Why So Much Misdiagnosis with Hysterosalpingography
advertisement

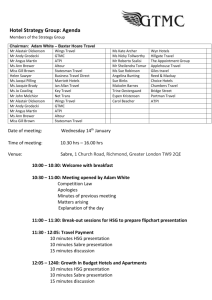
Common Causes of Misdiagnosis with Hysterosalpingography by Lousine Boyadzhyan, MPhil, and Alan DeCherney, MD UCLA Department of Obstetrics and Gynecology Box 951740, 27-139 CHS Los Angeles, CA 90095-1740 Introduction Hysterosalpingography (HSG) involves catheterization of the cervix to yield a watertight seal and injection of a contrast material under pressure in order to follow its flow path by obtaining radiographic images of the process. In this manner, one is able to appreciate morphology of the uterine cavity, lumina of the Fallopian tubes and, finally, tubal patency by visualizing peritoneal spillage of the contrast material.6,12,18,20 Many authors have questioned the validity of HSG, as rather wide ranges of negative and positive predictive values have been reported in the literature. Whereas reported negative predictive values range from 57.1 % to 92.0 %, positive predictive values range from 30.8 % to 84.5 %. 4,13, 14, 24 Therefore, there appear to be numerous cases of misdiagnosis with hysterosalpingography. Since HSG is felt by many experts to be invaluable at least in the initial diagnosis and treatment of patients in the field of infertility, its accurate interpretation is crucial for the infertility workup of any given female patient. Hysterosalpingography versus Other Diagnostic Modalities Many studies have been performed on comparing HSG and hysteroscopy (HSC), which is generally indicated for a thorough study of the uterine cavity interior.7,15 Whereas HSG is a good screening procedure for uterine abnormalities, HSC is used for confirmation and treatment of either abnormalities found on HSG or in those cases with normal HSG findings that had no improvement in fertility for at least 6 months. 15, 21, 25 In a recent prospective comparative study between HSG and HSC performed on 336 patients the most commonly misdiagnosed conditions were cervical stenosis as severe intrauterine adhesions, endometrial polyps as submucous myomas, and submucous myomas as endometrial polyps. 16 Similarly to how HSC has been compared to HSG in intrauterine defects, several authors have compared HSG with laparoscopy as the gold standard for tubal patency. A meta analysis of 20 studies between 1968 and 1994 led to the conclusion that while a negative HSG result will not rule out a disease, a positive HSG result is good at ruling in tubal obstruction.23 In fact, many experts investigate abnormal HSG tubal findings with laparoscopy or if no improvements in fertility are seen in six months after a normal HSG film.21, 23, 25 Technical Aspects Oil versus aqueous contrast media HSG films generated with oil-based contrast material have more contrast and sharpness to the image than their water-based contrast counterpart.22 In addition, oilbased media possesses a therapeutic benefit in infertile women.1,3 However, one is able to appreciate longitudinal rugations of the ampullary portion of the fallopian tubes indicative of normal tubal mucosa only when using a water-based and not an oil-based contrast.22 Even though no serious complications have been reported due to oil-media intravasation, one should be carefully monitoring their technique to avoid oil emboli. Common Technical Errors in Uterine Cavity Visualization After reviewing HSG films from 100 patients, Hofmann et al presented three reasons for inadequate visualization of the uterine cavity.10 The most common reason (82 %) was an axial view of the cavity as a result of inadequate traction on the cervix during the procedure. Other reasons for incomplete visualization of the uterine cavity were obscured views of the lower uterine cavity and endocervical canal due to obstruction of the lower uterine cavity by the bulb of the intrauterine catheter and obstruction of the endocervical canal by the vaginal speculum. In his review of HSG, Siegler commented on the danger of overfilling the uterine cavity with contrast material when attempting to evaluate the shape of the latter in search for submucous myomas, endometrial polyps, or synechiae.20 In fact, increasing amounts of contrast material can obscure the classic finding of a submucous myoma seen as a filling defect of a distorted, enlarged cavity (Fig. 1). Fig. 1 Submucous myoma, classically seen as a filling defect in a large uterine cavity. Technical Artifacts Some of the most common technical artifacts potentially leading to misdiagnosis on HSG films are air bubbles and venous or lymphatic intravasation.27 Incidental introduction of air bubbles into the uterine cavity may be falsely considered to be due to other filling defects such as polyps, blood clots, endometrial hyperplasia, or submucosal myomas.15,27 Often one sees a single or multiple air bubbles appearing as a well-defined round filling defect, which can usually be recognized by their mobility and removed through fallopian tubes by additional injection of contrast material. Another common technical artifact in HSG that can take place in up to 6 % of patients undergoing the procedure is venous or lymphatic intravasation (Fig. 2).30 Most commonly this occurs as a result of inadvertent insertion of the cannula into the myometrium and excessive pressure during the injection of contrast material.20 Since endometrial scarring, fibrosis, and ulcerations promote entry of the contrast material into myometrial vessels, one has to be aware that patients with uterine adhesions, tubal disease and/or obstruction, history of recent uterine operations, uterine malformations, history of uterine tuberculosis, and submucous tumors are predisposed to this complication of HSG.20,22 Radiographically, early intravasation appears as filling of multiple thin beaded channels following an ascendant course.27 Although often venous and lymphatic channels can be identified by their anatomy, contrast intravasation into uterine and ovarian veins can sometimes be mistaken for tubal filling.20 Fig. 2 Venous intravasation seen as a network of thin vessels on top of uterus and in a pattern that could be confused with tubal filling. Apparent Tube Blockage If an HSG procedure shows blockage of one tube and patency of the other, there could simply be a resistance difference between the two tubes, resulting in the contrast following the path of least resistance and thus falsely suggesting that the tube with greater resistance is blocked.12 Another scenario resulting in false-positive diagnosis of tubal occlusion is when inadequate wedging of cervical cannula allows leakage of contrast material into the vagina, thus interfering with generation of sufficient intracavitary pressure and often leading to a misdiagnosis of tubal occlusion.19 In these situations, it would be of great benefit to proceed with a selective salpingogram and clearance of the apparently blocked tube, as that would result in correct diagnosis of the patient.12, 19 It is also important to be aware of the fact that tubal spasm may mimic tubal occlusion and result in false-positive diagnosis of tubal occlusion.2 In order to minimize such diagnostic errors, use of smooth muscle relaxants for the relief of tubal spasms has been suggested.26 In addition, concluding the study prematurely, failing to obtain delayed or follow-up films as well as to use adequate amounts of contrast material can lead to a false diagnosis of proximal tubal obstruction. If an apparent unilateral blockage is visualized, one should continue to add 1-2 ml of contrast material until either the material from the patent side appears to obscure the pelvic shadow or the opposite tube fills and spills.20 Several authors have shown the importance of consistency in injection pressure and spot film timing in carrying out HSG procedures. Differences in both of these aspects have been shown to have a great effect on visualization of anatomic contours as well as the assessment of tubal patency and filling.9,19 Result Interpretation and Analysis Reader Reliability When considering reasons for misdiagnosis with an imaging technique, in addition to dissecting out technical aspects of the study, one has to take into account the unavoidable possibility of objectiveness involved in the interpretation of results. A study by Glatstein et al found considerable interobserver variability among reproductive endocrinologists in their assessment of HSG films in regards to various categories. After distributing 50 HSG films to five fertility specialists with an average of 20 in clinical experience, the authors compared their impressions in uterine and tubal categories by determining the kappa () statistic (Table 1).8 Variable abnormal uterus abnormal tubes Right side fill dye spillage hydrosalpinx adhesions statistic Variable statistic Left side fill dye spillage hydrosalpinx adhesions 0.633 0.399 0.575 0.104 0.358 0.430 0.603 0.404 0.645 0.111 Table 1. Kappa statistics for interobserver reliability of the HSG result interpretation in specified categories (from Glatstein et al). Whereas the best agreement was found between filling aspects and evaluation for hydrosalpinx, the biggest discrepancies were found in regards to tubal adhesions. Overall, interobserver reliability was slightly better in the evaluation of abnormal tubes ( = 0.430) than in abnormal uteri ( = 0.358). A retrospective review of 50 HSG films by reproductive endocrinologists and radiologists shed some light on intrareader and interreader reliability in interpreting HSG findings as well as compared reliability of radiologists and clinicians (Table 2).17 High intrareader reliability among both radiologists and clinicians, as defined by > 0.6, was found in evaluation of a normal uterus, normal tubes, congenital uterine anomaly, uterine filling defect, and tubal obstruction. In contrast, low intrareader reliability was seen in detection of hydrosalpinx, uterine adhesions, and pelvic adhesions (Table 2). Variable k statistic Variable k statistic normal uterus normal tubes congenital uterine anomaly uterine filling defect tubal obstruction 0.71 0.68 0.80 0.67 0.71 hydrosalpinx uterine adhesions pelvic adhesions 0.28 0.37 0.33 Table 2. Overall kappa statistics for intrareader reliability of HSG results for each diagnosis. (from Renbaum et al) The authors also used the interclass correlation coefficient (ICC) to summarize the data from all readers and multiple evaluations per reader in order to evaluate outcomes across readers and thus to assess the interreader reliability (Table 3). Variable ICC Variable ICC normal uterine contour normal tubal patency congenital uterine anomaly uterine filling defect 0.58 0.53 0.53 0.50 hydrosalpinx cornual obstruction distal obstruction pelvic adhesions SIN 0.37 0.38 0.36 0.13 0.27 Table 3. ICC (interclass correlation coefficient) as a measure of interreader reliability for HSG film readings for each diagnosis; SIN=salpingitis isthmica nodosa. (from Renbaum et al) As can be seen from Table 3, the interreader reliability was found to be high, as defined by ICC > 0.49, for normal uterine contour, normal tubal patency, uterine congenital anomaly, and uterine filling defect. A slightly lower reliability was found in evaluation of hydrosalpinx as well as cornual and distal tubal obstruction. The lowest interreader reliability was found for pelvic adhesions and salpingitis isthmica nodosa. While no statistically significant differences were found among reliability of clinicians and radiologists, certain trends were observed. Reproductive endocrinologists appeared to be more consistent than radiologists in diagnosing uterine anomalies, cornual obstruction, and hydrosalpinx. Radiologists, on the other hand, were more consistent in evaluating uterine adhesions and salpingitis isthmica nodosa.17 Diagnostic Criteria in Evaluation of Peritubal Adhesions Valentini et al showed improvement in HSG diagnostic accuracy for peritubal adhesions in patent tubes by taking into account more than one of the reported radiographic signs when using laparoscopy as the gold standard.11,28,29 The HSG data was analyzed according to two different criteria for normality and abnormality: (1) no sign means a normal result, one or more signs mean an abnormal result, (2) up to one sign means a normal result, two or more signs mean an abnormal result. These HSG results classified with 2 different criteria were compared to their corresponding findings at laparoscopy and analyzed with kappa statistics. Whereas the first criteria yielded a low diagnostic accuracy in both patent and distally nonpatent tubes as compared with laparoscopy findings (k = 0.144 and 0.045 with insignificant p value), the second criteria improved the overall accuracy of HSG in radiologically patent tubes by 89.2 % with reduction in false-positive rates from 82.3 % to 11.7 %, an acceptably low false-negative rate of 9 %, improvement in kappa value by a factor of 5.4 and in p value of 0.001. Therefore, including one more radiographic sign in the diagnostic criteria improved the accuracy of HSG diagnosis of peritubal adhesions in radiologically patent tubes. Result Stratification in Assessing Tubal and Peritoneal Factors Diagnostic accuracy of imaging techniques can often be improved by devising appropriate classification systems. Opsahl et al performed an informative study where they proposed and validated a practical classification system of HSG results, which correlated reasonably well with presence and severity of tubal and peritoneal disease.14 The authors classified their findings in 756 patients as (1) normal, (2) abnormal, and (3) suspicious (image without completely normal findings or without unambiguous bilateral distal tubal obstruction). Analysis revealed that suspicious films are primarily responsible for the false-positive results previously attributed to the HSG results. In fact, the overall false-positive rate falls from 28.8 % to 1.2 % (P < 0.001) when one includes only normal and abnormal HSG categories. Findings in normal and abnormal categories quite accurately predicted pathological or normal findings, as confirmed later by surgery. Positive predictive value of 95.7 % was found for bilateral distal tubal occlusion with or without hydrosalpinx (abnormal category). For the normal category, the authors found a false-negative rate of 3.4 % and a negative predictive value of 96.6 %. Thus, while the accuracy of HSG is quite high for patients with a normal pelvic structure or a distal tubal obstruction, confirmatory laparoscopy is recommended for suspicious findings. Normal Variants and Congenital Uterine Anomalies The ability to recognize a spectrum of radiographic findings among normal anatomic variants is essential to the correct interpretation of HSG films. Some of the more commonly encountered normal variants recognized on radiographic films are myometrial folds, double uterine contour, and prominent cervical glands.27 Considered to be benign remnants of the mullerian duct fusion during fetal development, myometrial folds occasionally appear as broad longitudinal folds parallel to the uterine cavity, whose visualization is obliterated by increasing amounts of contrast material.30 Double contour appears as a thin line of contrast medium surrounding the uterine cavity and is often appreciated when HSG is performed during late secretory phase of the menstrual cycle. If HSG is performed during early pregnancy, one can often see contrast material underneath the decidual reaction of the endometrium that appears as double contour.27 Yet another normal finding is that of normal endocervical glands appearing as multiple tubular structures originating from both cervical walls. Congenital uterine anomalies can lead to significant gynecologic problems and thus are important to diagnose correctly.5 When unicornuate uterus is suspected, it is important to rotate the uterus, as failure to do so has been shown to lead to misdiagnosis in the case of a normal uterus. Usually, true unicornuate uterus is displaced laterally with more than 80 % of patients missing a kidney on the contralateral side.20 Conclusion HSG is an important diagnostic test in the evaluation of intrauterine abnormalities and tubal patency in the infertility workup of female patients. One can maximize the yield of this technique and minimize misdiagnosis of patients by practicing skilled techniques, understanding the limitations of HSG, and being consistent and thoughtful in the interpretation of the radiographic films. Whereas invaluable in the initial work-up of infertility patients, one should consider other diagnostic modalities, such as hysteroscopy and/or laparoscopy, if no improvements are seen in about six months after infertility treatments and normal HSG findings. References 1. 2. 3. 4. Cundliff G. Infertile couples with a normal HSG. J Reprod Med 1995; 40: 19-23. DeCherney AH. Anything you can do I can do better...or differently! Fertil Steril 1987; 48: 374376. DeCherney AH, Kort H, Barney JB, DeVore GR. Increased pregnancy rate with oil-soluble hysterosalpingography dye. Fertil Steril 1980; 33: 407. El-Minawi MF, Abdel-Hadi M, Ibrahim AA, Wahby O. Comparative evaluation of laparoscopy and hysterosalpingography in infertile patients. Obstet Gynecol 1978; 51: 29-32. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. Farber M. Uterus bicornis unicollis with a noncommunicating rudimentary uterine horn: an unusual cause of dysmenorrhea. Int J Gynaecol Obstet 1973; 11: 190. Forestier J. Iodized oil in roentgenology. Am J Roentgen 1926; 15:352. Ganglione R, Valentini AL, Pistilli E, Nuzzi NP. A comparison of hysteroscopy and hysterosalpingography. Int J Gynecol Obstet 1996; 52: 151-153. Glatstein IZ, Sleeper LA, Lavy Y, Simon A, Adoni A, Palti Z, Hurwitz A, Laufer N. Observer variability in the diagnosis and management of the hysterosalpingogram. Fertil Steril 1997; 67: 233-237. Gleicher N, Confino E, Corfman R, Coulam C, Decherney A, Haas G, et al. The multicenter transcervical balloon tuboplasty study: conclusions and comparison to alternative technologies. Hum Reprod 1993; 8: 1264-71. Hofmann GE, Scott RT, Rosenwaks Z. Common Technical Errors in Hysterosalpingography. Fertil Steril 1992; 37: 41-43. Karasick S, Goldfarb AF. Peritubal adhesions in infertile women: diagnosis with hysterosalpingography. AJR 1989; 152: 777-779. Livsey R. Hysterosalpingography. Australasian Radiology 2001; 45: 98-99. Opsahl MS, Klein TA. Tubal and peritoneal factors in the infertile woman: use of patient history in selection of diagnostic and therapeutic surgical procedures. Fertil Steril 1990; 53: 632-637. Opsahl MS, Miller B, Klein TA. The predictive value of hysterosalpingography for tubal and peritoneal infertility factors. Fertil Steril 1993; 60: 444-448. Pellicer A. Hysteroscopy in the infertile woman. Obstet Gynecol Clinics North America 1988; 15: 99-105. Preutthipan S, Linasmita V. A prospective comparative study between hysterosalpingography and hysteroscopy in the detection of intrauterine pathology in patients with infertility. J Obstet Gynaecol Res 2003; 29: 33-37. Renbaum L, Ufberg D, Sammel M, Zhou L, Jabara S, Barnhart K. Reliability of clinicians versus radiologists for detecting abnormalities on hysterosalpingogram films. Fertil Steril 2002; 78: 614618. Rindfleisch W. Darstellung des Cavum Uteri. Klin Wochenschr 1910; 47: 780. Risquez F, Confino E. Transcervical tubal cannulation, past, present and future. Fertil Steril 1993; 60: 211-226. Siegler AM, Hysterosalpingography. Fertil Steril 1983; 40: 139-158. Snowden EU, Jarrett JC, Dawood MY. Comparison of diagnostic accuracy of laparoscopy, hysteroscopy, and hysterosalpingography in evaluation of female infertility. Fertil Steril 1984; 41: 709-713. Soules MR, Spadoni LR. Oil versus aqueous media for hysterosalpingography: a continuing debate based on many opinions and few facts. Fertil Steril 1982; 38: 1-11. Swart P, Mol BWJ, van der Veen F, van Beurden M, Redekop WK, Bossuyt PMM. The accuracy of hysterosalpingography in the diagnosis of tubal pathology: a meta-analysis. Fertil Steril 1995; 64: 486-491. Swolin K, Rosencrantz M. Laparoscopy vs. hysterosalpingography in sterility investigations. A comparative study. Fertil Steril 1972; 23: 270-273. Thurmond A, Novy M, Rosch J. Terbutaline in diagnosis of interstitial fallopian tube obstruction. Invest Radiol 1986; 23: 209-210. Taylor PJ. Correlations in infertility: symptomatology, hysterosalpingography, laparoscopy and hysteroscopy. J Reprod Med 1977; 18: 339-342. Úbeda B, Paraira M, Alert E, Abuin RA. Hysterosalpingography: spectrum of normal variants and nonpathologic findings. AJR 2001; 177: 131-135. Valentini AL, Danza FM, De Vivo D, Colavita N, Vincenzoni M. Aderenze peritubariche e isterosalpingografia. Radiol Med 1985; 71: 326-328. Valentini AL, Muzii L, Marana R, Catalano GF, Summaria V, Felici F, Rossetti A, Destito C. Improvement of hysterosalpingographic accuracy in the diagnosis of peritubal adhesions. AJR 2000; 175: 1173-1176. Yoder IC. Hysterosalpingography and pelvic ultrasound: imaging in infertility and gynecology. Boston: Little, Brown, 1988: 23-28, 133-193.