and effective as a prognostic indicator but it is an invasive and costly tool that should be taken if necessary.20 However, previous studies in which ultrasound findings were compared to histologic result indicate that the overall sensitivity and specificity of ultrasonographic examination for the diagnosis of fatty liver are approximately 80%-95% and 90%-95% respectively.21-23 Retrospective case study was used to analyze the prevalence of metabolic syndrome in nonalcoholic fatty liver diagnosed by ultrasonography in patients admitted in Metropolitan Medical Center, Department of Internal Medicine. II- Significance of the study: The study would like to create awareness among physicians that in patients with ultrasounds findings of fatty liver, one must further investigate and include work up for metabolic syndrome. Thus early diagnosis and treatment in this condition would be done in order to prevent its progression to end stage liver disease. III- Objectives: A. General Objective: The aim of the study is to determine the prevalence Metabolic Syndrome in patients with Non alcoholic fatty liver disease (NAFLD). B. Specific Objective: 1. To describe the socio-demographic profile of patients with non-alcoholic fatty liver disease. 2. To determine the association of non-alcoholic fatty liver disease and metabolic syndrome based on its clinical presentations as defined by the NCEP ATP III such as hypertension, hypertriglyceridemia, decreased serum HDL, impaired fasting glucose and obesity. (Appendix A) IV- Methodology: Study Design: This is a retrospective study with descriptive cross sectional mode of data analysis aiming to describe the clinical profile of patients with non-alcoholic fatty liver disease diagnosed by ultrasonography as seen in Metropolitan Medical Center, with special emphasis on the risk factors among selected patients. Study population: This is a chart review of 256 selected patients age 19 years old and above with fatty liver over a one year period between August 2004 to August 2005 at Metropolitan Medical Center. Patients seen as in and out-patient who strongly denies significant alcoholic intake, intake of hepatotoxic drugs, with no history of chronic liver disease was included in the study. Fatty liver was diagnosed by ultrasonography using a Hitachi EUB-525 abdominal probe at 3.5 MHz. Longitudinal, subcostal, ascending and oblique scans were performed. The ultrasonographic criteria which were used to diagnose a fatty liver included liver and kidney echo discrepancy and presence of an increased liver echogenicity or “bright liver”, echo penetration into deep portion of the liver and clarity of the liver’s blood vessel structures. In most patients’ medical charts serum level of SGPT, SGOT, total cholesterol, triglyceride, HDL, LDL, albumin, fasting blood sugar, insulin assay and hepatitis profile were documented. The Body Mass Index (BMI) was calculated as body weight in Kg/ (height in meter)2, where as the BMI is more than ≥25 Kg/m2 in obese patient and its ≥23 Kg/m2 in overweight patients.24 (Appendix B) Insulin resistance was computed using the Homeostatic Model Assessment index (HOMA).25 A single investigator obtained all these data. IR= Insulin assay ( microunits/ml) x FBS (mmol/ml) 22.5 The HOMA has been used extensively as a reliable marker measuring insulin resistance among patients diabetes mellitus and normal subjects. This has been proven by studies made by Lansang26 and Bonora27 both of which compared HOMA with the more complex glucose clamp technique and conducted that HOMA can be used reliably as a less expensive alternative for measuring insulin resistance. A HOMA-IR value of 2.77 was chosen as the threshold for insulin resistance based on the Bruneck Study. Exclusion criteria for the study included: primary liver disorders other than fatty liver disease that could account for steatosis including hepatitis B and C, alcohol intake of > 20 grams/day, history of jaundice for past six months, previous intake of steatogenic drugs such as amiodarone, estrogen, chemotherapeutic drugs and anti-koch’s medications. Other subjects who were excluded in the study are patients who were pregnant, with CHF (NYHA class III), with COPD, with history of sepsis and parenteral nutrition. Metabolic syndrome also known as Syndrome X was diagnosed according to the new National Cholesterol Education Program Adult Treatment Panel III (NECP ATP III) report which is 3 or more of the following is present will satisfy the diagnosis: Hypertension (BP130/85 mmHg), Fasting blood glucose (110-125mg/dl or 6.1mmol/L), Hypertriglyceridemia (150 mg/dl), Low HDL-C ( < 40 mg/dl for men and < 50 mg/dl for women), Abdominal obesity (waist circumference of >102cm for men and >88cm for women).28 V- Data Analysis: Data were expressed as meansSD using Students t test and Chi-square test for statistical analysis. All data was encoded and presented using the Statistical Package for Social Sciences (SPSS) version 10. Prevalence of metabolic syndrome will be calculated using the traditional formula: Prevalence = number of patients w/ 3 risk factor Total population X 100 VI- Results: A total of 256 patients with fatty liver findings on ultrasound were selected for the study, in which only 180 charts were available for reviewed. Out of 180 subjects 71 of which were excluded due to 52 of them were alcoholic and 19 of them had history of exposure to what was mentioned in the exclusion criteria. Only a total of 109 patients were enrolled in the study. The mean age of the entire subject population was 47.815.6 with 70 were male (64.2%) and 39 were female (35.7%) with male to female ratio of 1:1.7 (Table 1). The age distribution of study patients is given in Figure 1. Figure 1. Age distribution of study patients 30.0 25.0 Percent 20.0 15.0 10.0 5.0 0.0 15.0 25.0 35.0 45.0 55.0 65.0 75.0 85.0 Age range Laboratory Results: The mean SGPT level was 68.756.05, SGOT level was 34.9115.28. The values of cholesterol above normal range were present in 18 subjects (40.9%) and subjects with elevated triglyceride were 71 (69.6%). The mean cholesterol and triglyceride level were 190.4735.04 and 180.5865.52 respectively. The association of hypercholesterolemia and hypertriglyceridemia in this study were strongly correlated to the incidence of patients with non alcoholic fatty liver. The serum HDL which is below the normal range was noted in 33 subjects (35.48%). The mean serum HDL was 49.5011.0. The laboratory data of the study population were given in Table 2. Insulin assay was done in 19 subjects (17.43%) in which insulin resistance were noted in 16 subjects (84%) with non alcoholic fatty liver by ultrasound. The mean insulin assay was 14.816.36. Table 1: Demographic and Clinical characteristics of patients with Nonalcoholic Fatty Liver Characteristics Age BMI Gender Male Female Diabetics Hypertensive n 109 106 109 109 109 Percent 70(64.2%) 39(35.7%) 52(47.7%) 72(66.1%) MeanSD 47.815.61 28.353.19 Median 48 28.71 Range 23-86 18.83-34.99 Table 2: Laboratory Data of patients with Nonalcoholic Fatty Liver Laboratory Test n MeanSD Median Range SGPT SGOT Cholesterol Triglycerides HDL FBS Insulin assay 108 42 45 102 93 106 19 68.7056.05 34.9115.28 190.4735.04 180.5862.52 49.511.0 129.8349.73 14.816.36 50.6 32.9 190.33 185.22 48 114.88 13.5 17-363.9 12.5-78 121.7-265 49.4-361 28.18-81.3 77.9-373 3.7-33.8 SGPT= 7-41 U/L SGOT= 10-37 U/L Cholesterol = 40-200 mg/dL Triglycerides= 52-201.75 mg/dL HDL=35-65 mg/dL FBS= 110-125mg/dL Insulin assay= < 7.1 microunits/ml Clinical Conditions: Obesity was the most prevalent predictor in our study group which was present in 93 of 106 subjects (85.32%). The BMI distribution is given in figure 2. The mean BMI was 28.353.19 Kg/m.2The mean BMI in males was 28.323.33, and in females it was 28.402.96 (p<0.9 between males and females). No significant difference in BMI was noted between male and female population. Hypertension was present. 66.1% (72/109) in our study group. Diabetes was also an important risk factor associated in non alcoholic fatty liver which is present in 47.7% (52/109) of our subjects. The characteristic of the study group is given in Table 1. Insulin resistance was also noted as an additional for the development of non alcoholic fatty liver which was detected in 16 out of 19 patients (84%) using the HOMA-IR index. The prevalence of metabolic syndrome among patients with NAFLD is at 51% (56/109) of the total study population. Figure 2: BMI distribution of patients with NAFLD 7% 6% obese overwt normal 87% VII- Discusssion: Our data from 109 patients with non-alcoholic fatty liver disease had clinical features compatib le with the metabolic syndrome. This includes obesity (85.32%), hypertension (66.1%), diabetes (47.7%), hypertriglyceridemia (69.6%) and low HDL-C (35.48%). It was noted in 51% (56/109) of our study group had at least 3 or more of the clinical feature suggestive of metabolic syndrome. Obesity was easily accompanied with fatty liver,29 it is a very common phenomenon in the developed countries. 60-100% patients of nonalcoholic steatohepatitis (NASH) were prove to have obesity.30 Hypertension can also be an independent risk factor in patients with NAFLD, Donati et al31 showed that there is a higher prevalence of NAFLD in non-obese hypertensive. Type 2 diabetes mellitus usually accompanied insulin resistance. 32,33 Both peripheral and hepatic insulin resistance were present in almost all patient with nonalcoholic fatty liver disease, irrespective of the coexistence of related risk factors.32 Above findings, together with the associated hyperlipidemia, obesity and hypertension, were considered as the manifestation of the metabolic syndrome that was associated with insulin resistance.33 Insulin resistance was also noted in 16 out of 19 subjects (84%), recent studies have pointed to hyperinsulinemia and insulin resistance as pathogenic factors in NAFLD. Marchesini et al34 showed that insulin resistance was the laboratory finding most closely associated with the presence of NAFLD in a large series of patients, irrespective of BMI, fat distribution or glucose tolerance. In this study, either type 2 diabetes or elevation of fasting blood glucose was related to fatty liver. It only suggested that insulin resistance might be a risk factor for fatty liver and metabolic syndrome, since there is only small sample size was used. Accordingly NAFLD represent another feature of metabolic syndrome. 35 Since patients with this syndrome have a 30% increased risk of cardiovascular death in the absence of type 2 DM and a 40-70% increased risk of cardiovascular death in the presence of type 2 DM, 36 patients with the metabolic syndrome require the treatment of the syndrome regardless of the severity of any associated non-alcoholic fatty liver disease. However non-alcoholic fatty liver disease may be an independent disease but more generally it is a lesion of the liver in certain systemic diseases and can progress from mild steatohepatitis to severe fibrosis and cirrhosis. 10 Although the etiology of non-alcoholic steatohepatitis is explained extensively. The complicated and multifactor pathogenesis made it remain poorly understood. Several of the recognized associated conditions such as intestinal by pass surgery, steroid treatment and total parenteral nutrition, can cause a metabolic shift favoring lipogenesis rather than lipolysis and lead to steatosis. 30 Recently, a ‘two-hit’ hypothesis for the development of nonalcoholic steatohepatitis has been proposed. The first hit was insulin resistance which produces steatosis, the second, any source of oxidative stress that increase the lipid peroxidation and subsequently leads to increased liver damage.37 Factors which can produce a ‘second hit’ such as alcohol, and drugs were conspicuously absent in our study group. At present there is no established therapy for NAFLD based on evidence from large, RCT’s. Treatment for all patients whatever the severity of their disease, should therefore be directed at the associated metabolic syndrome risk factors: obesity, type 2 DM, dyslipidemia and hypertension. This strategy will reduce morbidity and mortality and may also be beneficial to the liver.38 VIII- Conclusion: The preliminary data presented in the study showed prevalence of metabolic syndrome among patients with NAFLD at 51% (56/109) of the study group. The factors associated with metabolic syndrome among patients with NAFLD includes: obesity, hypertension, diabetes, hypertriglyceridemia and low HDL-C. IX- Recommendation: The researcher/s further recommends comparing the study group to a control. A follow up research using a prospective study design should be done to the subjects giving emphasis to the insulin resistance, in which the researcher/s failed to use a bigger sample size. VIII- References: 1. Angulo P., Non-alcoholic Fatty Liver Disease. N Engl J. Med 2002; 346: 1221-1231 2. Lonardo A., Fatty Liver and Non-alcoholic Steatohepatitis. Where do we stand and where are we going? Dig Dis Sci 1999; 17:80-89 3. Leevy CM; Fatty Liver: A study of 270 patients with biopsy proven fatty liver and review of literature, Medicine 41: 249-276, 1982 4. Ludwig J, Viaggiano TR, McGill DB, Oh BJ; Non-alcoholic Steatohepatitis; Mayo Clinic experience with a hitherto unnamed disease. Mayo Clinic Proc 1980; 55: 434-438 5. Al-quorain A., Jatti MB, Al-hamdan AR, Al-gindan Y, Ibrahim E, Khatib R et al. Pattern of Chronic Liver Disease in the Eastern province of Saudi Arabia. A hospital based clinicopathological study. Trop Georg Med 1994;46:358-364 6. Wanless IR, Lentz JS; Fatty Liver Hepatitis (Steatohepatitis) and Obesity an autopsy study with analysis of risk factors. Hepatology 12: 1106-1110, 1990 7. Eriksson S, Eriksson KF, Bondessol; Non-alcoholic Steatohepatitis in Obesity; A reversible condition. Acto Med Scand. 220:83-86, 1988 8. Powell EE, Cooksley WG, Hanson R, Searle J, Halliday JW, Powell LW; The natural history of non-alcoholic steatohepatitis. A follow-up study of forty-two patients for up to 21 years. Hepatology 11: 74-80, 1990 9. Lee RG: Non-alcoholic Steatohepatitis: A study of 49 patients. Hum Pathol 20:549598,1994 10. Bacon BR, Farahvash MJ, Janney CG, Neuschwander-Tetri BA: Non-alcoholic steatohepatitis: an expanded clinical entity. Gastroenterology 107:1103-1109,1994 11. Itoh S, Yougel T, Kawagoe K, Comparison between non-alcoholic steatohepatitis and alcoholic hepatitis. Am J Gastroenterol 82:650-654,1987 12. Diel AM, Goodman Z, Ishak KG, Alcolic disease in nonalcoholics: a clinical and hitologic comparison with alcohol induced liver injury. Gastroenterology 95:1056-1062,1988 13. Tominaga K, Kurata JH, Chen YK, Fujimoto E, Miyagawa S, Abe I, Kusano Y. Prevalence of fatty liver in Japanese children and relationship to obesity. An Epidemiological ultrasonographic survey. Dig Dis Sci 1995; 40: 2002-2009 14. Yano E, Tagawa K, Yamaoka K, Mori M. Test validity of periodic liver function test in a population of Japanese male bank employees. J Clin Epidemiol 2001;54:945-951 15. Matteoni CA,Younossi ZM, Gramlich T, Boparai N, Liu YC, McCullough AJ. Nonalcoholic fatty liver disease:a spectrum of clinical and pathological severity. Gastroenterology 1999;116: 1413-1419. 16. Araujo LM, De Oliveira DA, Nunes DS. Liver and biliary ultrasonography in diabetes and non-diabetic obese women. Diabetes Metab 1998;24:458-462 17. Bellentani S, Saccoccio G, Masutti F, Croce LS, Brandi G, Sasso F, Critanini G, Tiribelli C. Prevalence of and risk factors foe hepatic steatosis in Nothern Italy. Ann Int Med 2000;132:112-117 18. el-Hassan AY, Ibrahim EM, al-Mulhim FA, Nabhan AA, Chammas MY. Fatty infiltration of the liver: analysis of prevalence, radiological and clinical features and influence on patients management. Br J Radiol 1992;65:774-778 19. Collantes R, Ong J, Younossi Z, Nonalcoholic fatty liver disease and the epidemic of obesity. Clev Clin J of Med 2004;71:657-664 20. Chen QK, Chen HY, Huang KH, Zhong YQ et al. Clinical features and risk factors of patients with fatty liver in Guangzhou area.World J Gastroenterol 2004,10(6):899-902 21. Joseph AE, Saverymuttu SH, al-Sam S, Cook MG, Maxwell JD. Comparison of liver histology with ultrasonography in assessing difuse parenchymal liver disease. Clin Radiol 1991;43:26-31 22. Hulcraniz R, Gabrielson N. Patients with Persistent elevation of aminotranferases: Investigation with ultrasonography, radionuclide imaging and liver biopsy. J of Int Med 1993;233:7-12 23. Mendler MH, Bouillet P, LeSidaner A, Lavoine E, Labrousse F, Sautereau D. Pillegand B. Dual energy CT in the diagnosis aand quantification of fatty liver: Limitted clinical value in comparison to ultrasound scan and single energy CT, with special reference to iron overload. J of Hepatology 1998;28:785-794 24. The Asia pacific Perspective Obesity and its Treatment WHO/Western Pacific Region IASO-International Association for the Study of Obesity 2004 25. Bonora E.,Kiechl S., Willeit J., Oberhollenzer F., Egger G., Targher G., Alberiche M., Bonadonna RC., Muggeo M. Prevalence of Insulin Resistance in Metabolic Disorders: The Bruneck Study. Diabetes 47 (10):1643-9, Oct. 1998. 26. Lansang MC, Williams GH, Caroll JS. Correlation between the Glucose Clamp technique and the Homeostatic Mode Assessment in Hypertention. Am J of Hypertension 14(1):513, 2001 Jan 27. Bonora E, Targher G, Alberiche M, Bonadonna RC, Saggiani F, Zenere MB, Monauni T et al. Homeostatic model assessment closely mirrors the glucose clamp technique in the assessment of insulin sensitivity: studies in subjects with various degrees of glucose tolerance and insulin sensitivity. Diabetes Care 2000;23:57-63. 28. Grundy S, Brewer H, Cleeman J, Smith S, Lenfant C. Definitipon of Metabolic Syndrome. Circulation 109(2004),433-438. 29. Gray DS. Diagnosis and prevalence of obesity. Med Clin North Am 1989;73:1-13. 30. Sheth SG, Gordon FD, Chopra S. Nonalcoholic Steatohepatitis. Ann Intern Med 1997; 126:137-45. 31. Donati G, Stagni B, Piscaglia F, Venturoli N, Morselli-Labate AM, Rasciti L, Bolondi L. Increased prevalence of fatty liver in arterial hypertensive patients with normal liver enzymes: role of insulin resistance. Gut 2004;53:1020-1023. 32. Marceau P, Biron S, Hould FS, Marceau S, Simard S, Thung SN, Kral Jg. Liver pathology and the metabolic syndrome X in severe obesity. J Clin Endocrinol Metab 1999;84:15131517. 33. Marchesini G, Brizi M, Bianchi G, Tomassetti S, Bugianesi E, Lenzi M, McCullough AJ, Natale, Forlani G, Melchinda N. Nonalcoholic fatty liver disease: a feature of the metabolic syndrome. Diabetes 2001;50:1844-1850. 34. Marchesini G. Brizi M, Morselli Labate AM, Bianchi G, Bugianesi G, McCullough AJ, Forlani G, Melchionda N. Association of nonalcoholic fatty liver disease to insulin resistance. Am J Med 107:450-455, 1999. 35. Cortez-Pinto H, Camilo ME, Baptista A, De Oliveria AG, De Moura MC. Nonalcoholic fatty liver: another feature of the metabolic syndrome? Clin Nut 18:353-358,1999. 36. Isomaa B., Almgren J., Tuoni T. et al. Cardiovascular Morbidity and mortality associated with the metabolic disorders. Diabetes Care 2001; 24:683-9. 37. Day CP, James OFW. Steatohepatitis: A tale of two hits? Gastroenterology 1998;114:842-5 38. Day CP. Non-alcoholic fatty liver disease. Gastroenterology 2004; 26:393-403 Appendix A: Components of the Metabolic Syndrome (NCEP ATP III recommendations) Components Defining level Fasting Glucose > 110 mg/dl or 6.1mmol/L Hypertension ≥130/≥85 mmHg Abdominal Obesity (waist circumference) Men > 102 cm or > 40 inches Women > 88 cm or >35 inches Triglyceride ≥ 150 mg/dL or ≥ 1.7 mmol/L HDL-C Men < 40 mg/dL or < 1.0 mmol/L Women < 50 mg/dL or < 1.2 mmol/L Metabolic syndrome is defined by the presence of 3 or more these features APPENDIX B: Body Mass Index (BMI) wt. in Kg/ ht. in m2 ____________________________________________________________ Classification BMI score ____________________________________________________________ Underweight < 18.5 Normal 18.56 – 22.99 Overweight 23- 24.99 Obese 1 25 – 29.99 Obese 2 > 30 ____________________________________________________________ The Asia pacific Perspective Obesity and its Treatment WHO Western Pacific Region-International Association for the Study of Obesity 2004 APPENDIX C Data Collection Form: Ultrasound Findings of Fatty Liver among Non- Alcoholic Metabolic Syndrome Patients Date ______________ Name_________________________________ A. Vital signs: BP: ___________ Subject No.__________________ Age/Sex_____________________ CR: ________ RR: __________ B. History: Alcohol Drinking >2 bottle of beer/day >200ml of wine/day >50ml of 80% proof Yes ( ) ( ) ( ) ( ) No ( ) ( ) ( ) ( ) Yes Pregnant ( ) On parenteral nutrition ( ) COPD ( ) Congestive heart failure ( ) History of : Jaundice Hepatitis B Hepatitis C Hypertension ( ( ( ( ( ( ( ( Sepsis Renal Failure Bowel surgery Diabetes ( ( ( ( ) ) ) ) ( ( ( ( ) ) ) ) Anti-Koch’s Anti-Neoplastic ( ( ) ) ( ( ) ) ) ) ) ) ) ) ) ) Intake/use of the following medication/s: Amiodarone ( ) ( ) Estrogen ( ) ( ) No ( ) ( ) ( ) ( ) C. Anthropometric Measurements: Weight: (kg) _______ Height: (m) ________ Abdominal Circumference: (cm) ___________ Hip-Waist Ratio: _______________________ BMI: __________ Hip Circumference: (cm) ______________ D. Laboratory Results: FBS_________ HDL __________ SGPT______ ___U/L HBs Ag _______ Total Cholesterol___________ Triglyceride _________ LDL ___________ SGOT_______ __U/L Serum Albumin________ HCV Ab _______ E. Ultrasound of the Liver result: