Ch 20 DIGESTION
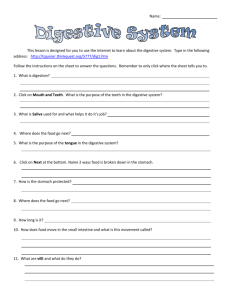
advertisement

1 Ch21 DIGESTION DIGESTION: primary fx is the breakdown of food into monomers and to transfer these nutrients, as well as water & electrolytes, into the body's internal environment. What part of the nervous system controls digestion? Which cranial N provides this stimulation? ABSORPTION: monomers are transported across the small intestine epithelium into the blood & lymph. Generalizations 1. Composition of food is similar to body tissues. So why don't we digest ourselves? We have protective mechanisms: - enzymes needed for hydrolysis are secreted in an inactive form. - the gastrointestinal tract is not inside the body—the harsh conditions that exist for digestion are external to the simple columnar epithelium of the stomach, small intestine, & large intestine. The lumen is analogous to a garden hose stuck through the middle of the body. Complex (“tube inside tube” tissue layered) animals, particularly the vertebrates, specialize in digesting food particles “outside their body”—the food is too big to be absorbed and must be broken into monomers before absorption. What good is this adaptation? Importance of Ingested Food 1. Essential for an energy source for cellular respiration: Glucose ATP 2. Building supplies for growth, maintenance, & repair. Macromolecules that are ingested are used to form tissues. Protein in chicken or beef is broken down into to amino acids to be used to create more of you!! Normally about 95% of ingested food is made available for the body. Digestion has 4 Basic Processes 1. Motility refers to the movement of food through the digestive tract through the processes of : - Ingestion: taking food into the mouth - Mastication: chewing the food using skeletal Mm of the mandible & mixing it with saliva What are 2 major masticatory Mm? - Deglutition: swallowing food - Peristalsis: rhythmic, wavelike contractions that move food through the GI tract. Due mostly to involuntary contraction of smooth M in mucosa & submucosa. 2. Secretion: many different digestive juices are secreted by exocrine glands. - All secretory glands extract large amounts of water from the ECF and large amounts of energy are required for the manufacture & transport of substances. - Controlled by hormonal & neural stimuli. Most secretions are reabsorbed, except when one vomits or has diarrhea, so why can diarrhea be deadly? - Exocrine secretions: water, electrolytes, HCl, & digestive enzymes secreted by stomach, pancreas, & liver. - Endocrine secretions: the stomach & small intestine secrete a number of hormones that help regulate the digestive system. 3. Mechanical & chemical digestion: breakdown of food into small units by smooth muscular action (mechanical) and smaller absorbable units by hydrolysis with digestive enzymes (chemical). 4. Absorption: passage of food monomers from the lumen into the epithelium, the ECF, and then into capillary beds or lymph vessels. Where do the lymph vessels eventually empty into the circulatory system? Three Food Stuff Classes 1. Carbohydrates = monosaccharide chains - Starch from plants - Glycogen from meat - Cellulose (plant fiber) cannot be digested by humans, so why is it an important part of our diet? - Disaccharides: e.g., sucrose = table sugar (1 glucose + 1 fructose) or lactose = milk sugar (1 glucose +1 galactose). All of the above are converted by chemical digestion into monosaccharides. Salivary amylase & pancreatic amylase help in the hydrolysis of polysaccharides into disaccharides, then sucrase, maltase, & lactase from the pancreas break it down into monomers so the small intestine’s simple columnar epithelium can absorb them, then to intestinal capillaries liver rest of body. Where does the liver’s blood drain into? 2 2. Proteins: amino acid chains held together by peptide bonds. Hydrolysis (with enzymatic help) breaks those bonds, so we can absorb the amino acids, dipeptides, & tripeptides. Enzymes ex.: pepsin, trypsin, chymotrypsin, carboxypeptidases. 3. Lipids: most dietary fat is in the form of triglycerides. Break these down into monoglycerides (glycerol + 1 fatty acid) & 2 fatty acid chains, which are absorbable. Plasma lipids are insoluble in water, and digestion is accomplished by the chemical rx hydrolysis, which is the addition of water to break chemical bonds, and enzymes are necessary to make the rx happen fast enough to sustain life. - Remember digestive enzymes are very specific to the bonds they help break: Gastric pepsin only breaks protein peptide bonds in the stomach. To fx enzymes must have the right conformation, pH, temp, & coenzymes. Oral Cavity & Saliva: mastication provides mechanical breakdown of large food molecules into smaller ones & mixes food with mucous saliva to form a bolus of food for swallowing. 1. parotid, sublingual, & submandibular salivary glands produce saliva List 5 major fxs of saliva: 2. Saliva is 99.5% H2O & 0.5% protein & electrolytes - the major protein is salivary amylase = breaks polysaccharides down into maltose (disaccharide of 2 glucose monomers). Process begins in mouth & is continued in the stomach until when? - mucus (mucin = glycoprotein) is a thick, slippery protein (slippery when wet!) that facilitates swallowing by lubricating food particles & holding them together; rinses the mouth - Lysozymes kill bacteria 3. No absorption of food occurs in the mouth or pharynx or esophagus or stomach. PHARYNX & ESOPHAGUS: swallowing, aka deglutition: moves food from oral cavity to stomach. Remember that the esophagus is a collapsible tube just posterior to the trachea. It takes 6-9secs to deglutinate. - swallowing is initiated when a bolus of food is forced to the rear of the mouth by the tongue; pressure on the arch bordering the oral cavity & pharynx initiates the swallowing reflex. - pressure receptors send afferent sensory impulses to the swallowing center in the medulla this activates pharyngeal Mm to swallow in an ALL or NONE FASHION. The initiation is voluntary, but once activated this skeletal M constriction can't be stopped. - peristalsis pushes food to the stomach—that's why you can swallow while standing on your head! - cardiac sphincter at top of gastric fundus prevents food from back flowing into esophagus. This physiological sphincter also prevents air from entering to produce gas buildup, which prevents eructation (burp, burp, burping). - emesis (aka vomiting): the esophagus & stomach are relaxed, and it’s caused by reverse peristalsis of the small intestine and contraction of the diaphragm & abdominal Mm. A flaccid stomach is squeezed between the diaphragm from above and compressed by the abdominal contents below. The glottis is closed, so vomited material does not enter the trachea. Also the uvula is elevated to close off the nasal cavity. It’s mediated by the GI receptors & the vomiting center in the medulla. Caused by touching of back of throat, irritation or distension of stomach or duodenum, elevated intracranial pressure, rotation of head, or chemical agents (emetics). STOMACH is a J-shaped, collapsed muscular tube with rugae; lined with simple columnar epithelium that form gastric pits & contain gastric glands. Fxs 1. primary fx: storage of food until it can be emptied into the small intestine. - Slow rate of emptying for optimal digestion & absorption - A meal you eat in minutes takes hours to breakdown & absorb; the fundic & proximal body regions will hold food, while the distal body & pyloric regions are busy mixing & mashing 2. secretes pepsinogen & lipase for initial protein & lipid digestion, respectively 3. secretes HCl to activate pepsinogen to pepsin & kill microorganisms (Die! Die! Die! Die!) 4. motility (smooth M contraction) of stomach mixes food with gastric secretions to form chyme Gastric Secretions: (about 2-3 L/day) hormones, mucus, enzymes, & water, which with food, all form chyme. 1. Secretions come from gastric pits 2. Goblet cells secrete mucus; lubricates, inhibits pepsin digestion of stomach lining; deep to the mucosa bicarbonate is secreted to protect itself from the HCl 3 3. Parietal cells deep in the gastric pits secrete HCl (2-3 liters/day) & intrinsic factor - HCl activates pepsinogen pepsin; provides acidic environment for proper conformation of pepsin - HCl aids in denaturing proteins to expose peptide bonds for pepsin to act on (destroys tertiary structure) - HCl kills many microorganisms - intrinsic factor (polypeptide) required for absorbing Vitamin B12, which is essential for erythrocyte formation 4. Chief cells secrete pepsinogen & gastric lipase - pepsinogen is cleaved by H+; pepsin begins protein digestion by breaking some peptide proteins bonds - pepsin is stored in form of pepsinogen, so cells don’t digest themselves - the action of gastric lipase & lingual lipase in the stomach accounts for 10% of lipid digestion 5. G cells secrete the hormone gastrin Why should you avoid coffee if you have gastric acid problems? - When food enters the stomach, gastric endocrine glands secrete gastrin into circulation - Gastrin stimulates the parietal & chief cells to secrete their products to form gastric juice 6. Mucous cells secrete mucus & bicarbonate to prevent autodigestion physically & chemically 7. Other stimuli for gastric secretion - increased HCl & pepsinogen are secreted in response to thinking about, seeing, or smelling food via the vagus cranial nerve: feedforward control mechanism. [ Aaantica-payayayaya-shuuun is making me way-ay-yate. Ann-tiss-sa……..SAY IT! SAY IT!!!!!! ] - stimulus to the stomach itself by distension & the presence of protein, which stimulates gastrin production gastric juice (HCl & pepsin). Even if there’s no food or proteins present, liquids stimulate gastrin production. Alcohol & caffeine do this well, which is why they cause stomach irritation. Gastric Generalities 1. No food or H2O is absorbed by the stomach mucosa. - Carbohydrate & protein digestion has begun, but is not completed until the small intestine. - The small amount of lipid digestion from lingual lipase in saliva is stopped after 1-2 hours, when the bolus breaks apart and the pH drops below 4.5. Gastric lipase is secreted by the chief cells. - Just water in the stomach is squeezed into the duodenum in minutes; food takes hours ("sticks to your ribs”). 2. Ethyl alcohol & aspirin are absorbed directly by the stomach mucosa - Both are lipid soluble - Both are even more rapidly absorbed by the small intestine - Thus, alcohol absorption occurs more slowly if gastric emptying is delayed. Because fat is the most potent duodenal stimulus for inhibiting gastric motility, eating fat-rich foods (whole milk or pizza with lots of cheese & sausage) before or during alcohol ingestion delays gastric emptying, preventing the alcohol from producing its effects as rapidly. Also lipids in the stomach will hold the alcohol, delaying its absorption. Of course, the liver has a maximum rx rate for breaking down alcohol of 1/2-1 oz/hr. NOTHING can make one sober faster. Caffeine will just make you an awake drunk. 3. Protected by mucosa: impermeable to H+ & held together by tight junctions & mucus secretions. Enzymes are secreted in inactive forms. Entire stomach lining is replaced in 1-2 weeks. There are also bicarbonate ions under the mucus lining to protect the simple columnar epithelium from the HCl. Gastric filling - The stomach can vary its volume from 50ml to over 1000ml during a meal. Size ranges from hotdog to football (empty full). The rugae stretch out (relax), so there’s not a high pressure built up. The stomach will grow larger if continually stretched by large meals. - If more than 1 liter is consumed (on average), the stomach is over distended, and one experiences discomfort. - Vagus N (X) mediates this action. - Secretions are stimulated here by protein presence & distension. Gastric emptying (1-6 hours) - The stomach empties by strong peristaltic action, pushing food out a relaxed pyloric sphincter. - Depends on the amount of chyme produced. Empties at a rate proportional to the volume of chyme in it, at any given time. Distention of the stomach triggers increased gastric motility by stimulating stretch receptors in the smooth M. - Fluidity of chyme. It must be in a very liquefied form, which requires lots of secretions & mixing. Another reason to drink plenty of water. 4 Factors inhibiting gastric emptying 1. Fat in the duodenum: it needs more time—lipid digestion & absorption take longer than other nutrients. 2. Acid: Chyme is acidic due to gastric HCl. Acid is neutralized in the small intestine by sodium bicarbonate. UNNEUTRALIZED ACID inhibits further emptying of chyme. 3. Duodenal distension: too much chyme in the duodenum inhibits emptying of more chyme. CHYME is emptied into the small intestine and is mixed with secretions from the small intestine itself, as well as with secretions of the liver & pancreas. And what would those many secretions be? SMALL INTESTINE - Is the site at which most digestion & absorption take place. No further digestion is accomplished after the contents of the lumen pass beyond the small intestine, and no further absorption of nutrients occurs, although the proximal half of the large intestine does absorb water, electrolytes, & a few vitamins (B 5, biotin, & K). - The small intestine is a tube that lies coiled in the abdominal cavity & is about 2m (6-7m in a cadaver due to no muscle tone). 3 segments: duodenum, jejunum, & ileum. - Food monomers are absorbed by the mucosa of the small intestine. - Villi & microvilli of the simple columnar epithelium fx to increase SA for absorption. - Simple columnar epithelium contains intestinal glands & goblet cells. - Small intestine secretes 1-2 L of intestinal fluid/day. It’s slightly alkaline & contains H 2O, hormones, & mucus. DIGESTION IN THE SMALL INTESTINE Mechanical 1. Segmentation: major movements in intestine are caused by localized contractions that oscillate back & forth - mixes the chyme, bile, bicarbonate, hormones, enzymes, & intestinal juice. - Brings nutrients into contact with the mucosa. 2. Peristalsis propels chyme through the small intestine, but very weak compared to esophagus & stomach. 3. Both processes are controlled by the parasympathetic Nn of the autonomic nervous system Chemical Digestion Products & Transport Mechanisms 1. Chyme entering small intestine is composed of partially digested carbohydrates, proteins, & lipids which are further broken down into their component monomers and absorbed into epithelium, then transported to the plasma: Starch monosaccharides; Proteins into amino acids; Triglycerides monoglycerides & fatty acids 2. This is accomplished by enzymes secreted by the pancreas & enzymes secreted by the small intestine itself. Enzymes from the small intestine are not secreted into the lumen, but are attached to the cell membrane with their active sites exposed to the chyme = brush border enzymes include enteropeptidase (activates trypsinogen from pancreas); disaccharidases = maltase, sucrase, & lactase; and peptidases. 3. Small intestine simple columnar epithelium is protected by mucus and a constant supply of new cells. A cell lasts about 3 days—they’re abraded by chyme movement. Intestinal Absorption 1. Most absorption of nutrients & water (carbohydrates, lipids, amino acids, calcium, iron, etc.) occurs in the duodenum & jejunum. 2. The ileum is responsible for the absorption of bile salts, vitamin B12, water, & electrolytes. 3. Water Absorption: the total volume of fluid that enters the small intestine each day is about 9 liters. Nearly all is reabsorbed in the small intestine. About 1.5 to 2.0 liters is passed on to the large intestine, which absorbs all, except for about 200ml that’s part of the feces. The water follows the osmotic gradient set up by the transport of ions. 4. Monosaccharides: occurs by facilitated diffusion & cotransport into lining of intestine (villi/microvilli). Transported through the capillary endothelium by facilitated diffusion. Review the Na/K pump & glucose transport across the intestinal epithelium. 5. Amino Acids: transported through the intestinal epithelium by facilitated diffusion & cotransport. Transported through the capillary endothelium the same way. 5 [ Larger peptides are absorbed through endocytosis after binding to a plasmalemma receptor. Unfortunately, peptide fragments can act as antigens, resulting in antibody formation, or simply an allergic rx to food. In newborns, large peptide absorption mainly occurs in intestinal crypt cells. At birth, the intestinal villi are small, and the crypts are well-exposed to chyme. As the villi grow and the crypts have less access to chyme, the high peptide absorption rates of the newborn decline. If parents delay the ingestion of allergy-inducing peptides, the gut has a chance to mature, which lessens the likelihood of antibody formation, and thus food allergies. A big food allergy is gluten, which is common in wheat. Since the 70’s, it’s been recommended that parents not use gluten-based cereals until the infant is several months old, and the incidence of gluten allergies has dropped. ] 6. Monoglycerides & fatty acids: transported into lining by diffusion, but because lipids are insoluble in water, they need aid in transport. - Micelles are water soluble carriers formed from the interaction of lipid monomers & bile salts. The lipid monomers of the micelle diffuse through the plasmalemma (like dissolves like). The simple columnar epithelium rebuilds the lipids and attaches proteins, excreting these lipoprotein complexes through exocytosis. They’re mostly transported by the lymph system into the circulatory system. - Low density lipoproteins (contain less protein & more cholesterol): carry cholesterol to the cells, including those lining the blood vessel walls. Results in atherosclerosis, which is the gradual blockage of Aa due to cholesterol & lipid buildup in artery walls (plaque). Atherosclerosis can lead to strokes & myocardial ischemia (= lack of blood flow to a tissue). The death of the tissue is called an infarct, hence myocardial infarction. - High density lipoproteins (contain the most protein & least amount of cholesterol). Removes cholesterol from the cells and transports it to the liver for partial elimination from the body. Lots of LDL (“bad cholesterol”) in blood increases the risk of atherosclerosis. [ Arteriosclerosis is a thickening & toughening of arterial walls. Complications related to arteriosclerosis accounts for about half of US deaths (e.g., strokes & heart attacks). Focal calcification is the gradual degeneration of the smooth M of the tunica media & subsequent deposition of calcium salts. It’s common in the limbs & groin. Rapid calcification is a complication of diabetes mellitus. Atherosclerosis is associated with damage of the endothelium & formation of lipid deposits in the tunica media. High blood lipid levels (particularly cholesterol) are a major factor. Monocytes in the blood eat cholesterol-rich lipoproteins, become full of lipid droplets, attach to the endothelium, & release growth factors. This causes the smooth M to grow, thickening the vessel wall. Other monocytes invade through the endothelium. Monocytes, smooth M cells, & epithelium all begin ingesting lipids. This build up is called plaque. If the plaque persists, the endothelial cells become swollen with lipids & gaps appear in the endothelium. Platelets stick to the exposed collagen fibers. This build up restricts blood flow, which may lead to a stroke or heart attack. Significant plaque in the artery to the sinoatrial node can cause arrhythmias in the cardiac conduction system, so that an artificial pacemaker is needed. ] 7. Electrolyte absorption occurs by active transport & cotransport. Na+, Cl-, Ca+2, Iodide, Nitrate, etc. 8. Vitamin absorption: Vitamins are small organic molecules that serve as part of coenzymes or have other, specific fxs. Need them for vital processes in cellular respiration, vision, erythrocyte formation, metabolism, & clotting. Vitamins your body can't manufacture and must obtain in the diet are called essential. The body can make the fat-soluble vitamins K & the precursor to D, but what does the body require to finish making vit D? - Water soluble vitamins: include vit C & the B vitamins thiamin, riboflavin, niacin, & folic acid; they are absorbed passively with water. Eliminated in urine, when not needed. - Fat soluble vitamins: D, E, K, A; they are absorbed passively in micelles with digested fats & stored, if not needed. What happens if one ingests no fat or not enough? - Antioxidants (betacarotene, C, & E) inactivate free radicals. Free radicals are highly reactive particles that carry an unpaired electron. Some free radicals arise naturally in the body, some due to exercise, and others from smoke & radiation. They damage cell membranes, DNA, & other cellular structures and contribute to formation of artery narrowing atherosclerotic plaques. Antioxidants protect against cancer, reduce arterial plaque, delay aging, & cataract formation. Overdoses can be deadly. More is better is a very harmful way to think. Important to have a balanced diet—remember homeostasis is a game of “just right.” Excesses can be toxic to cells, cause slow wound healing, and liver & kidney damage. Too much vit A causes hair loss & fragile bones & can kill. [ Watch those polar bear livers!!! ] [ Discovered in 20th century, vitamins were first named by their order of discovery. It’s now in vogue to use their chemical names, e.g., vitamin C is ascorbic acid. ] 6 7. Minerals or Trace Elements work in tandem with other nutrients to ensure a smoothly functioning body. They’re absorbed through cotransport & diffusion. Here are some & their basic fxs: Fe (iron) for the oxygen-binding protein hemoglobin (Hb) in erythrocytes Z (zinc) for enzyme fx Cu (copper) for Hb synthesis Cr (chromium) enhances effectiveness of insulin on carbohydrate metabolism Se (selenium) is an antioxidant Mn (manganese) has enzyme & neural fxs Ca for bone formation, muscle contraction K for nerve conduction NaCl for transport of water, electrolyte balance, nerve conduction LARGE INTESTINE (5 ft.) primarily serves as a drying & storage organ. Propulsion, Absorption, & Defecation - Consists of the cecum & appendix; the ascending, transverse, descending, sigmoid, & rectal colons; & anus. - Completes absorption of fluid, and NaCl from the chyme it receives from the small intestine. - secretes mucus - absorbs a few vitamins (biotin, B5, & K) and short fatty acid chains produced by the bacterial flora in the proximal half; the distal half is just for storage. - The colon normally receives about 500 ml of chyme/day. Since most digestion & absorption have been accomplished in the small intestine, the contents delivered to the large intestine consist of indigestible food residues (e.g., cellulose), remaining fluids, and also cellular wastes received from the liver. [ The average N. Am. eats 2-2.5 gallons of food per day & only 12 oz (protein, inorganic matter, fat, food roughage, digestive juices, shed intestinal cells, dead bacteria, & water) reach the large intestine. Mucus is secreted to bind this material together and to lubricate it & protect the colon walls. Feces are about 75% water, and the strong odor is due to the small amount of bacterial breakdown of proteins. ] Mechanical movement 1. Once indigestible food is moved into the large intestine, peristalsis (very slow) & haustral churning (haustra are the pouches) occurs smooth Mm contract chyme is pushed to the next haustra. Aids in the mixing of the chime, which facilitates water absorption. 2. Mass movements occur 3-4 times/day; long slow powerful contractions of smooth M that move over large areas of the colon. Chemical action 1. GI tract has a normal bacterial flora. The colon itself produces no digestive enzymes & has no chemical digestive fx. However, the bacteria in its lumen metabolize remaining carbohydrates & amino acids, releasing hydrogen, CO 2, methane, & H2S gases, which contribute to the odor of feces. The bacteria make the vitamins biotin, B 5, & K. [ The most numerous cells “inside” the human body are the bacteria that live in the digestive system! These organisms form a complex ecology with over 400 species. There are estimated to be as many as 100 trillion of them! The best known of these species is Escherichia coli, the common gut bacterium. Other species include Helicobacter pylori, which causes ulcers, & Lactobacillus acidophilus, which may help to suppress ulcers. Other than bacteria, there are about 10 trillion cells in the human body, of which the most numerous are brain cells (about 1.1 trillion) & erythrocytes (about 30 billion). ] 2. Absorption is limited to water, vitamins, & electrolytes in the proximal half. 3. The semisolid product delivered to the rectum is feces and contains undigested food residues, cellulose, mucus, sloughed off epithelial cells, millions of bacteria, and just enough water to allow (hopefully) its smooth passage. - feces still produced if you don't eat: waste products bilirubin, bacteria, & dead cells of GI Tract. - 75% water (100-200mls) & 25% solid. If you take in 800g of solid material you will excrete 50 g of solid wastes. - Color is from bilirubin & bile salts. A chalk-like color indicates liver malfunction—unless you’re taking Milk of Magnesia. Defecation 1. Mass peristalsis from the sigmoid colon initiates the defecation reflex. It is a spinal mediated reflex that causes the walls of the sigmoid colon & rectum to contract and the anal sphincters to relax. 2. As feces is forced into the anal canal, messages reach the brain, allowing us to decide whether the external (voluntary) sphincter should remain open or be constricted to stop the passage of feces temporarily. If the decision is to delay defecation, the reflex contractions end within a few seconds, and the rectal walls relax and feces move back into the sigmoid colon. With the next mass movement, the defecation reflex is initiated again. 7 3. We ordinarily aid defecation voluntarily by closing the glottis (entrance to the trachea) to keep air in the lungs and contracting the diaphragm & abdominal wall Mm to increase intra-abdominal pressure. This breath-holding maneuver, called the Valsalva maneuver, effectively forces the feces at your distal end (grunting). 4. As in the micturition reflex, involuntary defecation normally occurs in children until they’re 2-3 because they have not yet acquired voluntary control of their external anal sphincter (nerve myelination not finished). 5. Diarrhea results from rushing food residue through the large intestine before sufficient time is allowed for water to be absorbed. - results in excessive water loss, dehydration, & electrolyte imbalance. - Most commonly due to entertoxin produced by invading bacteria, which stimulates NaCl transport followed by water movement into the lumen. [ “Pour salt on those sluggy bacteria.” ] 6. Constipation results when food residues reside too long in the colon. Too much water is absorbed, and the stool becomes hard & difficult to pass. Causes: lack of fiber, failing to heed the call, lack of exercise, emotional upset, laxative abuse, & alcohol. Alcohol: diuretic dehydration constipation. Also, ethanol is an intestinal irritant. 7. Laxatives are lubricants such as castor oil, or cellulose such as Metamucil, or parasympathomimics that increase peristalsis (i.e., block cholinergic/muscarinic receptors), such as Immodium AD (atropine). [ Patients that need to have their bowels cleaned out before surgery are often given four liters of an isotonic solution of indigestible polyethylene glycol & electrolytes. The large volume of solution triggers diarrhea, removing all solid wastes from the GI tract. The WHO estimates that 4 million die each year of diarrhea. In the US, diarrhea in children results in 200,000 hospitalizations per year. ] Oral rehydration solutions contain glucose, as well as Na, K, & Cl. WHY DO THEY CONTAIN GLUCOSE? ACCESSORY ORGANS AID IN THE DIGESTIVE PROCESS - Liver & pancreas help by adding secretions of enzymes and other products into the small intestine PANCREAS, an endocrine/exocrine gland - Endocrine portion secretes glucagon & insulin from the alpha & beta cells in the islets of Langerhans. - Exocrine portion secretes pancreatic juice, which contains enzymes and a watery bicarbonate (alkaline) solution. (Some enzymes secreted in inactive form). Mucus is secreted by the intestinal glands to protect the small intestine from digestion. - Travel by way of pancreatic duct to hepatopancreatic duct through sphincter of Oddi into duodenum. Pancreatic Enzymes: break bonds in macromolecules to their component monomers. Secreted by acinar cells. Enzyme release is stimulated by duodenal distension. 1. proteolytic enzymes: aid protein digestion. The 3 major ones are: - trypsinogen, chymotrypsinogen, & procarboxypeptidase are the inactive forms of the enzymes; require a basic pH. - trypsinogen is converted to active form trypsin by enterokinase, an enzyme secreted by the small intestine. - trypsin then converts the other 2 to their active forms chymotrypsin & carboxypeptidase. - Each proteolytic enzyme attacks different peptide bonds, breaking them into smaller polypeptides, & eventually, amino acids. 2. pancreatic amylase aids in carbohydrate digestion; secreted in active form by islets of Langerhans. Helps hydrolyze polysaccharides to disaccharides. 3. pancreatic lipase aids in lipid hydrolysis; helps break down triglycerides into a monoglyceride & 2 fatty acids. Secreted in active form. No danger to cells. Pancreatic aqueous alkaline secretion 1. Pancreatic enzymes require a neutral/slightly alkaline pH to perform correctly (i.e. in order to not be denatured) 2. Alkaline secretion quickly neutralizes the acidic chyme received from the stomach to prevent damage to duodenum and provide the optimal pH for the pancreatic enzymes to fx. - Composed of H2O & NaHCO3 (sodium bicarbonate). 8 3. Control of pancreas: 2 hormones released by small intestine in response to chyme entering the duodenum. - secretin carried by the blood to pancreas, stimulates gastric cells to release pepsinogen & pancreatic cells to release bicarbonate solution, which is for . - cholecystokinin is carried by the blood to the pancreas to stimulate pancreatic enzyme secretion & to the gall bladder to stimulate its contraction for bile release. CCK is secreted by intestinal glands in the duodenal mucosa. [ It’s also a neurotransmitter in the CNS & enteric NS. Cholecystokinin appears to enhance satiety, so it may be possible to use as a “natural” appetite suppressant. ] Diagram: Duodenal Fluid & Enzyme Secretion Control LIVER is part of the biliary system which is composed of the liver, gall bladder, & associated ducts. 1. The liver has about 500 different fxs (summarized in Figure 21-22), but its main importance in digestion is the production of bile, which is made by the liver & stored by the gall bladder. 2. Hepatic cells in liver lobules can perform most of its many fxs. Cells are not specialized, however, except for resident phagocytes called Kupffer cells. - Bile is a yellowish/greenish/brownish liquid that is slightly alkaline: water, bile salts, cholesterol, lecithin (phospholipid), & bile pigments called bilirubin. - Bile is stored until needed. It is released by contraction of the gall bladder into the small intestine (cystic duct to common bile duct to hepatopancreatic duct) during meals by the stimulation of the hormone cholecystokinin (CCK) from duodenal mucosa upon the entrance of chyme into the duodenum. - Can get precipitation of constituents of bile in gall bladder to form gall stones, which are painful & cause impaired lipid digestion by blocking bile secretion. Removal of gall bladder is not a problem, since it isn't crucial for digestion. After removal, the bile secreted between meals is stored, instead, in the common bile duct, which becomes dilated. 9 3. Bile salts in bile provide emulsification of lipids,(i.e., mechanically breakup lipid globules into droplets) this increases the surface area for pancreatic lipase to increase lipid digestion rate. Bile salts are absorbed in the terminal ileum. Your body does not have a large store, and the same salts may be recycled up to five times in digesting one meal. 4. Bilirubin, in bile, is a waste product derived form the breakdown of worn-out erythrocytes. - Yellow pigment gives bile its color; modified by bacteria in intestinal lumen to give feces its traditional brown color. - Some is reabsorbed in the intestine and also gives urine its traditional yellow color. - If bilirubin is formed more rapidly than it can be excreted, then jaundice results. Yellowish color of your sclera & skin due to the high concentration in the blood vessels. DIGESTIVE SYSTEM CONTROL - Digestive motility & secretion are carefully regulated to maximize digestion & absorption of ingested food. - Generally regulated by the autonomic nervous system (sympathetic & parasympathetic systems) & hormones, such as gastrin, CCK, etc. Factors Regulating Digestive System Fx a plexus [ “braid” ] is an interconnecting network of axons 1. Intrinsic nerve plexi located in the muscularis layer of the GI tract and are entirely within the GI tract wall run from the esophagus to the anus. It contains as many neurons as the spinal cord and endows the tract with a considerable degree of self-regulation; sometimes called the enteric nervous system. - myenteric plexus is located between the longitudinal and circular smooth muscle layers in the muscularis. - submucous plexus is located in the submucosa - They are primarily responsible for coordinating local activity within the digestive tract, such as motility, secretion of digestive juices, & secretion of gastrointestinal hormones. 2. Extrinsic Nn are the Nn that originate outside the digestive tract and innervate the various digestive organs, namely, both parasympathetic & sympathetic Nn of the ANS. - The ANS nerve fibers influence digestive tract motility & secretion either by modifying ongoing activity in the intrinsic plexi, or, in some instances, acting directly on the smooth M & glands. - Parasympathetic innervation enhances motility & secretions by way the vagus N (X). Rest, digest, & repose response. - Sympathetic innervation inhibits motility & secretions. Fight, fright, & flight response. 3. Gastrointestinal hormones - Tucked within the mucosa of certain regions of the digestive tract are endocrine gland cells that release hormones into the blood upon appropriate stimulation. - Carried through the blood to other areas of the digestive tract, where they exert either excitatory or inhibitory influences on smooth M or exocrine glands (e.g., acinar cells in pancreas) - Examples: gastrin in stomach causes parietal & chief cells to secrete HCl & pepsinogen, respectively. Secretin and CCK cause the pancreas and liver to secrete their digestive products (enzymes, alkaline secretion, & bile). 4. Paracrine fxs are many and the field is evergrowing - histamine acts as a digestive paracrine for the parietal cells to secrete HCl - serotonin acts as a digestive paracrine to stimulate a peristaltic reflex, as well as a neurotransmitter in the enteric & central nervous systems 5. Local Factors - pH must be near optimal for enzymes to fx for digestion to occur. - Entrance of chyme stimulates stretch receptors & chemoreceptors, which in turn, stimulates motility. 6. Ultimately controlled by the medulla (brain stem). GI TRACT IMMUNE FXS The GI tract is the largest immune organ in the body. First line of defense: lysozymes & immunoglobins in saliva & gastric HCl. If pathogens or toxins reach the small intestine sensory receptors & immune cells of the gut-associated lymphoid tissue (GALT) respond. Toxin/invader flushing responses are diarrhea & emesis. 10 EATING THE "PREGAME MEAL" Many coaches & athletes believe intensely in special food rituals before a competitive event. For example, one football team may always have steak before a game or include bananas in their pregame meal. Do these rituals work? Studies show that no single food substance eaten before an athletic event will greatly enhance performance. The athlete's training is the most important determinant of performance. 1. Some food choices can actually hinder competitors, so what you eat can be debilitating for an athletic event. - Meals that are high in protein or fat take a long time to digest & empty from the stomach. This could impair performance by causing cramps or a feeling of sluggishness. - Other food rituals do not impair performance. They actually boost morale and are harmless. People attach special meanings to eating certain foods, and their faith in these practices should be respected, because they can make the difference between winning & losing a game. Some athletes are superstitious in a variety of ways. 2. The greatest benefit of the pregame meal is to prevent hunger during competition. Because the stomach can take from 1-6 hours to empty, an athlete should eat at least 3-5 hours before competition begins. - Excessive quantities should NOT be consumed before competition, especially ones high in fat & protein. - Food that remains in the stomach during competition may cause nausea, vomiting, & sluggishness. 3. The best food choices are ones that are high in carbohydrates and low in fat & protein. - These are recommended, because they are emptied from the stomach more quickly than fat or protein, which are digested very slowly. - Breakdown of protein produces nitrogenous wastes such as urea, whose osmotic activity draws H 2O from the body and increases urine volume, which could cause dehydration & cramps. Lack of water is probably the number one cause of muscle cramps. - Best choices are breads, pasta, rice, potatoes, gelatins, & fruit juices. They empty from the stomach quickly and help maintain blood glucose levels during the event. 4. Although it seems logical to eat something sugary immediately before a competitive event to provide an "energy boost," foods & beverages high in sugar should be avoided because they trigger insulin release. - Once you begin exercising, insulin sensitivity increases, which results in a decrease in blood glucose levels which causes feelings of fatigue, and an increased use of muscle glycogen stores, which can limit performance in endurance events, such as a marathon. - Therefore, sugar consumption just before a competition can impair performance. - Best to drink water within an hour of competition to ensure adequate hydration to prevent cramps.