Management and Control: Plague (Yersinia pestis)
advertisement

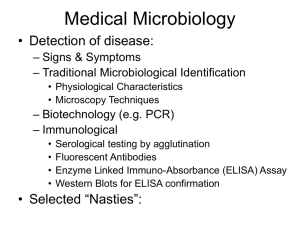
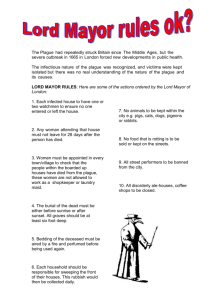
Management and Control: Plague (Yersinia pestis) IUCN SSC Invasive Species Specialist Group (ISSG) 1.0 GENERAL MANAGEMENT STRATEGIES 1.1 PREDICTING OUTBREAKS 2.0 PREVENTION 2.1 CHEMICAL CONTROL OF FLEA VECTORS FOR PREVENTION OF Y. PESTIS SPREAD 2.2 PLAGUE VACCINES 2.2.1 KILLED WHOLE CELL VACCINES 2.2.2 SUBUNIT BASED VACCINES 2.2.3 LIVE ATTENUATED STRAIN VACCINES 3.0 TREATMENT 3.1 HISTORICAL TREATMENT 3.2 ANTIBIOTIC TREATMENT 3.3 ALTERNATIVES TO ANTIBIOTICS 3.3.1 IMMUNOTHERAPY 3.3.2 NON-PATHOGEN-SPECIFIC IMMUNOMODULATORY THERAPY 3.3.3 PHAGE THERAPY 3.3.4 BACTERIOCIN THERAPY 3.3.5 INHIBITORS OF VIRULENCE FACTORS 1.0 GENERAL MANAGEMENT STRATEGIES “Outbreaks are usually tackled with a fire-fighting approach. Teams move into an infected area to kill fleas with insecticides, treat human cases, and give chemoprophylaxis to exposed people. Many experts have argued that this crisis management approach is insufficient as the outbreak is likely to be on the wane by the time action is taken. Informed, pre-emptive decisions about plague management and prevention before outbreaks occur would certainly be more sustainable and cost-beneficial” (Stenseth et al. 2008). 1.1 PREDICTING OUTBREAKS “Plague cannot be eradicated, since it is widespread in wildlife rodent reservoirs. Hence, there is a critical need to understand how human risks are affected by the dynamics of these wildlife reservoirs” (Stenseth et al. 2008). Humans and other susceptible mammals experience their greatest exposure risk during epizootic periods where disease spreads rapidly. Thus understanding the factors that lead to epizootics is highly important (Gage and Kosoy 2005). Climatic factors may be important in some areas (e.g. Cavanaugh 1971 in Gage and Kosoy 2005). Parmenter et al. (1999) proposed a trophic cascade hypothesis where increased precipitation caused greater plant and food production for rodents. Increased host rodent populations led to a greater likelihood of epizootics and human cases of Yersinia pestis (Parmenter et al. 1999 in Gage and Kosoy 2005). There have been other recent progresses, “such as development of rapid diagnosis tools (Chanteau et al. 2003), some challenging of accepted dogma about the dynamics of sylvatic plague in the United States (Webb et al. 2006) and in Central Asia (Begon et al. 2006), and the identification of predictive critical rodent abundance thresholds for plague in Kazakhstan (Davis et al. 2004). What is striking, though, is our lack of understanding of this high profile disease in even the best-studied foci, particularly in Africa: often, we do not even know the natural reservoir of the bacilli. The capacity of the plague bacillus to form permanent foci under highly diverse ecological conditions attests to its extraordinary adaptability. During its emergence in Central Asia, Y. pestis accumulated copies of insertion sequences rendering its genome highly plastic (Parkhill et al. 2001). The capacity to undergo genomic rearrangements may thus be an efficient means for the plague bacillus to adapt to new ecological niches. Y. pestis was, furthermore, recently shown to be able to acquire antibiotic resistance plasmids under natural conditions (Galimand et al. 1997; Guiyoule et al. 2001)” (Stenseth et al. 2008). 2.0 PREVENTION The Center for Disease Control (2002) states that the spread of Y. pestis in humans can be controlled by eliminating sources of food and shelter for rodents in and near homes, modifying homes to prevent rodent access, using insecticides in the home when Y. pestis has been detected in the rodent population, and using insect repellents containing N, N-diethyl-m-toluamide (DEET) on skin and repellents or appropriate insecticidal sprays containing permethrin on clothing. Travelers should avoid sick or dead animals or rodent nests and burrows, and whenever possible they should avoid visiting areas that have experienced recent plague epidemics or epizootics. Animal fleas vector Y. pestis so control measures should be taken around animals, such as treating domestic dogs and cats weekly with appropriate insecticides, avoiding direct contact with sick or dead rodents, handling severely ill cats with extreme caution (these animals should be examined by a veterinarian), and avoiding rodent nests and burrows. Hunters should always wear gloves when handling dead animals (Gage et al. 2001). Y. pestis is designated as a Class I notifiable disease because of its high fatality rate and its epidemic potential, thus it is subject to International Health Regulations. These regulations require that all suspected cases be reported to and investigated by public health authorities and that confirmed cases be reported to the World Health Organization (WHO) in Geneva, Switzerland. For more information on transmission, clinical signs, diagnosis, recommended action if plague is suspected, quarantine and disinfection, please see Factsheet Plague from the Institute for International Cooperation in Animal Biologics. 2.1 CHEMICAL CONTROL OF FLEA VECTORS FOR PREVENTION OF Y. PESTIS SPREAD In North America use of insecticidal dust in rodent burrows to control flea vectors is a common method used to control spread of Y. pestis, particularly during epizootics. Carbaryl or permethrin formulations have been used in the past successfully (Barnes et al. 1972; Beard et al. 1992 in Seery et al. 2003), although permethrin is no longer commercially available. Seery et al. (2003) tested the effectiveness of deltamethrin, a synthetic pyrethroid similar to permethrin. It was found to significantly reduce flea populations for at least 84 days following just one application, and even seemed to suppress an epizootic of plague. Wilder et al. (2008) highlight the importance of timing when using insecticidal dust to treat rodent burrows to maximize effectiveness. The two main flea vectors in prairie dogs Oropsylla hirsuta and O. tuberculata cynomuris reach their peak abundances in March and October respectively. Thus insecticidal application is likely to be the most effective when times to reduce the peak times for flea-borne transmission: late February and August-September. Resistance to deltamethrin has been recorded in a number of vector species, including fleas (e.g. Bossard et al. 1998 in Wilder et al. 2008). Thus it is important that insecticidal dust is used carefully, and that colonies are chosen based on risk of plague exposure to humans and conservation importance (Wilder et al. 2008). 2.2 PLAGUE VACCINES 2.2.1 KILLED WHOLE CELL VACCINES There are a number of different forms of vaccines against Y. pestis which continue to be developed. Killed whole cells (KWC) of Y. pestis have been used in plague vaccines as early as 1897 (Titball and Williamson 2001). A formalin-inactivated preparation known as Plague Vaccine USP was licensed for use in the United States until recently, but was withdrawn in 1999 and is no longer available (Morris 2007). Currently there is another KWC vaccine available but it is not licensed by the FDA (Morris 2007). “Data from animal and human investigations suggest that KWC vaccines are effective in preventing or ameliorating bubonic plague, but are not effective in preventing primary pneumonic plague” (Morris 2007). Killed whole cell vaccines also have the disadvantage that they often cause significant adverse reactions, particularly after booster injections, which are needed to maintain protection (Buller 1983 in Smiley 2008). 2.2.2 SUBUNIT BASED VACCINES Subunit vaccines containing Y. pestis proteins offer great promise for development of safe and effective protection against plague (Kummer et al. 2008). “For development of a subunit vaccine to plague, efforts have focused on two primary Y. pestis antigens (Ags), the outer capsule protein (F1-Ag), which is believed to help avoid phagocytosis and the low calcium response protein (lcrV) or V-Ag.” Much research is being conducted using these proteins, either in equal concentrations or as a fusion protein and different variations of these proteins (Cornelius et al. 2008). Vaccination with recombinant F1 likewise protects mice against aerosolized Y. pestis (Andrews et al. 1996 in Smiley 2008). “However F1-negative Y. pestis strains exist, so vaccines based solely on F1 may fail to protect against weaponized pneumonic plague” (Smiley 2008). Unlike F1, LcrV is critical for virulence. “Vaccination with purified LcrV protects mice against subcutaneous Y. pestis challenge, as does passive transfer of LcrV-specific antibodies. Vaccination with recombinant LcrV protects mice against aerosol challenge with either F1positive or F1-negative Y. pestis strains”. However “vaccines based on LcrV alone also may fail to protect against weaponized pneumonic plague, because pathogenic Yersinia species express LcrV variants that may not confer crossprotective immunity (Roggenkamp et al. 1997)” (Smiley 2008). Vaccines containing both F1 and LcrV will be more difficult for Y. pestis to overcome, and provide better protection than vaccines comprised of just one of these subunits (Williamson et al. 1995; Williamson et al. 1996 in Smiley 2008). A recombinant plague vaccine, rF1V, a fusion of the Y. pestis F1 capsular and V virulence proteins, was designed developed at the United States Army Medical Research Institute of Infectious Diseases (USAMRIID). The vaccine has been demonstrated to protect animals against aerosol challenge (Heath et al. 1998; Powell et al. 2005 in Morris 2007). Preliminary studies suggest that the vaccine is safe, well-tolerated and immunogenic (Morris 2007). Similarly the United Kingdom’s defense department demonstrated that an alum formulation of the Y. pestis F1 and LcrV proteins protects mice against pulmonary Y. pestis challenge (Williamson et al. 1997; Jones et al. 2000 in Smiley 2008). Although subunit vaccines comprised of F1 and LcrV proteins are well-tolerated and immunogenic in humans, they cannot be tested for efficacy because of ethical reasons against intentional infection of humans. These vaccines protect mice and cynomolgus macaques, but inconsistently do not adequately protect African green monkeys. There is currently no explanation for this observation, and it is unclear whether F1/LcrV-based vaccines will provide humans with effective protection as observed with cynomolgus macaques, or the inadequate protection observed in African green monkeys (Smiley 2008). “A number of approaches are underway to improve the efficacy of F1/LcrV-based vaccines (Titball and Williamson 2004). Some researchers are genetically modifying the antigens (Goodin et al. 2007; DeBord et al. 2006), while others are exploring the use of alternate adjuvants (Jones et al. 2006; Glynn et al. 2005; Eyles et al. 2000; Honko et al. 2006) and delivery platforms (Wang et al. 2004; Oyston et al.1995; Titball et al. 1997; Leary et al. 1997; Garmory et al. 2003; Yang et al. 2007; Palin et al. 2007; Chiuchiolo et al. 2006). These approaches are certainly promising” (Smiley 2008). Research has also gone into vaccines for some animal species. Prairie dogs (Cynomys spp.) are highly susceptible to Y. pestis, and plague outbreaks can totally eliminate colonies. Rocke et al. (2008-A) determined that groups immunized with recombinant raccoon poxvirus expressing the F1 antigen of Y. pestis incorporated into a palatable bait had higher survival rates than unimmunized control group. Vaccines for black-footed ferrets (Mustela nigripes) have also been developed based on the F1-V fusion protein. The vaccine protects against injection directly with Y. pestis and also plague contracted via ingestion of infected mice, a probably route for natural infection (Rocke et al. 2008-B). 2.2.3 LIVE ATTENUATED STRAIN VACCINES Live attenuated (avirulent) strains of Y. pestis have also been developed for use as vaccines (Meyer et al. 1974 in Gage et al. 2001). “Vaccines based on live attenuated organisms provide the theoretical advantage of simultaneously priming immunity against many antigens, thereby reducing opportunities for circumvention by weapons engineers” (Smiley 2008). However these vaccines can be unstable and may become virulent, sometimes killing experimental non-human primate test subjects (Meyer 1970; Meyer et al. 1974; Russell et al. 1995; Welkos et al. 2002 in Smiley 2008). “Safety concerns have limited enthusiasm for the development of live attenuated vaccines in the United States and Europe, where plague is uncommon and the risk of harm may outweigh the benefits of vaccination. However, live attenuated vaccines were administered to tens of millions of humans in Indonesia, Madagascar, and Vietnam, apparently without causing any deaths (Girard 1963)” (Smiley 2008). Currently the live attenuated Y. pestis strain EV76 is still available for use in Russia (Smiley 2008), but is not licensed by the FDA (Russell et al. 1995; Titball and Williamson 2001; Titball and Williamson 2004 in Morris 2007). Recently Blisnick et al. (2008) investigated the possibility of using Yersinia pseudotuberculosis as an oral live vaccine for Y. pestis. Y. pseudotuberculosis shares high genetic similarity with Y. pestis as well as being much less virulent, genetically more stable and deliverable orally. Protection given by Y. pseudotuberculosis Strain IP32680 was high (one inoculation 75%, two inoculations 88%). Another advantage is that if Y. pseudotuberculosis were to be accidently released into the environment it would be less problematic that Y. pestis. The final advantage of an oral inoculation is the avoidance of syringes, which the World Health Organization mentions as a major source of disease transmission in its vaccination guidelines (WHO 2003 in Blisnick et al. 2008). The authors conclude that “our results thus validate the concept that an attenuated Y. pseudotuberculosis strain can be an efficient, inexpensive, safe, and easy-to-produce live vaccine for oral immunization against bubonic plague.” However strain IP32680 cannot be used for human vaccination because the causes of its attenuation are unknown, and thus it could become pathogenic. More research is needed to develop live attenuated strains of Y. pseudotuberculosis which have defined, irreversible mutations (Blisnick et al. 2008). 3.0 TREATMENT “The main limitation of the prevention of plague by vaccination is that protection is delayed for at least 1 week after immunization, and this time may be crucial with respect to the lethal outcome of the disease (Butler, 1983; Dennis et al., 1999; Domaradskii, 1993, 1998; Inglesby et al., 2000; Lien-Teh et al., 1936; Naumov & Samoilova, 1992; Nikolaev, 1972; Perry & Fetherston, 1997; Pollitzer, 1954; Rudnev, 1940). As a consequence, antibiotics are employed for the early initiation of prophylaxis and therapy of plague” (Anisimov and Amoako 2006). Diagnosis must be made quickly due to the fast progression of the disease and the high mortality rate followed by appropriate antibiotic treatment (Eisen et al. 2007-A). An examination of sputum or a lymph node biopsy will reveal gram-negative, bipolar staining coccobacilli. In the United States, suspected cases of plague should be reported to state health departments, which in turn notify the Center for Disease Control (CDC). All cases subsequently confirmed by laboratory analysis are reported by CDC to WHO. 3.1 HISTORICAL TREATMENT “Until the nineteenth century, the treatment of plague was based on mysticism and superstition. Such ‘remedies’ as magic and talismans, mixtures of bird and animal blood, tablets made from rattlesnake meat, and even material squeezed from fresh horse dung, were widely used (Afanas’ev & Vaks, 1903). Later, methods such as phlebotomy, emetics, purgatives and diaphoretics were also applied to plague treatment (Rudnev, 1940). The isolation of the plague pathogen (Y. pestis), in 1894 (Yersin, 1894) made possible scientific approaches to the cure of plague infected patients. The local application of antiseptics such as iodine, mercuric chloride, carbolic acid or quinine, together with the incision or even searing of bubos, were promising in some cases, as were attempts to surmount severe systemic disease by the use of the same remedies, specific bacteriophages or animal hyperimmune sera (Lien-Teh et al., 1936; Rudnev, 1940); however, real success in plague therapy was observed when sulfanilamides (Carman, 1938) and then streptomycin (Hornibrook, 1946) became available” (Anisimov and Amoako 2006). 3.2 ANTIBIOTIC TREATMENT Cases of bubonic plague can often be successfully treated using antibiotic prophylaxis and therapy. Antibiotics used are usually streptomycin, tetracycline or chloramphenicol (Perry 1997 in Titball and Williamson 2001), which the World Health Organization Expert Committee on Plague name as the ‘gold standard’ treatment (Anisimov and Amoako 2006). Treatment must be quick and aggressive in order to be successful. Antibiotic treatment of septicemic and pneumonic plague is less successful because the disease develops rapidly, and treatment must begin during the early stages of infection. Gage et al. (2001) state that persons suspected of having pneumonic plague should be maintained under respiratory droplet precautions until 48 hours after antibiotic treatment begins. Persons who have confirmed cases of pneumonic plague should be kept under droplet precautions until sputum cultures are negative. Prophylactic antibiotics should be administered to persons who have had close exposure (6.5 feet or 2 metres) to persons suspected of having pneumonic plague. 3.3 ALTERNATIVES TO ANTIBIOTICS Recent detection of antibiotic resistant strains of Y. pestis indicate that antibiotics may not be a feasible for long-term use to treat plague (Galimand et al. 1997 in Titball and Williamson 2001) and has led to exploration of alternatives to antibiotics (Anisimov and Amoako 2006). These include immunotherapy, non-pathogen-specific immunomodulatory therapy, phage therapy, bacteriocin therapy, and treatment with inhibitors of virulence factors as reviewed in Anisimov and Amoako (2006). 3.3.1 IMMUNOTHERAPY Serum therapy has been used since 1896 by A. Yersin and others. Serum therapy involves using the serum of vaccinated animals to cure infected patients. Treatment of bubonic plague obtained mildly successful results, but serum therapy is less successful against sepicemic and pneumonic forms. This type of therapy also frequently caused side effects of serum sickness and anaphylactic shock. In 1970, the WHO Expert Committee on Plague recommended the continuation of further development of plague antitoxic sera that might be used for the treatment of plague patients with severe toxicosis (WHO 1970 in Anisimov and Amoako 2006). Antibody therapy begun to be developed in the 1960s for preventing and treating infectious diseases. In contrast to older remedies based on animal sera, these specific immunoglobulins contained antibodies derived from immunized human donors, rather than animals, and so had minimal side effects. As well as limitations such as high cost, low availability and potential to transmit disease; therapy based on a single antibody against a single antigen or epitope will be ineffective in the case of infection with a virulent strain lacking the antigen or expressing a different serological variant of the antigen (Anisimov et al. 2004; Friedlander et al. 1995; Roggenkamp et al. 1997 in Anisimov and Amoako 2006). 3.3.2 NON-PATHOGEN-SPECIFIC IMMUNOMODULATORY THERAPY “Y.pestis is known to efficiently overcome the innate immune system of many mammals. However, it has been shown that neutrophils (Cavanaugh & Randall, 1959) and CD11c+ cells (Bosio et al., 2005), which represent the initial line of host defence against invading pathogens, play an important role in suppressing the initial replication and dissemination of inhaled Y. pestis” (Anisimov and Amoako 2006). Recent studies have shown that that granulocyte colony- stimulating factor, granulocytemacrophage colony-stimulating factor and interferon-c can augment the functional antimicrobial activities of neutrophils, and may be useful for plague therapy (Liles 2001 in Anisimov and Amoako 2006). Y. pestis causes septic shock which includes an inability to regulate the inflammatory response and is one of the major causes of death (Butler 1983; Dmitrovskii 1994; Van Amersfoort et al. 2003 in Anisimov and Amoako 2006). The group of cholesterol-lowering drugs known as statins which also have immunomodulatory and anti-inflammatory properties may have use in plague therapy. Studies show that simvastatin (Merx et al. 2004 in Anisimov and Amoako 2006) and cerivastatin (Ando et al. 2000 in Anisimov and Amoako 2006) pretreatment improve survival rates to sepsis. 3.3.3 PHAGE THERAPY Bacteriophages were first used to treat plague in 1925 by d’Herelle. Four patients with serious plague infectious were treated effectively by injection of the phage. This work led to a number of attempts to confirm the efficacy of the phage therapy in animal and clinical trials. However a poor understanding of phage-bacterial interactions and poorly designed trials led to conflicting results (Skurnik and Strauch 2006; Sulakvelidze, 2005; Summers, 1999, 2001 in Anisimov and Amoako 2006). Bacteriophages have received renewed attention lately as possible agents against bacterial pathogens. A number of recent trials have found that phage therapy can be effective, although treatment depends on the route and frequency of phage application (Skurnik and Strauch 2006; Sulakvelidze, 2005; Summers, 1999, 2001 in Anisimov and Amoako 2006). However there are a number of obstacles to use of phage to treat plague. These include phage resistance, possibility of phage mediated transfer of genetic material to bacterial hosts. A number of Y. pestis specific phage genomes have recently been sequenced, which could provide the basis for a revival in phage therapy for plague. A safer possibility than using live phage agents is therapeutic use of enzymes extracted from bacteriophages. A potential class of enzymes is endolysins, which have cell-wall-hydrolysing action against specific bacteria (Young 1992; Berchieri et al. 1991; Goode et al. 2003 in Anisimov and Amoako 2006). 3.3.4 BACTERIOCIN THERAPY Bacteriocins are bacterially produced antimicrobial peptides. Purified bacteriocins have potential to be used for reduction or elimination of pathogens, including plague (Braude and Siemienski; Riley and Wertz 2002 in Anisimov and Amoako 2006) and many have been successfully used against pathogens including Streptococcus dysgalactiae and Y. pseudotuberculosis. A purified bacteriocin NRRL-B- 30509 secreted by Paenibacillus polymyxa has shown to inhibit growth of Y. pestis in vitro (E. A. Svetoch and B. V. Eruslanov, personal communication in Anisimov and Amoako 2006) in doses similar to those recommended by the WHO Expert Committee on Plague (WHO, 1970 in Anisimov and Amoako 2006) for antibiotics. Currently the bacteriocin Gallidermin shows the most promise as a therapeutic agent, with relatively low cytotoxicity and potent antimicrobial activities (Maher & McClean, 2006 in Anisimov and Amoako 2006). 3.3.5 INHIBITORS OF VIRULENCE FACTORS “Microbial factors involved in the process of virulence are unique, in that their inhibition, by definition, should interfere with the process of infection rather than with bacterial viability. Inhibitors of such targets would be unlikely to affect host cells, to be cross-resistant to existing therapies, or to induce resistance themselves. Bacterial virulence may therefore offer unique opportunities to inhibit the establishment of infection or alter its course as a method of antimicrobial chemotherapy.” (Alksne, 2002; Lee et al. 2003; Marra, 2004 in Anisimov and Amoako 2006). One focus of current research into Y. pestis virulence factors is bacterial adhesins, which are responsible for adhesion to host surfaces which is a necessary step in successful colonization and disease production by pathogens. Short-chain oligosaccharides have potential anti-adhesion therapeutics (Thomas & Brooks 2004 in Anisimov and Amoako 2006). Also Ysc-Yop Type III weaponry which delivers effector proteins into cytosol of target cells is a major pathogenicity factor of Yersinia. Inhibitors specifically targeting type III secretion are becoming a research focus (Chen et al. 2003; Lee et al. 2003, 2005; Kauppi et al. 2003a,b; Nordfelth et al, 2005; Xie et al. 2004 in Anisimov and Amoako 2006). “Other possible targets for inhibiting Y. pestis virulence are quorum sensing (Suga & Smith 2003), the two-component regulatory systems (Oyston et al. 2000; Winfield et al. 2005) that govern virulence, and/or the enzymes for the biosynthesis of the LPS that is believed to determine antimicrobial-cationic-peptide (Anisimov et al. 2005; Bengoechea et al. 1998) and serum resistance (Anisimov et al. 2005; Porat et al. 1995)” (Anisimov an Amoako 2006).
![[Presentation by Sara Morgans].](http://s2.studylib.net/store/data/005578977_1-95120715b429730785aca2fdba9a2208-300x300.png)