SG Blood Glucose Monitoring - Diabetes Education & Camping
advertisement

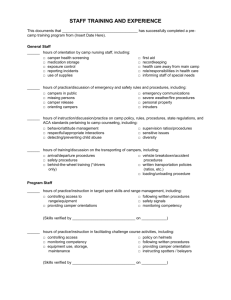
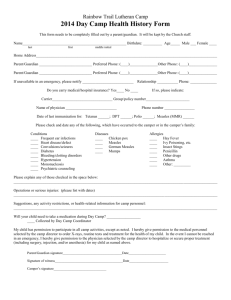
Video Study Guide Blood Glucose Meters This study guide is intended to be a general guide that will help you understand the key elements of this video. Each diabetes camp operates under detailed policies and procedures that follow Board of Health and national accreditation standards that ensure the health and safety of children with diabetes. It is essential that camp staff familiarize themselves with the policies and procedures specific to the diabetes camp at which they will work or volunteer, ask questions and use good judgment as they provide diabetes management supervision and educate youth with diabetes at camp. While doing so, it is equally important that camp staff not lose focus – camp is a place for youth to have fun with peers – to feel supported and understood, and to feel part of a passionate community. Blood sugars at day and resident camps are checked routinely throughout the day. Typically “checks” will be done before breakfast, lunch, dinner and bedtime; before any snacks; at midnight and often at 2 or 3 AM (depending on camp protocol) and whenever symptoms of low or high blood sugar are voiced by the camper or noticed by staff. Blood glucose monitors are generously provided to most camps by DECA’s “Industry Partners” which enables campers to try different choices than they may have at home. Self-retracting lancets are used to minimize the potential for cross-contamination through needle sticks. This makes disposal easier and each camp will have a policy/procedure for disposing of “sharps” (lancets and syringes) while campers are in camp or on field trips. Sharps containers (approved medical waste containers) are typically distrubted throughout camp and carried with blood glucose and insulin supplies. One of the most common sayings at camp is that a “good” blood sugar is a blood sugar that is executed and documented. Documentation of all blood glucose readings is essential so that the camp doctor can review the numbers for each camper in order to make recommendations for the next insulin dose. Likewise, any low blood sugar treatment should be recorded as it also gives essential information, along with insulin doses administered each day. Each camp has a different system for record keeping but one common way to handle record-keeping is to keep a cabin group in a three-ring notebook and each camper will have an insulin administration record within that book that has a log for blood sugars, insulin administered and any treatments throughout the day. Many camps will have “reaction slips” that counselors carry in belt packs, along with blood glucose meters and treatments supplies so that, during activities, if a camper feels low, they check blood sugar level, treat if necessary and document both th reading and the treatment (and of course the name and time) on the reaction slip. Then, the next time they are with the health care team and the cabin book, they will transcribe that information into the camper’s permanent insulin administration log. Blood sugar levels at camp vary based on activity levels. Activities that are strenuous cause blood sugars to be lower (like basketball, running, soccer) while activities that are sedentary (arts & crafts, music) will have the opposite effect, causing blood sugars to rise. Likewise, a rainy day can cause the entire camp to have high blood sugars because the campers may have been “dosed” for a regular activity day that was spoiled by weather. All of these variations need to be taken into consideration when making choices about insulin dose. Reducing insulin before a strenuous hike, and/or increasing food, will help to prevent low blood sugar. Likewise, increasing insulin dose and not serving high carbohydrate foods on a rainy day, will help to minimize high blood sugar. Save the pizza for dance night! Stressful events may also have an effect on blood sugar and while stress tends to raise blood sugar in most people with diabetes, this is not always true. Monitoring blood glucose is the only way to be sure – so checking blood sugar levels during stressful events, or when a camper is feeling emotional or sick is essential. Food and meal planning is a really big part of diabetes mangement. It’s hard to know whether a camper is going to like what is being served and whether they are going to eat all of their meal. Some camps give insulin after the meal because of this. Others split the dose, giving half before and half after. This complicates insulin administration for the health care team but makes judgment about doses easier. Your camp will set its own policy in this regard. The most important thing is to know what your campers eat. How many carbohydrates did they ingest – because the insulin dose must be based on that campers “insulin-to-carbohydrate ratio” (number of units of insulin needed to cover set amount of carbohydrate, for instance 1-10 or 1-15). Blood glucose monitoring time is a great time for education. Health care team members or camp staff can discuss blood sugars and the effects of food and activity with the camper, sharing insights about why blood sugars may have been in or out of range. It is a good time to teach campers a new step in diabetes management – changing a pump site, taking an injection on their own, pricking their finger for the first time. It is also a time to impress upon each camper that blood sugar numbers are not “good” or “bad” as this places a burden of guilt upon the camper – rather, blood sugar numbers are information that can be used to make informed decisions on how to adjust insulin doses for the next administration time. At camp, the burden of diabetes should be removed, as much as possible, so that campers feel motivated to tackle the challenges of diabetes’ variability. Treatment protocol for low blood sugar varies from camp to camp. If a camper is able to take something by mouth, camps will typically treat with a fast-acting carbohydrate (glucose tabs, juice box, glucose gel), wait 15 minutes and then check blood sugar again. If the blood sugar has returned to normal range, some camps will follow with a complex carbohydrate/protein/fat snack (cheese crackers, granola bar) to ensure the blood sugar is maintained. If the blood sugar is still low, the treatment with fast-acting carbohydrate would be repeated and the same process followed until the blood sugar returned to normal. If there is a low blood sugar and the camper is unable to take treatment by mouth, this is an emergency and the health care team must be called immediately (see Emergency Treatment and Glucagon video). If blood sugar is high (on scheduled check or if a camper verbalizes symptoms) – over 240 is standard but adhere to your camp’s policy – a ketone check is important. Ketones are the body’s result of burning its own fat instead of glucose for fuel. Your camp will have procedures based on the result of the ketones test. In some cases, high blood sugars with ketones will necessitate that the camper be taken to the health care center to receive a correction dose of insulin (and/or to have his/her pump site checked to make sure its functioning properly) and to drink fluids to help hydrate the camper and rid the body of the ketones. With large ketones, activity may not be recommended as this may cause ketones to increase. In other cases, if the ketones are small or if the blood sugar is high with no ketones, your camp policy may be to wait until the next scheduled insulin administration time to correct the blood sugar with an adjusted dose. In this case, regular activity may help to reduce the elevated blood sugar. Most camps require staff to carry a belt or back pack with all necessary supplies – blood glucose monitor, strips, lancets, alcohol swabs, cotton balls, documentation slips, fast-acting carbohydrate and complex carbohydrate. Many camps also have blood glucose checking stations set up around camp. Treatment for severe lows (glucagon, IV dextrose) is typically kept in the healthcare center and may be strategically placed in other areas of camp where trained health care team members will have access in the event of a severe low blood sugar. Your camp will have a specific policy/protocol on treatment of severe low blood sugar with which you should familiarize yourself.