Table 1. Method of Contamination
advertisement

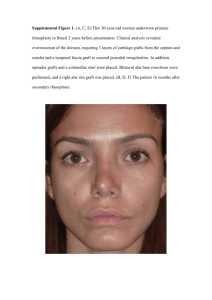
Management of the Contaminated Graft in Aesthetic Surgery Ankit R. Desai, MD, and Robert F. Centeno, MD INTRODUCTION: The use of autografts in aesthetic and reconstructive surgery has become a more common tool in a plastic surgeon’s arsenal. To date, the clinical experience, management, and outcome of graft contamination in plastic surgery have not been reported. On the basis of a literature review and a survey of plastic surgeons across the country, the authors propose an algorithm for the management of contaminated autografts in aesthetic surgery. METHODS: An internet link to a questionnaire was sent via email by the Aesthetic Surgery Education and Research Foundation (ASERF) to members of the American Society of Aesthetic Plastic Surgery. This anonymous survey was designed to obtain data on the frequency of autograft contamination, treatment preferences, clinical outcomes, and management of patient disclosure. RESULTS: A total of 223 surgeons responded to the online survey, a response rate of 12%. Of those responding, 87% were in practice for 10 or more years. A majority (70%) reported either witnessing or experiencing graft contamination during a plastic surgery procedure. Among the 156 surgeons with contamination experience, 27% reported a single occurrence, 33% reported 2 instances, 13% reported 3 occurrences, and 25% experienced 4 or more contaminated grafts. The methods of contamination are presented in Table 1. Grafts from the craniofacial region and lower extremity were the most commonly contaminated. The autograft most frequently contaminated was skin (97 instances) followed by cartilage. Table 1. Method of Contamination Exposure to nonsterile part of field/drape Exposure to nonsterile specimen container/suction cathetercanister/instrument Exposure to contaminated part of operating field (ear, nasopharynx, ano-rectal, GU) Graft/Flap fell on floor Graft/Flap discarded in trash Other # Occurrences 71 26 46 120 45 1 None of the respondants aborted a procedure after graft contamination occurred. Only one surgeon opted to use alloplastic material as a substitute. Eight surgeons harvested a graft from another site, and 3 employed an alternate reconstructive technique. However, all surgeons reported at least 1 instance in which the surgery was completed following graft decontamination. Only 3 of the 156 respondents with contamination experience reported a surgical site infection as an outcome of using a decontaminated graft. The extent of infections was not reported. These 3 clinical infections correlate to a complication rate of 1.9%, which is similar to clean non-contaminated cases.1 Sixty percent of surgeons who experienced graft contamination did not disclose the incident, and 24% made a notation in the chart only. However, 33 surgeons (20%) reported the contamination to the patient and/or family postoperatively. DISCUSSION: Inadvertent contamination of autografts poses a dilemma for the surgeon, but the medical literature provides little guidance on appropriate management of contaminated grafts. The most common decontamination agent used by survey respondents was povidone-iodine, followed closely by antibiotic solution. Several in vitro studies have demonstrated that fibroblasts are inhibited by povidone-iodine,2 including an investigation that found skin fibroblast growth to be completely inhibited by a concentration of 0.1%, which is only a tenth of the usual concentration.3 Consequently, alternative antiseptic solutions are recommended. Our literature review revealed that decontamination of bone and tendon grafts have received the most attention, with various antibiotic solutions, 10% povidone-iodine, and 4% chlorhexidine gluconate examined for decontamination effectiveness. In one study, 4% chlorhexidine gluconate had the greatest sterilization impact, with only 2% of grafts remaining culture positive after a 90 second soak.4 Other studies have found brief exposure to chlorhexidine to be safe for a variety of tissue types.5-7 Although decontamination with chlorhexidine gluconate is very effective, it has been found to be toxic to bone allografts and reduce osteoblast density and alkaline phosphatase activity.8 Because some antibiotic solutions are less toxic and provide comparable antisepsis,9 chlorhexidine should not be needed for bone decontamination. Instead, a combination antibiotic solution produces a similar reduction in bacterial counts with fewer cytotoxic effects.10 Regardless of the agent used, low-pressure lavage is preferred over soaks and high pressure lavage,9,11 which may cause decreased bone formation and less viable bone at fracture sites. Based on the limited data in the literature, we propose the algorithm presented in Figure 1 for graft contamination. As with most adverse events, the best solution is prevention, but the potential for graft contamination should be included in the written and verbal informed consent process. Prevention strategies should be implemented and discussed with all O.R. staff before autograft harvests. After harvest, the graft should be wrapped in saline-soaked gauze and placed in a labeled, sterile cup. The autograft also should be included in the surgical count process. In addition, tissue should not be discarded without confirmation from the surgeon. If an autograft does become contaminated, we propose decontamination of skin, cartilage, and composite tissue with 1 liter of low-pressure pulse lavage solution containing 4% chlorhexidine gluconate. Although no studies exist related to decontamination of fat grafts, the limited added morbidity from harvesting another fat graft should make decontamination unnecessary in most cases. For cancellous bone, we recommend re-harvesting, but cortico-cancellous bone may be decontaminated with 1 liter of low-pressure lavage using a triple antibiotic solution. Within our algorithm, we advocate disclosure to the patient. In addition, root cause analysis along with an incident report should be part of the postoperative process. With the assistance of the Quality Assessment and Assurance Committee, steps can be implemented to reduce the risk of future graft contaminations. REFERENCES 1 Culver DH, Horan TC, Gaynes RP, et al. Surgical wound infection rates by wound class, operative procedure, and patient risk index. National Nosocomial Infections Surveillance System. Am J Med 91(3B):152S-157S, 1991. 2 Lineaweaver W, Howard R, Soucy D, et. al. Topical antimicrobial toxicity. Arch Surg 120(3):267-270, 1985. 3 Balin AK, Pratt L. Dilute povidone-iodine solutions inhibit human skin bibroblast growth. Dermatol Surg 28(3):210-214, 2002. 4 Molina ME, Nonweiller DE, Evans JA, et. al. Contaminated anterior cruciate ligament grafts: the efficacy of 3 sterilization agents. Arthroscopy 16(4):387391, 2000. 5 Burd T, Conroy BP, Meyer SC, et. al. The effect of chlorhexidine irrigation solution on contaminated bone-tendon allografts. Amer J Sports Med 28:241-244, 2000. 6 Gunal I, Turgut A, Acar S, et. al. Effects of various irrigating solutions on articular cartilage. An experimental study in rabbits. Bull Hosp Jt Dis 59(2):73-75, 2000. 7 Reading AD, Rooney P, Taylor GJ. Quantitative assessment of the effect of 0.05% chlorhexidine on rat articular cartilage metabolism in vitro and in vivo. J Orthop Res 18(5):762-767, 2000. 8 Kaysinger KK, Nicholson NC, Ramp WK, et. al. Toxic effects of wound irrigation solutions on cultured tibiae and osteoblasts. J Orthop Trauma 9:303-311, 1995. 9 Bhandari M, Adili A, Schemitsch EH. The efficacy of low-pressure lavage with different irrigating solutions to remove adherent bacteria from bone. J Bone Joint Surg Am 83-A(3):412-419, 2001. 0 Hirn M, Laitinen M, Pirkkalainen S, et. al. Cefuroxime, rifampicin and pulse lavage in decontamination of allograft bone. J Hosp Infect 56:198-201, 2004. 1 Dirschl DR, Duff GP, Dahners LE, et. al. High pressure pulsatile lavage irrigatrion of intraarticular fractures: effects on fracture healing. J Orthop Trauma 29:187-190, 1998. Figure 1: Algorithm for Management of Contaminated Autografts AUTOGRAFT HARVEST [Pre-incident] Implement preventive strategies (process analysis) Informed consent Immediate placement of graft into labeled sterile cup in saline-soaked gauze Time Out Continuing education & process improvement Autograft implanted w/o complication AUTOGRAFT CONTAMINATED Yes REHARVEST (Fat/Dermal Grafts) Complete operation Obtain graft culture BONE Cancellous SKIN, CARTILAGE, & COMPOSITE TISSUE Corticocancellous REHARVEST Complete operation Low-pressure pulse lavage off sterile field with 1 L of triple antibiotic solution Confirm with surgeon prior to discarding any tissue POST-INCIDENT Can another autograft be harvested with minimal morbidity? No Incorporate into surgical count & during change of shift staff sign out Incident Report Submit to Quality Assessment & Assurance Committee Root Cause analysis Rinse with normal saline Disclosure to patient Low-pressure pulse lavage off sterile field with 1 L of 4% chlorhexidine gluconate Implement strategies to prevent recurrence and improve process