medical history questionaire - Coffee Regional Medical Center
advertisement

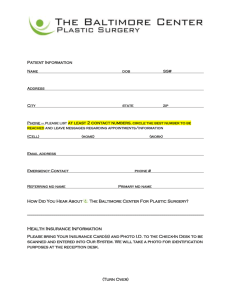
MEDICAL HISTORY QUESTIONAIRE Name: DOB: Date: What is your occupation? What are your concerns for today’s visit? Please answer the following to the best to your ability. 1. 2. 3. What is your gender? Male Female How is your health? Good Fair Do you have any ALLERGIES to any medications? _____Yes or If so, please list below and reaction: 4. Do you smoke or have you ever smoked? Yes or ______No If so, how many? Have you ever been treated for any of the following LUNG PROBLEMS? Asthma Chronic Cough Tuberculosis Wheezing Emphysema Shortness of breath Chronic Bronchitis Recent Pneumonia Coughing up blood Have you ever been treated for any of the following HEART PROBLEMS? Chest pain or Angina Heart Murmur Rheumatic Fever Stroke Shortness of breath High blood pressure Low blood pressure Heart attack Heart failure Leg swelling Palpitations of fainting Have you ever had or been treated for MUSCLE, BONE OR JOINT PROBLEMS? Arthritis Muscle Weakness Neck problems Cramps or spasms Trouble opening mouth Have you ever had or been treated for SKIN DISORDERS? Eczema Psoriasis Skin Cancer Have you ever had or been treated for DIGESTIVE TRACT PROBLEMS? Ulcer disease Hiatal hernia Cirrhosis Gastritis Hepatitis Pancreatitis Chronic indigestion Liver problems Yellow jaundice Have you ever had KIDNEY PROBLEMS, KIDNEY FAILURE, or ARE ON DIALYSIS? Yes or Have you ever had or been treated for PROLONGED OR UNUSUAL OR EASY BRUISING? _____ Yes or Family history of: Bleeding problems or hemophilia Sickle cell anemia or trait Have you ever had or been treated for PSYCHIATRIC PROBLEMS? _____ Anxiety _____ Depression _____ Panic Attacks _____ Other Issues Have you ever had or been treated for METABOLIC OR ENDOCRINE PROBLEMS? _____Low blood sugar _____Thyroid Disease _____Diabetes mellitus _____Porphyria Have you ever had or been treated for ALLERGY and/or INMUNOLOGY? _____Nasal Allergies _____Currently on allergy shots _____Skin allergies _____HIV/AIDS Have you ever had or been treated for NEUROLOGIC PROBLEMS? Convulsions/seizures/fits/epilepsy Numbness/tingling/pain in arms/legs Low back pain sciatica Fibromyalgia 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. Poor No No No Patient Name: DOB: 17. Is there a FAMILY HISTORY of any of the following? Heart attack Diabetes Hepatitis Stroke Seizures Tuberculosis Thyroid disease High Blood Pressure Bleeding disorders Cancer (List): Asthma Hearing loss Stomach ulcer 18. FEMALES ONLY: Last menstrual period: Are you pregnant? Yes or No Are you planning to get pregnant? Yes or No 19. Do you currently take any MEDICATION? If so, please list all the Prescription and Over-the-Counter: 20. Which pharmacy to you use? Phone: 21. Have you ever had SURGERY? Please list below: Date: Operation: Complications: Date: Operation: Complications: Date: Operation: Complications: Date: Operation: Complications: 22. Have you ever had CANCER? Yes or No Date: Type: Date: Type: 23. Please provide the following medical information to the best of your ability. (Circle) **For “Yes” responses, please check “current” if this symptom relates to the reason for your visit today. Hearing Loss Dizziness Nasal Congestion Post nasal drip Hoarseness Throat clearing Difficulty swallowing Headache Fatigue Swollen Glands Depression Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes No No No No No No No No No No No Current Current Current Current Current Current Current Current Current Current Current Ear noise Ear pain Sinus pressure or pain Problem snoring, apnea Throat pain Cough Heartburn Weight loss or gain Daytime sleepiness Mental health problems FOR OFFICIAL USE ONLY Weight: BP Sitting Pulse: PRESENT ILLNESS: lbs / mm Hg Temp: Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes No No No No No No No No No No Current Current Current Current Current Current Current Current Current Current
![Pediatric Health Histroy.Initial child.d[...]](http://s3.studylib.net/store/data/006593866_1-7ecae25d724665d2a564380f86b41e96-300x300.png)