the expertise covered in your centre
advertisement
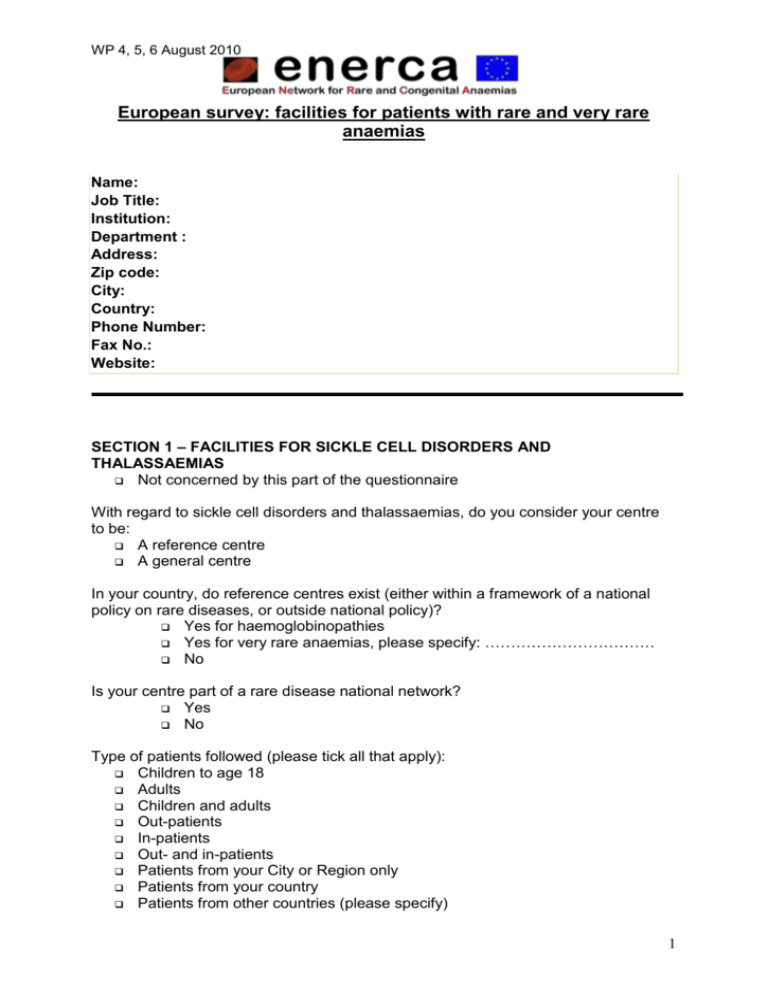
WP 4, 5, 6 August 2010 European survey: facilities for patients with rare and very rare anaemias Name: Job Title: Institution: Department : Address: Zip code: City: Country: Phone Number: Fax No.: Website: SECTION 1 – FACILITIES FOR SICKLE CELL DISORDERS AND THALASSAEMIAS Not concerned by this part of the questionnaire With regard to sickle cell disorders and thalassaemias, do you consider your centre to be: A reference centre A general centre In your country, do reference centres exist (either within a framework of a national policy on rare diseases, or outside national policy)? Yes for haemoglobinopathies Yes for very rare anaemias, please specify: …………………………… No Is your centre part of a rare disease national network? Yes No Type of patients followed (please tick all that apply): Children to age 18 Adults Children and adults Out-patients In-patients Out- and in-patients Patients from your City or Region only Patients from your country Patients from other countries (please specify) 1 WP 4, 5, 6 August 2010 Clinic: Average number of patients followed annually: children ______ / year adults ______ / year Total Registered patients: Sickle Cell Syndromes: ___________________ Thalassaemia Syndromes: ________________ Diagnosis centres: Average number of specimen received: For care For advice ______ / year ______ / year (confirmation or final diagnosis after first line tests obtained in another centre) Phenotype Genotype ______ / year ______ / year THE EXPERTISE COVERED IN YOUR CENTRE (Please tick all that apply) The areas of expertise not covered in our centre are available in other expert centres A close collaboration exists with those centres No collaboration exists with other centres 1. Diagnosis – prevention Phenotypic diagnosis of Haemoglobin Disorders Genotypic diagnosis of Haemoglobin Disorders Neonatal screening Local National Antenatal screening Pre-marital screening Local National Genetic counselling Pre-natal diagnosis Pre-implantation diagnosis Participation to an external quality control (QC) o Phenotype, name of the external QC: ………………………………. o Genotype, name of the external QC: ………………………………. 2. Follow-up/case management Acute events - Special services in your centre Does the centre have staff with specific expertise in dealing with acute events of Haemoglobin disorders (e.g. pain control, stroke)? 2 WP 4, 5, 6 August 2010 Yes No Allocated beds: Day unit Hospital Day unit and hospital Trained, dedicated staff: Nurses Medical doctors Psychologist Neurosurgical unit Imaging staff Blood transfusions: Do you perform an extended immuno-phenotype (beyond ABO and D)? Yes No Do you have access to donor red blood cell units with rare phenotypes Yes No Do you have: Access to exchange blood transfusion (trained staff) 24-hour service 3. Follow-up/case management Chronic events – special services in your centre Does the centre have staff experienced in monitoring, preventing and dealing with chronic complications of Haemoglobin disorders? Yes No Please tick the areas of case monitoring/follow-up that are offered by your centre (for early/timely detection of the following): Chronic pain Stroke (prevention), please give an example _____________________ Stroke (care) Leg ulcer Osteonecrosis Bone disease (e.g. osteoporosis) Chronic renal disease Pulmonary disease please give an example _____________________ Cardiac disease Eye complications Hearing complications Liver complications Growth 3 WP 4, 5, 6 August 2010 Endocrine complications Pregnancy Contraception - fertility Iron overload please give an example……………………………………… Psychological support Are patients monitored by specialists in: Cardiology? Liver disorders? Endocrinology? Other? (please specify)……………………………………………………… CRITERIA OF EXPERTISE IN YOUR CENTRE 1. Availability of specialised services, able to deal with SCD/thalassaemia complications (please tick all that apply): Intensive care unit Trained in sickle-related organ damage and multiple organ damage Transcranial echo-doppler MRI Angio MRI CT Angiofluorography Audiometry Assessment of cardiac iron by T2* MRI Measurement of liver iron concentration: Biopsy MRI SQUID 2. Availability of treatments: Stem cell transplantation Hydroxyurea Iron chelation Transfusions With rare blood phenotype Blood bank Exchange transfusion Automated Manual 3. Availability of patient services: Psychology services Link with education services (i.e. coordinating with school for educational problems) Link with other social services (e.g. employment, social security) 4 WP 4, 5, 6 August 2010 Link with patients’ associations 4. Availability of decision support (guidelines) Available electronically for patients Available electronically for health professionals Available in booklet form for patients Available in booklet form for health professionals Standard follow-up of patients with very rare anaemias Children Adults Management of chronic pain Management of chronic complications Acute blood transfusions management Chronic blood transfusions management Management of pregnancy Pre- and peri-operative surgery management Criteria for hospitalisation Diagnosis of complications Treatment of complications Pain management 5. Availability of registries: Epidemiological surveillance Long term follow up for clinical care and decision making Collection of material for research and teaching Clinical research 6. Link with research: Yes Occasional No 7. High level of expertise and experience documented: Through publications Grants Teaching and training activities 5 WP 4, 5, 6 August 2010 SECTION 2 – FACILITIES FOR VERY RARE ANAEMIAS: Not concerned by this part of the questionnaire Or by: Red blood cell membrane disorders Red blood cell enzyme disorders Congenital Dyserythropoietic Anaemia (CDA) Diamond Blackfan Anaemia (DBA) Paroxysmal Nocturnal Haemoglobinuria (PNH) Hereditary Sideroblastic Anaemia (HSA) Very rare anemias due to defective iron utilization With regard to very rare anaemias, do you consider your centre to be: A reference centre A general centre In your country, do reference centres exist (either within a framework of a national policy on rare diseases, or outside national policy)? Yes No Is your centre part of a rare disease national network? Yes No Type of patients followed (please tick all that apply): Children to age 18 Adults Children and adults Out-patients In-patients Out- and in-patients Patients from your City or Region only Patients from your country Patients from other countries (please specify) Clinic: Average number of patients followed annually: children ______ / year adults ______ / year Total registered patients with: Red blood cell membrane disorders: ________________ Red blood cell enzyme disorders: ________________ CDA: ________________ DBA: ________________ PNH: ________________ HSA: ________________ Very rare anemias due to defective iron utilization: ________________ Other Anaemias (please specifiy): ________________________ 6 WP 4, 5, 6 August 2010 Diagnosis centres: Average number of specimen received: For care For advice ______ / year ______ / year (confirmation or final diagnosis after first line tests obtained in another centre) Phenotype Genotype ______ / year ______ / year THE EXPERTISE COVERED IN YOUR CENTRE (Please tick all that apply) The areas of expertise not covered in our centre are available in other expert centres A close collaboration exists with those centres No collaboration exists with other centres 4. Diagnosis – prevention Genetic counselling, please specify…………………………………………… Pre-natal diagnosis, please specify…………………………………………… Pre-implantation diagnosis, please specify………………………………….. Participation to an external quality control (QC) o Phenotype, name of the external QC: ………………………………. o Genotype, name of the external QC: ………………………………. 5. Follow-up/case management Acute events - Special services in your centre Does the centre have staff with specific expertise in dealing with acute events of very rare anaemias (e.g. consequences of iron overload, hemolytic crises, aplastic crises)? Yes No Allocated beds: Day unit Hospital Day unit and hospital Trained, dedicated staff: Nurses Medical doctors Psychologist Imaging staff 7 WP 4, 5, 6 August 2010 Blood transfusions: Do you perform an extended immuno-phenotype (beyond ABO and D)? Yes No Do you have access to donor red blood cell units with rare phenotypes Yes No Do you have: Access to exchange blood transfusion (trained staff) 24-hour service 6. Follow-up/case management Chronic events – special services in your centre Does the centre have staff experienced in monitoring, preventing and dealing with chronic complications of very rare anaemias? Yes No Please tick the areas of case monitoring/follow-up that are offered by your centre: Leg ulcer Osteonecrosis Bone disease (e.g. osteoporosis) Chronic renal disease Pulmonary disease Cardiac disease Eye complications Hearing complications Liver complications Growth Endocrine complications Pregnancy Contraception - fertility Iron overload, please give an example…………………………………… Psychological support Other, please specify Are patients monitored by specialists in: Cardiology? Liver disorders? Endocrinology? Other? (please specify) ……………………………………………………… 8 WP 4, 5, 6 August 2010 CRITERIA OF EXPERTISE IN YOUR CENTRE 8. Availability of specialised services, able to deal with complications of very rare anaemias (please tick all that apply): Intensive care unit MRI CT Audiometry Assessment of cardiac iron by T2* MRI Measurement of liver iron concentration: Biopsy MRI SQUID 9. Availability of treatments: Stem cell transplantation Iron chelation Phlebotomy Transfusions With rare blood phenotype Exchange transfusion Automated Manual 10. Availability of patient services: Psychology services Link with education services (i.e. coordinating with school for educational problems) Link with other social services (e.g. employment, social security) Link with patients’ associations 11. Availability of decision support (guidelines) Available electronically for patients Available electronically for health professionals Available in booklet form for patients Available in booklet form for health professionals Standard follow-up of patients with very rare anaemias Children Adults Management of chronic pain Management of chronic complications Acute blood transfusions management Chronic blood transfusions management Management of pregnancy Pre- and peri-operative surgery management Criteria for hospitalisation Diagnosis of complications Treatment of complications 9 WP 4, 5, 6 August 2010 Pain management Pre- and peri-operative surgery management 12. Availability of registries: Epidemiological surveillance Long term follow up for clinical care and decision making Collection of material for research and teaching Clinical research 13. Link with research: Yes Occasional No 14. High level of expertise and experience documented: Through publications Grants Teaching and training activities 15. Free additional comments: Thank you very much for your collaboration 10 WP 4, 5, 6 August 2010 The completed questionnaire can be returned by mail, e-mail, or fax, to either directly to ENERCA via Prof Gulbis or to Dr Percy (UK contact person) Prof Béatrice Gulbis, MD PhD Head, Department of Clinical Laboratories Hôpital Erasme -U.L.B. Route de Lennik 808 B- 1070 Brussels Tel +32 2 555 34 28 Fax +32 2 555 66 55 E-mail: Beatrice.Gulbis@erasme.ulb.ac.be Dr Melanie J Percy, PhD, FRCPath, Department of Haematology, C Floor, Tower Block, Belfast City Hospital, Lisburn Road, Belfast BT9 7AB, Northern Ireland, UK Tel: + 44 (0)28-9026-3097 or 9026-3225 Fax: + 44 (0)28-9026-3870 Email: melanie.percy@belfasttrust.hscni.net 11