Department of Medical Nursing, Faculty of Nursing, Chiang Mai
advertisement

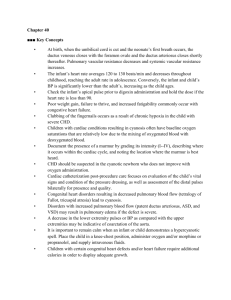
Department of Medical Nursing, Faculty of Nursing, Chiang Mai University Teaching Material for 561314: Adult Nursing II For International Program Nursing Students Semester I Academic Year 2007 ---------------------------------------------------------------------------------------------Principle of Holistic of Nursing Care for Adult with Common Problem in The Patients with Congestive Heart Failure Assist. Prof. Dr. Nitaya Pinyokham Objectives Upon completion of this course the student will be able to: Describe the pathophysiologic changes seen with congestive heart failure. List the causative factors associated with congestive heart failure. State the signs and symptoms associated with congestive heart failure. Have a better understanding of the current medical treatment options for patients with congestive heart failure. Discuss pharmaceutical interventions for treating congestive heart failure. Describe the nursing care and management of the patient with congestive heart failure. List nursing diagnosis that can be implemented to guide appropriate nursing care of the patient with congestive heart failure. Defining Congestive Heart Failure (CHF) CHF is a clinical syndrome that is described as the inability of the heart to pump an adequate amount of oxygenated blood to meet the body’s demands (adequate cardiac output). It is a condition that is marked by shortness of breath, edema, poor tissue perfusion, congestion of the vascular beds, pulmonary edema, jugular vein distention and liver congestion. Abnormal sodium levels and fluid retention (overload) are also often present with CHF. 2 Pathophysiology of CHF When CHF occurs and there is a drop in cardiac output; the sympathetic nervous system (SNS) is stimulated. Stimulation of the sympathetic nervous system activates the following compensatory changes in an attempt to increase venous return to the heart: Increased heart rate Increased force of contraction Vasoconstriction Increased preload (left end diastolic pressure) Increased afterload Increased systemic vascular resistance Note: The Frank Starling Law (or curve) states that up to a point, the greater the preload, the greater the cardiac output however; excessive preload can have the reverse affect and actually decrease cardiac output. In addition to an increase is SNS, the kidney’s also attempt compensate for the initial decrease in cardiac output by decreasing renal perfusion and activating the renin-angiotensin-aldosterone-system (RAAS). When RAAS is activated the following compensatory process begins: Angiotensin II and Aldosterone are released which lead to sodium retention and vasoconstriction. This release activates the release of increased anti-diuretic hormone (ADH). The release of ADH causes the kidneys to reabsorb more water. The combination of increased sodium and water leads to a further increase preload. In both acute and chronic CHF these initial compensatory mechanisms eventually become counterproductive and maladaptive. When either the right or left ventricle lose the ability to handle the extra or increased preload; there is a back up of fluid. If the left ventricle is involved, the fluid back up reaches the pulmonary bed and causes symptoms such as shortness of breath, dyspnea on exertion, orthopnea and pulmonary edema will present. If the right ventricle is involved the fluid backs up into the systemic circulation and produces symptoms such as elevated central venous 3 pressure (CVP), elevated jugular venous distention, hepatomegaly, ascites, anorexia and peripheral edema. Classifications of CHF Systolic Heart Failure – This refers to the hearts inability to contract effectively. Characteristics of systolic heart failure include an ejection fraction (EF) that is less than 35% to 40%. The gold standard for treatment of systolic heart failure is ACE inhibitors, Beta Blockers and Diuretics (Digoxin is added if the patient remains symptomatic after the gold standard treatment). Diastolic Heart Failure – With diastolic heart failure the heart can contract effectively (EF > 40%), but the ventricle has increased resistance to filling and causes a reduction in stroke volume. Treatment for diastolic heart failure (according to the American Heart Association Guidelines 2001) includes management of blood pressure, heart rate and fluid retention/overload with ACE inhibitors, Beta Blockers and Calcium Antagonists. Although systolic and diastolic classifications of heart failure focus on the pathophysiologic changes that occur; the New York Heart Association (NYHA) has published a “functional” classification for CHF. This breakdown is as follows: Class I – Patients without physical limitations. Class II – Patients who are comfortable at rest but become symptomatic with activity. Class III – Patients who are comfortable at rest, but have marked limitations with any type of physical activity. Class IV – Patients who are symptomatic with rest or activity. Causes of CHF There are thought to be many causes for the development of CHF. Common causes either independent or in combination are listed below: Weakened heart muscle Dampened/stenosed heart valves Atherosclerosis 4 Acute MI Toxic exposure (substance abuse with alcohol or cocaine) Infection Hypertension Pericardial disease (pericardial effusion) Congenital heart disease Prolonged (serious) arrhythmias Signs and Symptoms of CHF Left Sided Heart Failure: Capillary refill > 3 seconds Orthopnea Dyspnea on exertion Nocturnal dyspnea Cough with frothy sputum (indicative of pulmonary edema) Tachypnea Diaphoresis Basilar crackles or rhonchi Cyanosis Hypoxia (respiratory acidosis) Elevated pulmonary artery pressures Elevate pulmonary artery occlusive pressures Audible S3 and S4 heart tones Nocturia Mental confusion Weight gain Fatigue/weakness/lethargy Murmur or mitral insufficiency Enlarged left ventricle on X-ray Enlarged left atrium on X-ray Narrowing pulse pressure Pulsus alternans (alteration of weak and strong beats) 5 Right Sided Heart Failure: Hepatomegaly Splenomegaly Dependant pitting edema Venous distention Hepatojugular reflux Oliguria Arrhythmias Elevated CVP Elevated right atrial pressure Elevated right ventricular pressure Narrowing pulse pressure Kussmaul’s sign Murmur or tricuspid insufficiency Audible S3 and S4 heart tones Fatigue/weakness Abdominal pain Anorexia Enlarged right atrium on X-ray Enlarged right ventricle of X=ray Ascites Weight gain Medical Diagnosis of CHF: In addition to patient history and physical assessment; the following labs, tests and procedures are recommended for diagnosing CHF. Lab Tests: Beta Natriuretic peptide (BNP) – this laboratory study can help to identify CHF as the origin for unclear dyspnea. When serum levels of BNP are less than 100pg/ml the diagnosis of CHF is unlikely. Serum levels of BNP that range between 100 – 500 pg/ml is probably caused by CHF and BNP levels that are > 500 pg/ml are considered to be definitely consistent with a diagnosis of CHF. 6 Serum lab values that positively identify pre-renal apothecia, elevated alanineaminotransferase (ALT), elevated Aspartate Aminotransferase (AST) or elevated bilirubin are suggestive of congestive hepatomegaly (which is consistent with CHF). Cardiac enzymes and other serial markers for cardiac ischemia or injury should also be drawn and analyzed. Arterial blood gases (ABG’s) should be drawn when there is evidence of hypoxia, dyspnea or pulmonary edema. A decreased erythrocyte sedimentation rate (ESR) can help to diagnose early mild to moderate CHF. Elevated creatinine levels and dilutional hyponatremia may be observed in severe cases of CHF. Imaging Studies: Chest X-ray – Although diagnosis of CHF may be limited by chest X-ray, it is one of the most useful tools available. Cardiomegaly can be seen if the cardiothoracic ratio is greater than 50%. Echocardiography (ECHO) – Identifying the regional wall motion abnormalities that are associated with CHF can be accomplished with an echocardiogram. Other Tests/Procedures: Electrocardiogram (ECG) – This is a non-specific test that may be useful in diagnosing cardiac ischemia that is caused by CHF. ECG can also diagnose dysrhythmias that are caused by left ventricular hypertrophy (which often occurs in left sided failure). Cardiac catheterization may be indicated for severe cases of CHF in an attempt to assess and evaluate the progression and prognosis of the syndrome. A pulmonary artery catheter may be placed in order to provide initial and continual monitor of heart pressures and responses to diuretic therapy (this is not a required intervention). 7 Medical Treatment Options Because CHF is considered to be “syndrome” rather than a disease process; the most appropriate treatment regimen is one that focuses on treating the symptoms and processes that present such as ischemia, atherosclerosis, inadequate systolic/diastolic function, chest pain, excessive preload and renal artery stenosis. The following medical treatment modalities should be considered for effective treatment of CHF: ABC’s (airway, breathing, circulation). Oxygen therapy as needed (100% non-rebreather mask or intubation with mechanical ventilation may be initially required). Continuous cardiac/Pulse oximetry monitoring. HOB @ 30 degrees (this helps to reduce venous return). Pharmaceutical therapy often begins with nitrates and diuretics (appropriate medication regimens are the major focus of treatment). Restrict sodium and fluid intake (strict I&O) Bed rest is tolerated (patients may not tolerate bed rest and may wish to sit up with legs dangling off the bed). Pain relief (Morphine for chest pain). If a pulmonary artery catheter is placed; the following hemodynamic pressures should be monitored for patients with CHF. o Cardiac Output (the amount of blood ejected from the heart per minute). o Cardiac Index (the cardiac output divided by the body surface area). o Central Venous Pressure (the pressure in the right atrium). o Preload/PAWP (the volume of blood in the ventricle at the end of diastole). o Afterload/SVR (the amount of work or resistance that the ventricles must over come to eject stroke volume). o Pulmonary Artery Pressure (this is the pressure within the pulmonary bed). 8 Normal Hemodynamic Pressures Hemodynamic Pressure Normal Value Cardiac Output 4-8 L/min Cardiac Index 2.5-4 L/min Central Venous Pressure (CVP) 2-8 mm Hg Preload (PAWP) 8-12 mm Hg Afterload (SVR) 800-1200 dynes Pulmonary Artery Systolic Pressure 20-30 mm Hg Pulmonary Artery Diastolic Pressure 6-12 mm Hg Pharmaceutical Treatment Options Captopril (Capoten) – Angiotensin converting enzymes (ACE) inhibitors such as captopril are recommended for the treatment of CHF because they produce vasodilation and blockage of the RAAS process. By blocking the RAAS compensatory mechanism. Aldosterone and ADH are also blocked which prevents fluid retention. As a result of these actions, captopril reduces preload and left ventricular filing pressures which increase cardiac output. Carvedilol (Coreg) – Coreg is a non-selective B-blocker that improves left ventricular function and increases survival rates by increasing the force of contraction. Because B-blockers have a negative inotropic effect, it is recommended that they be titrated slowly after the patient has been stabilized with ACE inhibitors and diuretics. Furosemide (Lasix) – Lasix is a loop diuretic and is often ordered to reduce or eliminate excessive fluid (they should be used only for patients with signs and symptoms of fluid overload with the goal of returning the patient to a euvolemic state). Morphine – Because catecholamines are released in response to the anxiety and pain associated with suffering an acute MI (increasing the workload of the heart). Morphine can be used to help reduce the pain that can be associated with CHF. Morphine is also beneficial in reducing the hemodynamic workload by increasing venous capacitance and reducing systemic vascular resistance (therefore decreasing myocardial oxygen demand). 9 Nitroglycerin – Nitrates such as Nitroglycerin cause vasodilation of the vessels and help to decrease cardiac oxygen demand, cardiac preload and afterload while increasing cardiac output. This in return helps to decrease venous return and alleviates the heart from overworking. Dopamine – Dopamine has both a and b-adrenergic effects (as well as dopaminergic effects). At low doses (2-5 mcg/kg/min) it increases renal and mesenteric blood flow. At moderate doses (5-10 mcg/kg/min) it has a positive inotrope affect which increases blood pressure and cardiac output. At larger doses (10-20 mcg/kg/min) it exhibits a pure alpha stimulation which causes peripheral vasoconstriction with both increased systemic vascular resistance (SVR) and afterload. Dobutamine – Dobutamine stimulates B-receptors of the heart and provide a direct acting positive inotrope effect. Dobutamine increases stroke volume and cardiac output by increasing cardiac contractility while decreasing SVR. By increasing contractility and cardiac output; there is more oxygen rich blood available for damaged tissue. Milrinone (Incor) – Milrinone is a phosphodiesterase inhibitor that may be effective in the treatment of exacerbations of CHF. Milrinone decreases or inhibits the breakdown of cyclic AMP resulting in an increase in cardiac contraction and arterial venous dilation. Digitalis (Digoxin) – Digoxin is a cardiac glycoside that works by inhibiting the sodium-potassium pump system. The result of this action is increased cardiac contractility. Nursing Diagnosis Decreased cardiac output r/t ventricular damage, ischemia and restriction secondary to fluid overload. The defining characteristics of decreased cardiac output Impaired gas exchange r/t increased pulmonary interstitial fluid accumulation. The defining characteristics of impaired gas exchange 10 Altered tissue perfusion (cardiac) r/t imbalance between oxygen demand and supply. Defining characteristics of altered cardiac tissue perfusion Ineffective breathing pattern r/t imbalance between oxygen demand and supply. Defining characteristics of ineffective breathing pattern include: Alteration in fluid balance (excess) r/t decreased cardiac output and Aldosterone and ADH compensatory secretion. Defining characteristics of alteration in fluid and electrolytes Fatigue r/t imbalance between oxygen demand and supply. Defining characteristics of fatigue Anxiety r/t uncertain outcome. Defining characteristics of anxiety include: Knowledge deficit r/t new diagnosis/new medication regimen. Defining characteristics of a knowledge deficit Nursing Care and Management Assessment/Interventions: Monitor vital signs/oxygenation/Neuro status (report changes in heart and respiratory rate/patterns as well as changes in LOC). Daily weight (a 2.2 kg weight increase over a 1 day period is considered significant). Breath sounds (monitor for increased crackles, rhonchi or pulmonary congestion). Capillary refill (if greater than 3 seconds, assess for signs of peripheral edema). The presence of jugular vein distention (jugular vein distention can be a sign of worsening right sided heart failure). The presence of hepatomegaly (also a sign of worsening right sided heart failure). The presence of ascites (also a sign of worsening right sided heart failure). EKG changes Evaluate electrolyte levels (sodium, potassium and creatinine) Digoxin levels (if patient taking Digoxin) Pain level (degree, quality, source, location, onset and relieving factors) 11 Intake and Output (monitor effects of diuretic therapy and observe for signs and symptoms of either fluid overload or deficit) Assess degree of discomfort associated with activity (provide a proper rest/activity balance. Group nursing interventions when appropriate). Monitor for restless, anxious behavior and promote self care participation. Maintain adequate bowel function (stool softeners such as Colace should be ordered to prevent constipation). Patient Teaching: The following patient/family education should be provided prior to discharge and should also be reiterated at post discharge office visits: Discharge medication regimens Diet (low sodium) Fluid restrictions Activities of daily living Exercise Smoking cessation Available community resources/referrals The importance of making and keeping Dr.’s appointments Avoiding infection (flu/pneumovax vaccines) Self monitoring (when to report symptoms or changes such as shortness of breath, dyspnea, changes in weight [greater than 2.2 lbs over 1-2 days], pedal edema, blood pressure changes, nausea or fatigue). References Hudson, K. (2007). CHF-2 Nursing CEs. Retrieved 23, 2007 from http://dynamicnursingeducation.com/class.php?class_id=130&pid=23 Zambroski, C. H. (2006). Management beyond an uncertain illness trajectory: palliative care in advanced heart failure. International Journal of palliative Nursing, 12(12, 566573. 12 Nursing Diagnosis Decreased cardiac output r/t ventricular damage, ischemia and restriction secondary to fluid overload. The defining characteristics of decreased cardiac output include: o Dysrhythmias (tachycardia, bradycardia, electrocardiographic changes). o Altered Preload (jugular vein distention, fatigue, edema, increased/decreased central venous pressure [CVP], increased/decreased pulmonary artery wedge pressure [PAWP]). o Altered Afterload (cool clammy skin, shortness of breath/dyspnea, oliguria, prolonged capillary refill, decreased peripheral pulses) o Altered Contractility (crackles at the lung bases, cough, orthopnea/nocturnal dyspnea, cardiac output less than 4 liters/min, cardiac index less that 2.5 liters/min, decreased stroke volume, decreased left ventricular stroke work index (LVSWI), S3 or S4 heart sounds present). o Behavioral/Emotional (anxiety or restlessness). Impaired gas exchange r/t increased pulmonary interstitial fluid accumulation. The defining characteristics of impaired gas exchange include: o Decreased carbon dioxide (hyperventilation) o Dyspnea (difficulty breathing often secondary to fluid overload and/or pulmonary edema o Abnormal Arterial blood gas levels (respiratory alkalosis) o Hypoxia (oxygen delivery and consumption mismatch) o Tachycardia (increased workload of the myocardium) o Abnormal skin color (pale, dusky) Altered tissue perfusion (cardiac) r/t imbalance between oxygen demand and supply. Defining characteristics of altered cardiac tissue perfusion includes: o Altered respiratory rate (shortness of breath, dyspnea) o Use of accessory muscles to breath 13 o Capillary refill greater than 3 seconds (poor circulation of oxygenated blood) o Abnormal arterial blood gas levels (low Co2 from hyperventilation) o Chest pain (increased work load of the heart) o Sense of impending doom (feelings of doom often surface when a patient is having difficulty breathing) o Dysrhythmias (due to myocardial work loads) Ineffective breathing pattern r/t imbalance between oxygen demand and supply. Defining characteristics of ineffective breathing pattern include: o Decreased inspiratory/expiratory pressure (due to the extra work load of breathing) o Shortness of breath/dyspnea (fluid overload) o Pursed lip breathing (an attempt to increase the length of expiration) Alteration in fluid balance (excess) r/t decreased cardiac output and Aldosterone and ADH compensatory secretion. Defining characteristics of alteration in fluid and electrolytes includes: o Jugular vein distention (right sided failure) o Decreased hemoglobin (dilutional) o Weight gain (over a short period of time) o Changes in respiratory pattern (dyspnea, shortness of breath) o Pulmonary congestion (crackles, rhonchi, S3 auscultated) o Restless/anxious behavior o Increased CVP o Oliguria, azotemia, specific gravity changes o Positive hepatojugular reflex (due to hepatomegaly) Fatigue r/t imbalance between oxygen demand and supply. Defining characteristics of fatigue include: o Inability to restore energy (even after appropriate rest and sleep periods). 14 o Inability to maintain a level of physical activity (often due to shortness of breath and discomfort). o Verbalization of unremitting or overwhelming exhaustion. o Increase in physical complaints (unrelated to current medical condition). o Verbalization of guilt (for not being able to keep up with things) Anxiety r/t uncertain outcome. Defining characteristics of anxiety include: o Diminished productivity o Scanning and vigilance o Poor eye contact/glancing around/restless and irritable behavior o Extraneous movement (repetitive movement, foot shuffling) o Insomnia o Regretful/helpless/worried o Quivering of voice when speaking o Elevated pulse/blood pressure Knowledge deficit r/t new diagnosis/new medication regimen. Defining characteristics of a knowledge deficit include: o Verbalization of the problem o Inaccurate follow up or follow through o Inappropriate or aggravated behavior o Hysterical, hostile, agitated or apathetic behavior o Ineffective coping r/t health care demands and new diagnosis