Continuous Nebulized Brochodilator (CNB) Therapy on the General
advertisement
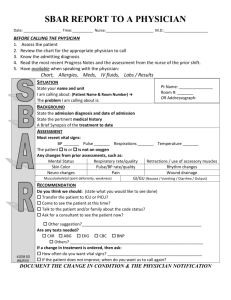
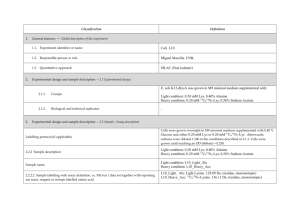
Guidelines for Continuous Nebulized Bronchodilator (CNB) Therapy on the Children’s Hospital Floors Policy: The purpose of this policy is to ensure the safe delivery of Continuous Nebulized Bronchodilator therapy to asthmatics outside the emergency department and critical care setting. Any patient determined to be unstable or outside the parameters listed below will need to receive the CNB in the emergency department, the Pediatric Intensive Care unit, or an intermediate unit. CNB therapy on the floors will be given on 7E or 7A. Asthmatic patients on 7B or 7C will need to be transferred to an area where CNB therapy is allowed. If a patient on 7B or 7C is in need of CNB therapy and there are no beds available in the areas CNB therapy is given, therapy will be initiated as plans are made to transfer the patient as soon as possible. In the case of a patient with significant co-morbid illness requiring CNB therapy, arrangements should be made to transfer the patient to the PICU. Patients requiring ongoing CNB therapy from the MUSC Pediatric Emergency Department will be transferred directly to the PICU or an intermediate unit. Patients who have received multiple CNB therapies in the emergency department should be monitored closely prior to transfer to the floor. They should be observed in the Peds ED until their treatments can be spaced to every two hours or deemed appropriate and stable for the floor by the Peds ED attending physician. Ideally patients should have a BAN treatment prior to transfer to the floor where delays can occur in patients receiving the next treatment. This does not apply to patients who did not require multiple CNB therapies in the Peds ED. The PICU attending physician, charge nurse, respiratory therapist, and HSC (at night) will be notified of patients placed on CNB therapy for the initial treatment and the second treatment (if given) on 7E or 7A in order to prepare the area for the possibility of the need for admission to the unit within the next 3-4 hours. After two CNB treatments, if the floor resident determines that a patient cannot be spaced to treatments every two hours, the PICU attending or upper level resident will go assess the patient and determine the need for a higher level of care. If the child is to remain on the floor, the inpatient team will determine the need for further CNB treatments. Residents caring for patients on CNB therapy on 7E or 7A will need to assess the patient after the first CNB treatment to determine what treatment regimen is necessary. A new order for therapy will need to be written following the patient assessment. The Respiratory Therapy clinical coordinator will be notified of every patient being placed on CNB therapy on the floors. The coordinator will evaluate the patient early in the treatment regimen and regularly throughout CNB therapy. Instances where a patient is in need of CNB therapy but does not meet floor criteria and there is no bed availability in the ICU will be handled on an individual basis with discussion between the nurse manager/HSC, respiratory clinical coordinator, floor physician and the PICU physician. CNB therapy will be started as the team decides the best way to ensure the patient receives appropriate, well monitored care. Upon transfer of a patient on the floor to the ICU or intermediate care unit, report should take place between the resident and PICU or intermediate care unit physician, the floor charge nurse and unit charge nurse, and the floor therapist and unit therapist. Patients on CNB therapy on the floor will need to be placed on a pulse oximeter. Patient Criteria: 1. 2. 3. 4. Age: > 36 months Clinical asthma score : < 6 FIO2: < .50 Oxygen Saturation: > 90% Revised: 7/1/10