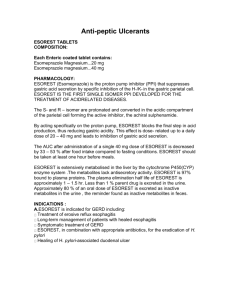
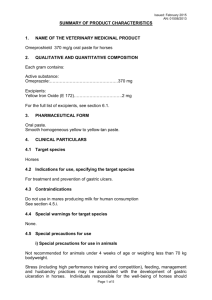
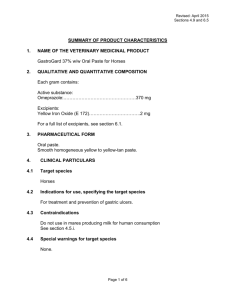
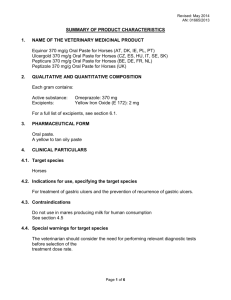
OMEPRAZOLE
advertisement

OMEPRAZOLE 0.0 Overview 1) Class a) This drug is a member of the following class(es): - Antiulcer - Gastrointestinal Agent - Proton Pump Inhibitor 2) Dosing Information a) Adult 1) Duodenal ulcer disease, Active a) 20 mg ORALLY once daily for 4 to 8 wks (Prod Info PRILOSEC(R) delayed release capules, 2005) 2) Duodenal ulcer disease, Dual therapy; Adjunct - Helicobacter pylori gastrointestinal tract infection, Dual therapy; Adjunct a) 40 mg ORALLY daily (with clarithromycin combination therapy) for 14 days (Prod Info PRILOSEC(R) delayed release capules, 2005) b) ulcer present at initiation of therapy, 40 mg ORALLY daily (with clarithromycin combination therapy) for 14 days, then 20 mg ORALLY for 14 days (Prod Info PRILOSEC(R) delayed release capules, 2005) 3) Duodenal ulcer disease, Triple therapy; Adjunct - Helicobacter pylori gastrointestinal tract infection, Triple therapy; Adjunct a) 20 mg ORALLY (in combination with clarithromycin 500 mg and amoxicillin 1000 mg) twice daily for 10 days (Prod Info PRILOSEC(R) delayed release capules, 2005) b) ulcer present at initiation of therapy, 20 mg ORALLY (in combination with clarithromycin 500 mg and amoxicillin 1000 mg) twice daily for 10 days followed by 20 mg ORALLY daily for 18 days (Prod Info PRILOSEC(R) delayed release capules, 2005) 4) Erosive esophagitis, To maintain healing; Prophylaxis - Gastroesophageal reflux disease, To maintain healing; Prophylaxis a) maintenance, 20 mg ORALLY once daily (Prod Info PRILOSEC(R) delayed release capules, 2005) 5) Erosive esophagitis - Gastroesophageal reflux disease a) 20 mg ORALLY daily for 4 to 8 wks (Prod Info PRILOSEC(R) delayed release capules, 2005) 6) Gastric hypersecretion a) initial, 60 mg ORALLY once daily, may increase up to 120 mg 3 times daily; doses greater than 80 mg/day should be administered in divided doses (Prod Info PRILOSEC(R) delayed release capules, 2005) 7) Gastric ulcer, Active, benign a) 40 mg ORALLY once daily for 4 to 8 wks (Prod Info PRILOSEC(R) delayed release capules, 2005) 8) Gastroesophageal reflux disease, Symptomatic a) 20 mg ORALLY once daily for up to 4 wks (Prod Info PRILOSEC(R) delayed release capules, 2005) 9) Stress ulcer; Prophylaxis a) initial, 40 mg NG or ORALLY (American Society of Health-System Pharmacists, 1999) b) maintenance, 20 to 40 mg NG or ORALLY once a day (American Society of Health-System Pharmacists, 1999). b) Pediatric 1) Safety not established in pediatric patients 2) Erosive esophagitis, To maintain healing; Prophylaxis - Gastroesophageal reflux disease, To maintain healing; Prophylaxis a) 2 y and older, less than 20 kg, 10 mg ORALLY daily (Prod Info PRILOSEC(R) delayed release capules, 2005) b) 2 y and older, 20 kg or greater, 20 mg ORALLY daily (Prod Info PRILOSEC(R) delayed release capules, 2005) 3) Erosive esophagitis - Gastroesophageal reflux disease a) 2 y and older, less than 20 kg, 10 mg ORALLY daily for 4 to 8 wks (Prod Info PRILOSEC(R) delayed release capules, 2005) b) 2 y and older, 20 kg or greater, 20 mg ORALLY daily for 4 to 8 wks (Prod Info PRILOSEC(R) delayed release capules, 2005) 4) Gastroesophageal reflux disease, Symptomatic a) 2 y and older, less than 20 kg, 10 mg ORALLY once daily for 4 wks (Prod Info PRILOSEC(R) delayed release capules, 2005) b) 2 y and older, 20 kg or greater, 20 mg ORALLY once daily for 4 wks (Prod Info PRILOSEC(R) delayed release capules, 2005) 5) Stress ulcer; Prophylaxis a) 0.5 mg/kg NG or ORALLY every 12 h; may require 0.5 mg/kg ORALLY every 6-8 h to maintain pH greater than 4-5 (Kaufman et al, 2002) 3) Contraindications a) Hypersensitivity to omeprazole or to any of its components (Prod Info Prilosec(R), 2001) 4) Serious Adverse Effects a) Hepatotoxicity b) Hip fracture c) Interstitial nephritis d) Pancreatitis 5) Clinical Applications a) FDA Approved Indications 1) Duodenal ulcer disease, Active 2) Duodenal ulcer disease, Dual therapy; Adjunct - Helicobacter pylori gastrointestinal tract infection, Dual therapy; Adjunct 3) Duodenal ulcer disease, Triple therapy; Adjunct - Helicobacter pylori gastrointestinal tract infection, Triple therapy; Adjunct 4) Erosive esophagitis, To maintain healing; Prophylaxis - Gastroesophageal reflux disease, To maintain healing; Prophylaxis 5) Erosive esophagitis - Gastroesophageal reflux disease 6) Gastric hypersecretion 7) Gastric ulcer, Active, benign 8) Gastroesophageal reflux disease, Symptomatic 9) Stress ulcer; Prophylaxis 1.0 Dosing Information 1.1 Drug Properties A) Information on specific products and dosage forms can be obtained by referring to the Tradename List (Product Index) B) Synonyms - Omeprazole C) Physicochemical Properties 1) Molecular Weight a) 345.42 (Canada, 1997) 2) pKa a) 4 and 8.8 1.2 Storage and Stability A) Preparation 1) Oral route a) ORAL SUSPENSION PREPARATION 1) For the preparation of the powder for suspension, empty packet into a cup containing 2 tablespoons of WATER. DO NOT USE OTHER LIQUIDS OR FOODS. Stir well and administer immediately. Refill cup with water and administer (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006) B) Oral route 1) The stability of omeprazole is a function of pH; it undergoes rapid degradation in an acidic medium, but has an acceptable stability under alkaline conditions (Prod Info Prilosec(R), 2001a). 2) The delay-released capsules of omeprazole should be stored between 59 to 86 degrees Fahrenheit (15 to 30 degrees Centigrade) in a tight container protected from light and moisture (Prod Info Prilosec(R), 2001a). The powder for oral suspension should be stored between 68 to 77 degrees Fahrenheit (25 degrees Centigrade) with excursions permitted to 59 to 86 degrees Fahrenheit (15 to 30 degrees Centigrade) (Prod Info Zegerid(TM), 2004). C) Extemporaneous Formulation - Oral route 1) The following is the compounding procedure used for the extemporaneous oral omeprazole liquid formulation when a fraction of a dose (ie, 20-milligram omeprazole capsule) is required (Woods & McClintock, 1993; Gunasekaran & Hassall, 1993): (1) Open one capsule (ie, Prilosec(R)) and weigh the contents. (2) Determine how many pellets are required for the recommended dose. (3) Repack the pellets into gelatin capsules. Protect capsules from moisture. Suggest relabeling the original bottle or using a glass or high-density polyethylene container with a tight closure and a desiccant. (4) Immediately prior to administration, mix the intact pellets with an acidic beverage (pH less than 5.3). In one clinical trial, the pellets were mixed with orange juice, cranberry juice, or yogurt to the fasting patient. An acidic beverage will help preserve the integrity of the pellet coat. 2) Patients should be instructed not to chew the granules in the vehicle. Since the stability of repacked omeprazole is unknown, one institution has recommended a maximum shelf-life of 7 days (Woods & McClintock, 1993). Bioequivalent studies have not been performed on the described extemporaneous omeprazole formulation. 3) The following procedure may be used for compounding oral omeprazole 2 milligrams/milliliter liquid (Quercia et al, 1997): (1) Empty five 20-milligram omeprazole capsules in the barrel of a 60-milliliter (mL) polypropylene Luer-Lok syringe with needle attached (2) Place plunger back in the barrel (3) Draw up 50 mL of 8.4% sodium bicarbonate (4) Remove needle and attach a fluid-dispensing connector (5) Attach a second Luer-Lok syringe to the other end of the fluid-dispensing connector (6) Transfer the omeprazole-sodium bicarbonate liquid back and forth until the granules are completely dissolved (7) Transfer the liquid into one syringe and disconnect the rest. This liquid can be transferred back into the empty 50-mL sodium bicarbonate vial (8) The liquid is stable for up to 14 days at 24 degrees Centigrade (C) and for up to 30 days at 5 and -20 degrees C when stored in this vial 1.3 Adult Dosage 1.3.1 Normal Dosage A) Intravenous route 1) Duodenal ulcer disease, Active a) The use of intravenous omeprazole has been extremely limited. In the treatment of duodenal ulcers, 160 milligrams intravenous omeprazole daily (every 8 hours as 80 milligrams/40 milligrams/40 milligrams) was required to decrease 24-hour intragastric acidity by 97%. This compares with 30 milligrams oral omeprazole daily (Walt et al, 1985). 2) Gastric hypersecretion a) Intravenous omeprazole, in a dose of 60 milligrams every 8 hours, has been used successfully in acute Zollinger-Ellison syndrome, followed by oral maintenance therapy of 90 milligrams omeprazole twice, then once, daily (Blanchi et al, 1982a). 3) Gastrointestinal hemorrhage a) After hemostasis of bleeding peptic ulcers, a regular dose of OMEPRAZOLE 20 milligrams (mg)/day intravenously (IV) for 3 days (total=60 mg; n=73) was as successful in preventing re-bleeding as the high doses regimen - 80 mg loading dose by IV bolus followed by 8 mg/hour IV for 72 hours (total=652 mg; n=69) (Udd et al, 2001). B) Jejunum route 1) OMEPRAZOLE suspension 40 milligrams provided adequate gastric pH control (pH maintained above 4.0) when administered by JEJUNAL TUBE, DUODENAL TUBE, OR NASOGASTRIC TUBE in critically ill surgical patients (surgical intensive care unit patients with mechanical ventilation and NPO status; n=9). All subjects were considered at-risk for stress ulcers. Omeprazole by each of the 3 routes maintained 24-hour gastric pH above 4.0. The suspension was prepared by dissolving the contents of two 20-mg capsules in 20 mL of 8.4% sodium bicarbonate. The drug had a slower time-to-peak and a lower maximum concentration when given by the nasogastric route compared with administration via a duodenal or jejunal tube; however, the area under the plasma-concentration curve (AUC) was not significantly different for administration via nasogastric tube or duodenal/jejunal tube (Phillips et al, 2001). 2) Omeprazole pellets administered through a jejunostomy tube has been successful in one institution. Omeprazole pellets were crushed then added to a sodium bicarbonate 8 millimoles/50 milliliter solution. Upon mixing, the solution was shaken to form a stable suspension. The resultant suspension is then flushed through a jejunostomy tube (Woods & McClintock, 1993; Gunasekaran & Hassall, 1993a). C) Nasogastric route 1) SUMMARY a) The immediate-release powder for oral suspension should be reconstituted with approximately 20 milliliters of water only. No other liquids or foods should be used. After instilling the suspension in the tube, it should be washed through with another 20 milliliters of water (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006). b) Various techniques have been successfully used to administer intact omeprazole granules through a nasogastric (NG) tube. These studies have documented statistically significant increases in intragastric pH after NG administration of omeprazole. However, these techniques have not been standardized, nor have direct comparative studies been conducted to determine the efficacy of omeprazole administered through the NG tube. 2) OMEPRAZOLE suspension 40 milligrams provided adequate gastric pH control (pH maintained above 4.0) when administered by JEJUNAL TUBE, DUODENAL TUBE, OR NASOGASTRIC TUBE in critically ill surgical patients (surgical intensive care unit patients with mechanical ventilation and NPO status; n=9). All subjects were considered at-risk for stress ulcers. Omeprazole by each of the 3 routes maintained 24-hour gastric pH above 4.0. The suspension was prepared by dissolving the contents of two 20-mg capsules in 20 mL of 8.4% sodium bicarbonate. The drug had a slower time-to-peak and a lower maximum concentration when given by the nasogastric route compared with administration via a duodenal or jejunal tube; however, the area under the plasma-concentration curve (AUC) was not significantly different for administration via nasogastric tube or duodenal/jejunal tube (Phillips et al, 2001). 3) Omeprazole has been administered via a nasogastric (NG) tube for the prevention of STRESS-RELATED MUCOSAL DAMAGE in ventilated, critically ill patients. The contents of one or two 20-milligrams omeprazole capsules were poured into a syringe. Ten to 20 milliliters of an 8.4% sodium bicarbonate solution was withdrawn in the syringe. Thirty minutes were allowed for the enteric-coated omeprazole granules to break down. The resulting milky substance was shaken prior to administration. The NG tube was then flushed with 5 to 10 milliliters of water then clamped for at least 1 hour. Patients received omeprazole 40 milligrams (mg) once, then 40 mg 6 to 8 hours later, then 20 mg once daily using this technique (Prod Info Prilosec(R), 1998). A similar nasogastric administration approach (omeprazole with 8.4% sodium bicarbonate) has been used successfully in another study (Lasky et al, 1998). 4) Another study used a different technique. The omeprazole capsule (20 or 40 milligrams (mg)) was opened, then the intact granules were poured into a container holding 30 milliliters (mL) of water. With the plunger removed, 1/3 to 1/2 of the granules were then poured into a 30-mL syringe which was attached to a nasogastric tube (NG). The plunger was replaced with 1 centimeter of air between the granules and the plunger top while the plunger was depressed. This process was repeated until all the granules were flushed, then a final 15 mL of water was flushed through the tube. Patients who received omeprazole 40 mg in this manner had a more predicable increase in intragastric pH than patients who received omeprazole 20 mg (Prod Info Prilosec(R), 1998). 5) The bioavailability and gastric acid suppression of omeprazole administered orally is equal to omeprazole administered through the nasogastric tube. In this study, nasogastric (NG) administration of Prilosec(R) was prepared as follows: (1) The granules were removed from the capsules and placed in a small dry cup; (2) Six to 10 granules were flushed through the NG tube with 10 to 20 milliliters of water; a total of 140 milliliters was used (Larson et al, 1996). D) Oral route 1) Duodenal ulcer disease a) To reduce the incidence of duodenal ulcer recurrence, the manufacturer recommends combining omeprazole with clarithromycin. The recommended dosage is omeprazole 40 milligrams once daily plus clarithromycin 500 milligrams 3 times daily for days 1 through 14. For days 15 through 28, only omeprazole is recommended and the dosage should be reduced to 20 milligrams once daily (Prod Info Prilosec(R), 2001a). b) HELICOBACTER PYLORI - DUAL THERAPY 1) SUMMARY a) Omeprazole, with clarithromycin, is approved for treating patients with H pylori infection and duodenal ulcer disease. Therapy will continue from 14 to 28 days depending on if an ulcer is present at initiation of therapy. In patients who fail therapy, dual therapy with clarithromycin is more likely to be associated with clarithromycin resistance than triple-drug therapy (Prod Info Prilosec(R), 2001a). 2) The following dual-drug regimen is approved for treating H pylori infection: omeprazole 40 milligrams(mg) once daily and clarithromycin 500 mg 3 times daily. Continue regimen for 14 days. In patients who present with an ulcer at the initiation of therapy, an additional 14 days of omeprazole 20 mg once daily is recommended for ulcer healing and symptom relief (Prod Info Prilosec(R), 2001a). It appears that omeprazole-containing triple-drug regimens are more effective than omeprazole-containing dual-drug regimens (Prod Info Prilosec(R), 2001a; Prod Info Prilosec(R), 1998). 3) Omeprazole 20 milligrams twice daily or 40 milligrams once daily in combination with clarithromycin 500 milligrams three times daily for 14 days is effective in patients with HELICOBACTER PYLORI infections. Eradication rates at these dosages range between 72% to 84% (Markham & McTavish, 1996). HIGHER cure rates are observed with omeprazole 40 milligrams once daily as compared to the 20 milligrams twice daily dosage (Soll, 1996). c) A 4-day triple regimen consisting of lansoprazole (LAN), azithromycin (AZITH) and tinidazole (TIN) was as effective as a 1-week regimen of omeprazole (OMEP), clarithromycin (CLAR), and TIN in curing H pylori infections in patients with active or non- active duodenal or gastric ulcers. The eradication rates for these 2 regimens were 78.7% and 83.7%, respectively. Doses used in this study were as follows: First regimen, LAN 30 mg twice daily on days 1 through 4, AZITH 500 mg once daily on days 2 through 4, and TIN 2000 mg for 1 dose on day 3; Second regimen, OMEP 20 mg once daily, CLAR 250 mg twice daily and TIN 500 mg twice daily on days 1 through 7 (Trevisani et al, 1998). 2) Duodenal ulcer disease, Active a) SUMMARY 1) Omeprazole is indicated for the short-term treatment of active duodenal ulcers. The recommended dose is omeprazole 20 milligrams (mg) once daily for 4 weeks. Some patients may require an additional 4 weeks of therapy (Prod Info PRILOSEC(R) delayed release capules, 2005; Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006). The delayed-release capsule should be taken on an empty stomach before meals (Prod Info PRILOSEC(R) delayed release capules, 2005). The immediate-release capsules and oral suspension should be taken 1 hour before a meal (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006). 2) For patients with Helicobacter pylori and active duodenal ulcer, the combination of omeprazole and clarithromycin is recommended. The recommended dosage for this combination regimen is omeprazole 40 mg once daily and clarithromycin 500 mg 3 times daily for days 1 through 14. For days 15 through 28, in patients with an ulcer present at the time of treatment initiation, discontinue clarithromycin and continue omeprazole at 20 mg once daily (Prod Info PRILOSEC(R) delayed release capules, 2005). b) Omeprazole 40 milligrams by mouth once daily was effective in the management of GIANT DUODENAL ULCER disease in a prospective study involving adult patients. Of the 27 patients receiving omeprazole therapy, 7 required subsequent surgery for ulcer complications or omeprazole failure, and 20 (71.4%) did not require surgical intervention. Among the 20 patients not requiring surgery, 15 demonstrated endoscopic evidence of ulcer healing, with most (12 of 15) occurring in 6 weeks (Fischer et al, 1999). c) Clinical studies have shown that eradicating Helicobacter pylori will prevent ulcer relapse and rebleeding in both duodenal and gastric ulcers. Patients with documented H pylori infection should receive therapy for the eradication of this organism (Rosengren & Polson, 1996a; Bianchi Porro et al, 1996c; Labenz & Borsch, 1993; Bell & Powell, 1993; Graham et al, 1993; Rokkas et al, 1993). d) The manufacturer does not recommend omeprazole for maintenance therapy of duodenal ulcers; however, omeprazole 20 milligrams once daily for 6 months has been shown to be safe and effective for maintenance therapy (ie, relapse rate, 3.8%) in healed duodenal ulcers (Prod Info Prilosec(R), 2001b); (Di Mario, 1996b). e) REFRACTORY DISEASE 1) Omeprazole 40 milligrams/day for 8 weeks has been highly effective in healing refractory peptic ulcers. Approximately 5% of peptic ulcers are unresponsive following the administration of H2antagonists at standard doses (Soll, 1996e; Skoutakis et al, 1995f; Anon, 1991aa). 2) Omeprazole 40 to 60 milligrams once daily was effective in healing refractory ulcers involving the duodenum, stomach, and esophagus in an uncontrolled study. Approximately 95% of patients responded to 40 milligrams/day and an additional 2% of patients responded to 60 milligrams/day. Patients had previously received ranitidine 450 to 600 milligrams/day for 3 months or greater (Soll, 1996e; Skoutakis et al, 1995f; Brunner et al, 1988). 3) Duodenal ulcer disease - Helicobacter pylori gastrointestinal tract infection a) A successful dosage regimen consisted of RANITIDINE BISMUTH CITRATE 400 milligrams (mg) twice daily on days 1 to 5 plus amoxycillin 1 gram twice daily, clarithromycin 500 mg twice daily, and metronidazole 500 mg twice daily on days 3 to 5 (the latter 3 drugs plus ranitidine bismuth citrate for 3 days). This regimen produced a 98% healing rate for duodenal ulcers and a 95% eradication rate for H. pylori (intention to treat). The ranitidine bismuth citrate combination therapy (n=56) was superior to a 10-day course of omeprazole, amoxycillin, and clarithromycin (n=55) for eradication of H pylori (p=0.042) (Catalano et al, 2000a). 4) Erosive esophagitis, To maintain healing; Prophylaxis Gastroesophageal reflux disease, To maintain healing; Prophylaxis a) SUMMARY 1) Omeprazole is indicated to maintain healing of erosive esophagitis. The recommended dose is 20 milligrams daily. Clinical efficacy studies do not extend beyond 12 months (Prod Info PRILOSEC(R) delayed release capules, 2005; Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006). The delayed-release capsule should be taken on an empty stomach before meals (Prod Info PRILOSEC(R) delayed release capules, 2005). The immediaterelease capsule and oral suspension should be taken 1 hour before a meal (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006). b) Omeprazole is indicated for the short-term treatment (4 to 8 weeks) and for the maintenance therapy (up to 12 months) of erosive esophagitis (Prod Info PRILOSEC(R) delayed release capules, 2005; Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006). For maintenance therapy, omeprazole is indicated for severe erosive or complicated ESOPHAGITIS grade 3 or above, or for grade 2 or greater in patients who have had at least 1 relapse (Skoutakis et al, 1995f; Dent et al, 1986a; Hetzel et al, 1986; Dammann et al, 1986b). The recommended oral dose is 20 milligrams daily (Hallerback et al, 1994; Dent et al, 1994a; Cucchiara et al, 1993a). Controlled studies have not evaluated the efficacy or safety of omeprazole in the maintenance healing of erosive esophagitis beyond 12 months (Prod Info PRILOSEC(R) delayed release capules, 2005; Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006). c) In intellectually disabled individuals, maintenance omeprazole therapy of 20 milligrams once daily for 3 months is effective in preventing relapse. Initially, these patients with grade I to IV reflux esophagitis were treated for 3 months with once daily omeprazole 40 milligrams (Bohmer et al, 1997a). 5) Erosive esophagitis - Gastroesophageal reflux disease a) SUMMARY 1) Omeprazole is indicated for the short-term treatment of erosive esophagitis that has been diagnosed endoscopically. The recommended dose is 20 milligrams daily for 4 to 8 weeks (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005). Patients who do not respond to 8 weeks of treatment may require an additional 4 weeks of treatment. If there is a recurrence of erosive esophagitis, an additional 4- to 8-week course of omeprazole may be considered (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005). The delayed-release capsule should be taken on an empty stomach before meals (Prod Info PRILOSEC(R) delayed release capules, 2005). The immediate-release capsule and oral suspension should be taken 1 hour before a meal (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006). 2) Omeprazole is indicated for the maintenance of healing of erosive esophagitis. The recommended dose is 20 milligrams daily (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005). b) Approximately 39% of patients with symptomatic esophagitis and endoscopically diagnosed erosive esophagitis of grade 2 or greater will respond to once daily omeprazole 20 milligrams. By week 8, the response rate is 74%. Higher omeprazole doses (eg, 40 milligrams once daily) are NOT statistically or clinically better than the 20 milligrams once daily dose in the treatment of esophagitis (Prod Info Prilosec(R), 2001b). c) Omeprazole 20 milligrams once daily (before breakfast) effectively resolved symptoms (ie, HEARTBURN, DYSPHAGIA, and ACID REGURGITATION) in 64% of patients with grades 0 through 4 erosive esophagitis. In this study, patients with gastroesophageal reflux disease (GERD) who were still symptomatic after 8 weeks of ranitidine therapy were treated with 8 weeks of omeprazole therapy. Gastrointestinal side effects were reported in 31% of patients (Richter et al, 1996b). d) High daily doses of omeprazole (40 milligrams) have been successfully used in intellectually disabled individuals with grade I to IV reflux esophagitis. These patients were initially treated for a total of 3 months; maintenance doses were used for an additional 3 months. Higher doses were used because this patient population generally has a poor response to lower doses. In addition, they often present with more severe esophagitis than the general population with GERD (Bohmer et al, 1997a). e) REFRACTORY DISEASE 1) Omeprazole 40 to 60 milligrams once daily was effective in healing refractory ulcers involving the duodenum, stomach, and esophagus in an uncontrolled study. Approximately 95% of patients responded to 40 milligrams/day and an additional 2% of patients responded to 60 milligrams/day. Patients had previously received ranitidine 450 to 600 milligrams/day for 3 months or greater (Soll, 1996e; Skoutakis et al, 1995f; Brunner et al, 1988). 6) Esophageal stricture a) Omeprazole 20 milligrams daily in combination with dilation is effective in patients with chronic benign esophageal strictures. In one clinical trial, patients treated with omeprazole had complete resolution of their strictures as demonstrated by endoscopy and esophagography (Silvis et al, 1996a). 7) Gastric hypersecretion a) SUMMARY 1) Omeprazole is indicated for the long-term treatment of pathological hypersecretory conditions such as ZOLLINGER-ELLISON SYNDROME, MULTIPLE ENDOCRINE ADENOMAS and SYSTEMIC MASTOCYTOSIS. The usual recommended starting dose is 60 milligrams (mg) once daily. Treatment with omeprazole in this patient population should be individualized based on the condition and response to treatment. Doses as high as 120 mg three times a day have been used. For patients requiring more than 80 mg/day, the total daily dose should be given in divided doses (Prod Info PRILOSEC(R) delayed release capules, 2005). b) Individualization of omeprazole dosing can be achieved by monitoring the basil acid output (BAO). The dose of omeprazole should be titrated upwards until acid secretion (ie, basil acid output) is less than 10 milliequivalents/hour. Once Zollinger-Ellison syndrome is under control with omeprazole therapy, a systematic reduction in dose to a maintenance dose of 20 milligrams once to twice daily is suggested (Maton, 1996a; Lamers, 1986; Bardram & Stadil, 1986; Delchier et al, 1986a; McArthur et al, 1985; Lamers et al, 1984a). 8) Gastric ulcer a) A 4-day triple regimen consisting of lansoprazole (LAN), azithromycin (AZITH) and tinidazole (TIN) was as effective as a 1-week regimen of omeprazole (OMEP), clarithromycin (CLAR), and TIN in curing H pylori infections in patients with active or non- active duodenal or gastric ulcers. The eradication rates for these 2 regimens were 78.7% and 83.7%, respectively. Doses used in this study were as follows: First regimen, LAN 30 mg twice daily on days 1 through 4, AZITH 500 mg once daily on days 2 through 4, and TIN 2000 mg for 1 dose on day 3; Second regimen, OMEP 20 mg once daily, CLAR 250 mg twice daily and TIN 500 mg twice daily on days 1 through 7 (Trevisani et al, 1998). 9) Gastric ulcer, Active, benign a) SUMMARY 1) Omeprazole is indicated for the short-term treatment of active benign gastric ulcers. The recommended dose is 40 milligrams/day for 4 to 8 weeks . After 8 weeks of therapy, the reported gastric ulcer healing rate is approximately 83% to 91% (Prod Info PRILOSEC(R) delayed release capules, 2005; Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Anon, 1996); (Anon, 1996a). b) The usual oral adult dose of omeprazole for the treatment of duodenal, gastric, jejunal, or esophageal ULCERS is 20 or 30 milligrams once daily before breakfast (Adams et al, 1988a; Clissold & Campoli-Richards, 1986b; Bader et al, 1986a; Huttemann et al, 1986; Pounder et al, 1986a; Prichard et al, 1985a; Lauritsen et al, 1985a; Prichard et al, 1985a; Gustavsson et al, 1983a). Maintenance therapy with 10 milligrams/day may be suitable for the management of PEPTIC ULCERS (Adams et al, 1988a); however, the safety and efficacy of this usage have not been established. c) Patients with GASTRIC ULCERS may require 4 to 8 weeks of therapy (Prod Info Prilosec(R), 2001b; Clissold & Campoli-Richards, 1986b; Darle et al, 1986; Huttemann, 1986a; Classen et al, 1985b). Longer durations of therapy may be required for patients with particularly large ulcers or for patients with duodenal ulcers who smoke (Clissold & Campoli-Richards, 1986b; Darle et al, 1986; Classen et al, 1985b; Prichard et al, 1985a; Naesdal et al, 1985). d) REFRACTORY DISEASE 1) Omeprazole 40 to 60 milligrams once daily was effective in healing refractory ulcers involving the duodenum, stomach, and esophagus in an uncontrolled study. Approximately 95% of patients responded to 40 milligrams/day and an additional 2% of patients responded to 60 milligrams/day. Patients had previously received ranitidine 450 to 600 milligrams/day for 3 months or greater (Soll, 1996e; Skoutakis et al, 1995f; Brunner et al, 1988). 10) Gastroesophageal reflux disease, Symptomatic a) SUMMARY 1) The recommended adult oral dose for the treatment of patients with symptomatic GERD and no esophageal lesions is 20 mg daily for up to 4 weeks. The recommended adult oral dose for the treatment of patients with erosive esophagitis and accompanying symptoms due to GERD is 20 mg daily for 4 to 8 weeks. Patients who do not respond to 8 weeks of treatment may require an additional 4 weeks of treatment. If there's a recurrence of erosive esophagitis or symptomatic GERD, additional 4- to 8-week courses of omeprazole may be considered (Prod Info PRILOSEC(R) delayed release capules, 2005; Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006). The delayed-release capsule should be taken on an empty stomach before meals (Prod Info PRILOSEC(R) delayed release capules, 2005). The immediate-release capsule and oral suspension should be taken 1 hour before a meal (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006). b) After 28 days of treatment, OMEPRAZOLE 20 milligrams (mg) once daily was shown to be superior to omeprazole 10 mg once daily or placebo in patients with gastroesophageal reflux disease without erosive esophagitis as determined by endoscopy, according to a randomized, double-blind trial (n=359). Omeprazole 20-mg group had the highest proportion of patients with no heartburn during the entire last, ie, fourth, week of the study (48% vs 27% (10-mg group), and 5% (control group); p less than or equal 0.002) (Richter et al, 2000). c) High daily doses of omeprazole (40 milligrams) have been successfully used in intellectually disabled individuals with grade I to IV reflux esophagitis. These patients were initially treated for a total of 3 months; maintenance doses were used for an additional 3 months. Higher doses were used because this patient population generally has a poor response to lower doses. In addition, they often present with more severe esophagitis than the general population with GERD. Once asymptomatic after 3 months of treatment, 20 mg once daily is effective in preventing relapse (Bohmer et al, 1997a). d) Omeprazole is indicated for the short-term (4 to 8 weeks) treatment of severe erosive esophagitis (grade 2 or higher) which has been diagnosed endoscopically (Prod Info Prilosec(R), 2001b). For maintenance therapy, omeprazole is indicated for severe erosive or complicated ESOPHAGITIS grade 3 or above, or for grade 2 or greater in patients who have had at least 1 relapse (Skoutakis et al, 1995f; Dent et al, 1986a; Hetzel et al, 1986; Dammann et al, 1986b). 11) Gastroesophageal reflux disease; Diagnosis a) SUMMARY 1) A 7-day omeprazole test has been effectively used as a diagnostic strategy in patients with noncardiac chest pain. The dosage used consists of omeprazole 40 milligrams (mg) in the morning and 20 mg in the evening (Ofman et al, 1999; Fass et al, 1999). b) The omeprazole test of 40 milligrams (mg) in the morning and 20 mg in the evening for 7 days as a diagnostic strategy in patients with noncardiac chest pain resulted in reduced costs, improved diagnostic accuracy, and a larger number of symptom-free patients at 1 year compared with conventional invasive diagnostic tactics. The decision analysis study to evaluate clinical and economic outcomes utilizing the omeprazole test followed sequentially by ambulatory pH monitoring, then manometry, and then endoscopy, resulted in an average cost savings of $454 per patient (Ofman et al, 1999). c) The omeprazole test of 40 milligrams (mg) in the morning and 20 mg in the evening for 7 days was a sensitive and cost- effective diagnostic tool for detecting gastroesophageal reflux disease (GERD) in a randomized, double-blind, placebo- controlled, crossover trial of 42 patients. The cost-effective analysis demonstrated the omeprazole test resulted in an average savings of $348 per patient undergoing a diagnostic evaluation for heartburn (Fass et al, 1999). 12) Helicobacter pylori gastrointestinal tract infection a) A triple drug regimen consisting of CIPROFLOXACIN, OMEPRAZOLE, and BISMUTH was effective in eradicating Helicobacter pylori in 76% of infected patients. The dosage used in this trial consisted of the following: oral ciprofloxacin 500 milligrams twice daily for 14 days, oral omeprazole 20 milligrams twice daily for 30 days, and 2 bismuth subsalicylate (Pepto-Bismol(R)) tablets 4 times daily for 30 days (Dresner et al, 1996). - Clarithromycin 250 milligrams twice daily PLUS - Omeprazole 20 milligrams once daily PLUS - Tinidazole 500 milligrams twice daily, each for 7 days (Trevisani et al, 1998) b) GENERAL DOSING INFORMATION 1) Eradication rate 83.7% in patients with active or non-active duodenal or gastric ulcers (Trevisani et al, 1998a). c) To reduce the incidence of duodenal ulcer recurrence, the manufacturer recommends combining omeprazole with clarithromycin. The recommended dosage is omeprazole 40 milligrams once daily plus clarithromycin 500 milligrams 3 times daily for days 1 through 14. For days 15 through 28, only omeprazole is recommended and the dosage should be reduced to 20 milligrams once daily (Prod Info Prilosec(R), 2001a). d) HELICOBACTER PYLORI - DUAL THERAPY 1) SUMMARY a) Omeprazole, with clarithromycin, is approved for treating patients with H pylori infection and duodenal ulcer disease. Therapy will continue from 14 to 28 days depending on if an ulcer is present at initiation of therapy. In patients who fail therapy, dual therapy with clarithromycin is more likely to be associated with clarithromycin resistance than triple-drug therapy (Prod Info Prilosec(R), 2001a). 2) The following dual-drug regimen is approved for treating H pylori infection: omeprazole 40 milligrams(mg) once daily and clarithromycin 500 mg 3 times daily. Continue regimen for 14 days. In patients who present with an ulcer at the initiation of therapy, an additional 14 days of omeprazole 20 mg once daily is recommended for ulcer healing and symptom relief (Prod Info Prilosec(R), 2001a). It appears that omeprazole-containing triple-drug regimens are more effective than omeprazole-containing dual-drug regimens (Prod Info Prilosec(R), 2001a; Prod Info Prilosec(R), 1998). 3) Omeprazole 20 milligrams twice daily or 40 milligrams once daily in combination with clarithromycin 500 milligrams three times daily for 14 days is effective in patients with HELICOBACTER PYLORI infections. Eradication rates at these dosages range between 72% to 84% (Markham & McTavish, 1996). HIGHER cure rates are observed with omeprazole 40 milligrams once daily as compared to the 20 milligrams twice daily dosage (Soll, 1996). e) A dosage range study found that omeprazole 60 to 80 milligrams daily in divided doses in COMBINATION with amoxicillin 500 milligrams four times daily was more effective in eradicating H pylori than omeprazole 20 to 40 milligrams daily in combination with amoxicillin (Rokkas et al, 1995). f) Omeprazole 40 milligrams twice daily in combination with amoxicillin 1 gram twice daily has been used in the treatment of Helicobacter pylori. The eradication rate for this regimen ranges from 58% to 77% in patients with either duodenal or gastric ulcers or both. More effective regimens are available using omeprazole in combination with antibiotics and bismuth compounds (Thijs et al, 1996; Tursi et al, 1996). g) A 14-day course of oral omeprazole 20 milligrams twice daily in combination with intravenous amoxicillin 2 grams three times daily for 7 days cured 60% of patients with Helicobacter pylori. If amoxicillin treatment was less than 7 days, the cure rate was less than 10%. Amoxicillin was administered intravenously to insure compliance. Clinically, omeprazole in triple drug regimens (ie, combined with bismuth, imidazoles and tetracyclines or amoxicillin or clarithromycin) has been more successful in eradicating H pylori than dual therapy using omeprazole and amoxicillin (Adamek et al, 1996; Bertoni et al, 1995); (Trieber, 1996)(Tursi et al, 1996). h) The duodenal healing rate and Helicobacter pylori eradication rate for a 2-week course of omeprazole (20 milligrams) and amoxicillin (1 gram twice daily) has been reported to be 83% and 75.5%, respectively. In comparison to triple drug therapy with bismuth, metronidazole, and tetracycline, the dual therapy regimen was similar in efficacy but with less adverse drug reactions (Sung et al, 1996). i) In a meta-analysis of various drug regimens (ie, mono, dual, and triple drug regimens) for the treatment of Helicobacter pylori, omeprazole 20 milligrams once daily combined with clarithromycin 500 milligrams/day and metronidazole 800 milligrams/day was considered the optimal drug regimen (eradication rate greater than 90%) in terms of efficacy and cost-effectiveness. If side effects and compliance are an issue, the recommended drug regimen is a 2 week course of omeprazole 40 milligrams daily combined with either amoxicillin (minimum dose of 2 grams daily) or clarithromycin (1 gram daily). The eradication rate for this dual therapy regimen ranges from 60% to 95% (Treiber et al, 1996)(Axon & Moayyedi, 1996; Unge, 1996). j) HELICOBACTER PYLORI - TRIPLE THERAPY The following 7-day regimen has had excellent clinical results (Hackelsberger & Malfertheiner, 1996): - Omeprazole 20 milligrams (mg) twice daily - Clarithromycin 250 mg twice daily - Metronidazole 400 mg twice daily The manufacturer recommends the following 10-day regimen: - Omeprazole 20 mg twice daily - Clarithromycin 500 mg twice daily - Amoxicillin 1000 mg twice daily In patients with an ulcer present at the time of initiation of therapy, an additional 18 days of omeprazole 20 mg once daily is recommended (Prod Info Prilosec(R), 2001a). 1) Several clinical trials have evaluated numerous different combinations of anti-ulcer drugs with antibiotics for the treatment of Helicobacter pylori. A 7-day, twice daily regimen of omeprazole (20 milligrams (mg)), clarithromycin (250 mg), metronidazole (400 mg) has H pylori eradication rates of up to 100% (Hackelsberger & Malfertheiner, 1996). The manufacturer recommended 10-day, twice daily regimen of omeprazole (20 mg), clarithromycin (500 mg), and amoxicillin (1000 mg) results in H pylori eradication rates of 69% to 83% (intent-to-treat)(Prod Info Prilosec(R), 2001a). 2) DURATION OF THERAPY a) Triple therapy for eradication of Helicobacter pylori infection was shown to be significantly more effective when given for 14 days compared with 7-day treatment; these findings were based on a metaanalysis of 13 studies which used a 3-drug combination including a proton pump inhibitor, clarithromycin, and either amoxicillin or metronidazole. Though not significant, there was a trend favoring 14day over 10-day triple therapy and 10-day over 7-day treatment. Side effects were more frequent with longer therapy, though the difference was not significant (Calvet et al, 2000). 3) An effective regimen in treating Helicobacter pylori infections utilizes the combination of OMEPRAZOLE, CLARITHROMYCIN, and METRONIDAZOLE. A dose-ranging study showed that 4-day triple therapy (omeprazole 20 milligrams (mg), clarithromycin 250 mg, and metronidazole 400 mg twice a day) followed by 6-day omeprazole 20 mg twice a day only was as effective as 10 days of the 3-drug combination and resulted in cost savings (Hurenkamp et al, 2000). 4) The combination of omeprazole, amoxicillin, and metronidazole is effective in the eradication of H pylori. However, the dosage of metronidazole may influence the eradication rate in patients with metronidazole-resistant H pylori. In two multicenter, randomized, parallel-group studies, patients were randomized to receive 7-day treatment with either omeprazole 40 milligrams (mg) once daily, amoxicillin 500 mg three times daily and metronidazole 400 mg three times daily (OAMtid; n=242); omeprazole 20 mg twice daily, amoxicillin 1000 mg twice daily and metronidazole 800 mg twice daily (OAM800; n=247); or omeprazole 20 mg twice daily, amoxicillin 1000 mg twice daily and metronidazole 400 mg twice daily (OAM400; n=127). The overall Helicobacter pylori (H pylori) cure rates were 76% with OAMtid, 80% with OAM800, and 76% with OAM400. In patients with metronidazole-sensitive H pylori strains, the overall eradication rate was 85% compared with 60% in patients with metronidazoleresistant strains (p less than 0.001). Although not statistically significant, the higher daily dosage of metronidazole (OAM800) resulted in a greater eradication rate in patients infected with metronidazole-resistant H pylori strains compared with regimens containing lower daily metronidazole doses (Bayerdorffer et al, 1999ab). 5) The following regimen has been effective: omeprazole 20 milligrams twice daily; clarithromycin 250 milligrams twice daily; metronidazole 400 milligrams twice daily. This triple drug therapy is administered for 7 days, is well tolerated, and has H pylori eradication rates of up to 100%. Resistance to either antibiotic will reduce the H pylori eradication rate (Hackelsberger & Malfertheiner, 1996). 6) The combination of omeprazole, amoxicillin, and metronidazole achieved an approximate 80% cure rate of Helicobacter pylori (H pylori) infection in one clinical trial (n=255). Most importantly, this trial demonstrated that the total daily dose and frequency of administration did not influence the outcome. Patients with H pylori- associated active duodenal ulcer were randomized to receive either a combination of omeprazole 20 milligrams (mg) twice daily, amoxicillin 1000 mg twice daily and metronidazole 800 mg twice daily (OAMbid); or a combination of omeprazole 40 mg once daily in the morning, amoxicillin 500 mg three times daily and metronidazole 400 mg three times daily (OAMtid). Both regimens were administered for 7 days, followed by all patients receiving omeprazole 20 mg once daily in the morning for 3 weeks. Ulcer healing in the intention-to-treat analysis was documented in 95% and 97% of patients receiving OAMbid and OAMtid treatments, respectively (Bayerdorffer et al, 1999b). In a clinical trial involving patients with metronidazole-resistant (MR) or metronidazole-susceptible (MS) Helicobacter pylori (H pylori) strains, the following one-week treatment regimens were effective: - -Option 1: Omeprazole 20 milligrams (mg) twice daily; Metronidazole 400 mg twice daily; Clarithromycin 250 mg twice daily (OMC). - -Option 2: Omeprazole 20 mg twice daily; Amoxicillin 1000 mg twice daily; Clarithromycin 500 mg twice daily (OAC). In the per-protocol (PP) analysis in the metronidazole group, the eradication rate for H pylori was 91% (52 of 57 patients) in the OAC treatment group and 84% (46 of 55 patients) in the OMC treatment group. If separating out MR and MS groups, both treatment groups were equivalent in the MS group according to the PP analysis. If using the intent-to-treat analysis, both treatment groups were equivalent in the MR group (Houben et al, 1999c). 7) Omeprazole 20 millgrams once daily for 4 weeks plus amoxicillin 1 gram 3 times daily and metronidazole 250 milligrams 4 times daily during the 2nd and 3rd weeks is effective in eradicating Helicobacter pylori and preventing duodenal ulcer recurrence (Bianchi Porro et al, 1996b). In a region with high metronidazole resistance, the following 2-week regimen was effective in eradicating 94% of H pylori-infected patients: - Omeprazole 20 milligrams (mg) twice daily - Amoxicillin 500 mg three times daily - Clarithromycin 250 mg three times daily (Adeyemi et al, 1999c) This study was conducted in patients (n=50) with endoscopic evidence or a past medical history of duodenal ulcer disease (Adeyemi et al, 1999c). k) The addition of omeprazole or ranitidine to the combination of amoxicillin and colloidal bismuth subcitrate (CBS) have equal efficacy in terms of ulcer healing, eradicating Helicobacter pylori, and preventing ulcer recurrence. Patients were given amoxicillin 1000 milligrams 2 times daily for 2 weeks and colloidal bismuth subcitrate 120 mg orally 4 times daily for 40 days. In addition to amoxicillin and bismuth therapy, patients were also given either ranitidine or omeprazole. The dosage regimen for these 2 drugs are as follows: Ranitidine 300 milligrams 2 times daily for 4 weeks followed by 150 mg 2 times daily for 8 weeks; Omeprazole 40 mg once daily for 4 weeks followed by 20 mg once daily for 8 weeks (Cataldo et al, 1996a). The combination of omeprazole, clarithromycin and furazolidone was effective in the eradication of Helicobacter pylori (H pylori) in duodenal-ulcer patients living in a region of high metronidazole resistance. Patients treated with the following: Omeprazole 20 milligrams (mg) every morning or omeprazole 20 mg twice daily Clarithromycin 500 mg twice daily Furazolidone 200 mg twice daily Clarithromycin and furazolidone were only given for the the first week of therapy. Omeprazole was continued for a total of 4 weeks. Of the 37 patients completing treatment, H pylori eradication was achieved in 97% of patients by the per-protocol analysis and in 90% of patients by the intention-to-treat analysis. No statistically significant difference was observed in the eradication rate between patients receiving omeprazole 20 mg and 40 mg daily doses (Dani et al, 1999b). l) Clarithromycin 500 milligrams (mg) every 8 hours AND Omeprazole 40 mg once in the morning for 14 days FOLLOWED BY Omeprazole 20 mg once daily for an additional 14 days for ulcer healing and symptom relief (Prod Info Biaxin(R), 2003) m) A short course (7 days) of omeprazole 20 milligrams once daily, tinidazole 500 mg twice daily, and clarithromycin 250 mg twice daily was effective in eradicating Helicobacter pylori in 72% of infected patients (Tursi et al, 1996). n) The duodenal healing rate and Helicobacter pylori eradication rate for a 1-week course of bismuth 120 milligrams, tetracycline 500 milligrams, and metronidazole 400 milligrams 4 times daily has been reported to be 89% and 83.6%, respectively. In comparison to a 2week course of omeprazole and amoxicillin, the triple-therapy regimen was similar in efficacy but had more adverse drug reactions (Sung et al, 1996). - Clarithromycin 500 milligrams, AND - Omeprazole 20 milligrams, AND - Amoxicillin 1000 milligrams all given twice daily for 10 days, FOLLOWED BY - Omeprazole 20 milligrams once daily for additional 18 days for ulcer healing and symptomatic relief if ulcer present at start of therapy (Prod Info Biaxin(R), 2003) LOW-DOSE CLARITHROMYCIN REGIMEN: - Clarithromycin 250 milligrams AND - Omeprazole 20 milligrams AND - Amoxicillin 1000 milligrams, all given twice daily for 7 days, FOLLOWED BY - Omeprazole 20 milligrams once daily for an additional 14 days (Choi et al, 2002). The low-dose CLARITHROMYCIN regimen produced comparable H. pylori eradication rates to the standard regimen of clarithromycin 500 milligrams, amoxicillin 1000 mg, and omeprazole 20 mg, all twice daily (Choi et al, 2002). o) A 4-day triple regimen consisting of lansoprazole (LAN), azithromycin (AZITH) and tinidazole (TIN) was as effective as a 1week regimen of omeprazole (OMEP), clarithromycin (CLAR), and TIN in curing H pylori infections in patients with active or non- active duodenal or gastric ulcers. The eradication rates for these 2 regimens were 78.7% and 83.7%, respectively. Doses used in this study were as follows: First regimen, LAN 30 mg twice daily on days 1 through 4, AZITH 500 mg once daily on days 2 through 4, and TIN 2000 mg for 1 dose on day 3; Second regimen, OMEP 20 mg once daily, CLAR 250 mg twice daily and TIN 500 mg twice daily on days 1 through 7 (Trevisani et al, 1998). p) A 7-day regimen of omeprazole 20 milligrams (mg) ONCE or TWICE daily with clarithromycin 250 mg twice daily and metronidazole 500 mg twice daily is effective for the treatment of H pylori infection. In the all-patients-treated analysis, eradication was 85% (39 of 46 in the omeprazole once daily group and 41 of 48 in the omeprazole twice daily group). Eradication was 80% in the intent-to-treat analysis, occurring in 39 of 49 patients in the omeprazole once daily group and in 41 of 51 patients in the omeprazole twice daily group (Chiba & Marshall, 2000). q) A 2-week regimen of rebamipide 100 milligrams (mg) 3 times daily in combination with amoxicillin (500 mg 3 times daily) and omeprazole (20 mg twice daily) is effective in eradicating H pylori in patients with peptic ulcer disease. All patients subsequently received an H2-blocker for 3 weeks (Nebiki et al, 1998) . See Drug Consult reference: "HELICOBACTER PYLORI INFECTIONS - DRUG OF CHOICE" 13) Stress ulcer; Prophylaxis a) The recommended loading dose is omeprazole oral suspension 40 milligrams (mg) initially, followed by 40 mg after 6 to 8 hours on the first day, then 40 mg once a day for up to 14 days (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006). 14) IMPORTANT NOTE a) For patients who have difficulty in swallowing, omeprazole delayedrelease capsules can be opened and the intact pellets can be mixed with one tablespoon of applesauce. All the pellets inside the capsule should be mixed with the applesauce and immediately swallowed with a glass of cool water. The applesauce (not hot) and pellets should not be chewed or crushed (Prod Info PRILOSEC(R) delayed release capules, 2005). Omeprazole intact granules can be mixed with a small amount of acidic fruit juice (eg, apple, cranberry, grape, grapefruit, orange, pineapple, prune, tomato, or V-8 juices) immediately prior to oral administration. Patients should be instructed to not chew the granules (Prod Info Prilosec(R), 1998). The granules should not be mixed with milk prior to administration. b) c) According to 1 study, omeprazole 20 milligrams twice daily is more effective (p less = 0.05) than 40 milligrams once daily (morning or evening) in maintaining gastric pH above 4; however, the effect of the different dosage regimens on distal esophageal acid exposure were not statistically different. The clinical relevance of these differences has not been determined (Kuo & Castell, 1996). d) In patients who FAIL combination therapy (ie, omeprazole plus clarithromycin) for the treatment of Helicobacter-associated duodenal ulcer, susceptibility testing is recommended. If H pylori resistance to clarithromycin is demonstrated or if susceptibility testing is not possible, alternative antimicrobial therapy is recommended (Prod Info Prilosec(R), 2001b). 15) COMPARATIVE DOSAGE TABLE The following table provides the recommended usual adult dosage ranges for the proton pump inhibitors (Prod Info Nexium(R), 2005; Prod Info PREVACID(R) oral delayed-release capsule, delayedrelease suspension, delayed-release disintegrating tablet, 2004; Prod Info PROTONIX(R) oral tablet, delayed-release, 2004; Prod Info Prilosec(R), 2003a; Prod Info Aciphex(R), 2003): GENERIC NAME BRAND NAME DOSAGE RANGE (mg) Esomeprazole Nexium 20 to 40 mg PO once daily Lansoprazole Prevacid 15 to 30 mg PO once daily Omeprazole Prilosec 20 to 40 mg PO once daily Pantoprazole Protonix 40 mg PO once daily Rabeprazole Achiphex 20 mg PO once daily Key: PO = orally E) Helicobacter-associated gastritis - Helicobacter-associated pyloric ulcer See Drug Consult reference: "HELICOBACTER PYLORI-INDUCED GASTRITIS/PEPTIC ULCERATION" F) Peptic ulcer disease See Drug Consult reference: "DRUG THERAPY OF PEPTIC ULCER DISEASE" G) MAXIMUM DOSE 1) Omeprazole in oral daily doses of up to 360 milligrams has been effective in producing improvement and marked inhibition of gastric acid secretion for patients with Zollinger-Ellison syndrome (Adams et al, 1988a). H) PRESCRIBING LIMITATIONS 1) The safety and efficacy of omeprazole has not been established beyond 8 weeks in patients with peptic ulcer disease. In the rare case in which a patient does not respond to therapy after 8 weeks, an additional 4 weeks may be useful. Also, if there is a recurrence of severe or symptomatic gastroesophageal reflux, an additional 4 to 8 weeks of therapy may be considered. However, omeprazole should not be used for maintenance therapy with the exception of erosive esophagitis. Maintenance treatment of erosive esophagitis has been evaluated up to 12 months (Prod Info Prilosec(R), 2001b). I) PROPHYLAXIS 1) Omeprazole 20 milligrams once daily was effective for the PROPHYLAXIS against peptic ulcers and dyspeptic symptoms in arthritic patients on non-steroidal anti-inflammatory drugs (NSAIDS). In comparison to placebo, omeprazole was more effective in reducing the incidence of ulcers (4.7% versus 16.7%, respectively) and reducing the incidence of dyspepsia (15.3% versus 35.6%, respectively) (Ekstrom et al, 1996). 1.3.2 Dosage in Renal Failure A) No dosage adjustment is required in patients with renal impairment (Prod Info Prilosec(R), 2001b). B) In patients with chronic renal failure who had a creatinine clearance between 10 to 62 milliliters/minute/1.73 meters squared, the disposition of omeprazole was not significantly different from that encountered in patients with normal renal function (Naesdal et al, 1986; Prod Info Prilosec(R), 2001b). Because omeprazole metabolites (which have little if any antisecretory effect) are primarily eliminated via the kidney, their elimination decreased in proportion to the individual's creatinine clearance (Prod Info Prilosec(R), 2001b). C) Doses of 30 milligrams/day have been examined in six patients with chronic renal failure and on regular hemodialysis. Omeprazole was administered on 3 occasions, each separated by 7 to 8 days. The first study day (non-dialysis day) a placebo capsule was given. On study days 2 (non-dialysis day) and 3 (dialysis day) 30 milligrams omeprazole was administered orally. There was no significant difference between nondialysis and dialysis measurements of gastric acid output, peak plasma concentration, time to reach peak plasma concentration and area under the curve (AUC) (Howden et al, 1985a). The drug was well tolerated, with no adverse effects noted. Omeprazole may be useful for the treatment of peptic ulcers in patients with chronic renal failure, however further study is needed. D) The primary route of elimination for omeprazole is hepatic; therefore, the disposition of omeprazole is not affected by varying degrees of renal dysfunction. The elimination of omeprazole metabolites IS affected by impaired renal function, but is compensated by increased biliary secretion (Andersson, 1996). 1.3.3 Dosage in Hepatic Insufficiency A) Dosage adjustment is suggested in patients with hepatic dysfunction and Asian subjects, especially those requiring long-term maintenance therapy (Prod Info Prilosec(R), 2001b). 1.3.4 Dosage in Geriatric Patients A) Although no dosage adjustments are required in elderly patients, the elimination rate is reduced and the bioavailability of omeprazole is increased. Patients should be monitored accordingly (Prod Info Prilosec(R), 2001b; Andersson, 1996). 1.4 Pediatric Dosage 1.4.1 Normal Dosage A) Oral route 1) Stress ulcer; Prophylaxis a) Omeprazole 0.5 milligram/kilogram suspension every 12 hours given through a nasogastric tube was successful for maintaining gastric pH above 4 to 5 and for preventing stress-related erosion of the gastrointestinal tract in pediatric patients (mean age 23.8 months) undergoing liver or intestinal transplantation (or both). About 20% to 25% of patients might need a shortened dosage interval of every 6 to 8 hours. The suspension was prepared by adding enteric-coated granules from omeprazole capsules to sodium bicarbonate 8.4% solution for injection to a final concentration of 2 milligrams/milliliter (Kaufman et al, 2002). B) Duodenal ulcer disease, Triple therapy; Adjunct - Helicobacter pylori gastrointestinal tract infection, Triple therapy; Adjunct 1) Triple therapy (ie, omeprazole, amoxicillin, and clarithromycin) was more effective than dual therapy (omeprazole and amoxicillin) in the eradication of H pylori infection in pediatric patients (n=136, ages 3 to 18 years). The omeprazole dose of 1 mg/kg/day was as effective as 2 mg/kg/day. Patients were randomized to receive an omeprazole dosage of either 1 or 2 milligrams/kilogram (mg/kg) per day (maximum 80 mg/day). Amoxicillin and clarithromycin were administered at dosages of 50 mg/kg/day (maximum 2 grams/day) and 20 mg/kg/day (maximum 1 gram/day), respectively. All drugs were administered in two divided doses daily for two weeks (Behrens et al, 1999b). C) Esophagitis 1) The safe and effective use of oral omeprazole at 0.5 milligram/kilogram/day was reported in 4 patients (age range 2 to 4.5 months) with peptic esophagitis (Alliet et al, 1994). 2) High daily doses of omeprazole (40 milligrams) have been successfully used in intellectually disabled individuals with grade I to IV reflux esophagitis. These patients were initially treated for a total of 3 months to heal ulcers. Patients enrolled in this study ranged from 4- to 75-years-old. The study did not report how many patients were in the pediatric group. Higher doses were used because this patient population generally has a poor response to lower doses. In addition, they often present with more severe esophagitis than the general population with GERD. Once asymptomatic after 3 months of treatment, 20 mg once daily is effective in preventing relapse (Bohmer et al, 1997a). 3) In a case report, a 4-month-old boy was successfully treated with omeprazole 0.5 milligram/kilograms once daily for 6 weeks for refractory esophagitis. The patient did not respond to a regimen of cisapride, cimetidine, and alginate antacid and was subsequently placed on omeprazole therapy. Within 48 hours of starting therapy, symptoms resolved and endoscopy at 5 weeks revealed complete healing of lesions (Alliet et al, 1993). Similar omeprazole dosages and results have been reported (Alliet et al, 1994). D) Gastroesophageal reflux disease, Symptomatic 1) In a consensus statement, the North American Society for Pediatric Gastroenterology and Nutrition recommends a omeprazole dose of 1 milligram/kilogram (mg/kg), maximum 20 mg, once daily or divided into two doses for the treatment of pediatric gastroesophageal reflux disease (Rudolph et al, 2001). 2) The effective omeprazole dosage for children (n=15, mean age, 8.1 years) with refractory gastroesophageal reflux disease (GERD) was in the range of 0.7 to 3.3 milligrams/kilogram (mean, 1.9 milligrams/kilogram) in one clinical trial. Starting omeprazole doses for patients older than 3 years of age was 20 milligrams once in the morning and for patients under the age of 3 was 10 milligrams once in the morning. In patients who could not swallow the capsules whole, omeprazole was administered as an oral solution or through a jejunostomy tube. Doses were titrated based on 24-hour intraesophageal pH studies. At the end of the second follow-up visit (ie, at 4 to 6 months), all patients were free of GERD sign and symptoms. Omeprazole was well tolerated with no major side effects noted during the trial (Gunasekaran & Hassall, 1993a). 3) According to a review of omeprazole use in children with gastroesophageal reflux disease with or without esophagitis, the recommended initial omeprazole dose is 1 milligram/kilogram/day Ranges of dosing and duration in published studies are 5 to 80 milligrams/day (0.2 to 3.5 milligrams/kilogram/day) for 2 weeks to 3 years. The contents of the capsule may be mixed in applesauce, fruit juice or yogurt if children cannot swallow the intact capsule (Zimmermann et al, 2001a). 4) High daily doses of omeprazole (40 milligrams) have been successfully used in intellectually disabled individuals with grade I to IV reflux esophagitis. These patients were initially treated for a total of 3 months to heal ulcers. Patients enrolled in this study ranged from 4 to 75 years old. The study did not report how many patients were in the pediatric group. Higher doses were used because this patient population generally has a poor response to lower doses. In addition, they often present with more severe esophagitis than the general population with GERD. Once asymptomatic after 3 months of treatment, 20 mg once daily is effective in preventing relapse (Bohmer et al, 1997a). 5) A case of documented ulcerative esophagitis in a 7-year-old boy with significant gastroesophageal reflux unresponsive to twelve weeks of ranitidine (75 milligrams twice a day) combined with domperidone (10 milligrams three times a day) and sucralfate (500 milligrams twice a day) is reported. Omeprazole 10 milligrams once a day was initiated with symptomatic relief reported within three days and demonstrated progressive weight gain. Abnormal endoscopic findings had completely resolved after eight weeks of omeprazole therapy. The child remained asymptomatic at a one-year follow-up (Dalzell et al, 1992). 6) In one study, an 8-week course of omeprazole 40 milligrams/day/1.73 square meters was effective in treating gastroesophageal reflux disease in children ages 6 months to 13 years. E) IMPORTANT NOTE 1) The safety and efficacy of omeprazole therapy in children has not been established; therefore, the manufacturer does not provide omeprazole dosing guidelines for children (Prod Info Prilosec(R), 2001b). 2.0 Pharmacokinetics 2.1 Onset and Duration A) Onset 1) Initial Response a) ANTACID EFFECT, oral: 113 minutes (Hedenstrom et al, 1997). 1) The average time to reach an intragastric pH of 4 for omeprazole 20 mg was 113 minutes. In this single-dose study, 40% of the subjects never reached pH 4 (Hedenstrom et al, 1997). 2) In 178 critically ill patients treated with omeprazole/sodium bicarbonate 40 mg/1680 mg, the average time to reach an intragastric pH above 4 was 1 to 2.5 hours after the first dose (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006). b) PEPTIC ULCER DISEASE, ORAL: 2 hours (Lind et al, 1983). 1) Omeprazole inhibits gastric acid secretion in a dose-dependent manner. Two hours after administration of single-dose oral omeprazole 20 mg and 40 mg, maximal acid secretion was inhibited by 51% and 86%, respectively. After 24 hours, inhibition was 26% and 48%, respectively (Lind et al, 1983). 2) Intravenous omeprazole 80 mg increased intragastric pH to greater than 4 within one hour of administration (Walt et al, 1985a). 2) Peak Response a) ANTACID EFFECT: oral suspension, 1 to 2.5 hours; oral capsule, within 2 hours (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005). 1) The maximum antisecretory effect of omeprazole occurs within 2 hours of oral administration (Prod Info PRILOSEC(R) delayed release capules, 2005). 2) In 178 critically ill patients treated with omeprazole/sodium bicarbonate 40 mg/1680 mg, the average time to reach an intragastric pH above 4 was 1 to 2.5 hours after the first dose (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006). 3) In a study of the antisecretory effect of repeated oral once daily dosing of omeprazole 40 mg/sodium bicarbonate 1680 mg compared with omeprazole 20 mg/sodium bicarbonate 1680 mg, the decrease in gastric acidity was 84% versus 82%. Time that gastric pH was greater than 4 was 18.6 hours versus 12.2 hours, and median pH was 5.2 versus 4.2 (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006). b) PEPTIC ULCER DISEASE, ORAL: 5 days (Cederberg et al, 1993). 1) Peak inhibition of basal and stimulated gastric acid secretion is reached in 5 days. After 1 day of omeprazole PO 30 mg/day, gastric acid secretion is suppressed by 30%. Fifty to 60% of gastric secretion is inhibited on days 5 and 10 (Muller et al, 1982). Similar results have been reported (Cederberg et al, 1993). 2) Omeprazole 20 mg/day has been shown to heal 79% of DUODENAL ULCERS after 2 weeks and 96.5% after 4 weeks (Huttemann et al, 1986a). The healing rate for GASTRIC ULCERS appears to be slower, with 43%, 81% and 95% healed after 2, 4, and 8 weeks of omeprazole 20 mg/day, respectively. In patients with reflux esophagitis, complete ulcer healing may require 6 to 8 weeks (Dent et al, 1986; Dammann et al, 1986a). Rate of ulcer healing may be slower in patients who smoke (Prichard et al, 1985b; Classen et al, 1985a). B) Duration 1) Single Dose a) INTRAGASTRIC ACIDITY, ORAL: unquantified (Thomson et al, 1997a). 1) The mean percentage of time that a pH of 3 or greater is maintained over 24 hours ranges from 50.7% (capsule) to 57.4% (tablet) for a single oral 20 milligram-dose of omeprazole. There is no statistical difference between the enteric-coated tablet and the capsule in reducing intragastric acidity (Thomson et al, 1997a). b) PEPTIC ULCER DISEASE, ORAL: 1 to 5 days (Lind et al, 1983). 1) Omeprazole inhibits gastric acid secretion in a dose-dependent manner. Two hours after administration of single-dose oral omeprazole 20 mg and 40 mg, maximal acid secretion was inhibited by 51% and 86%, respectively. After 24 hours, inhibition was 26% and 48%, respectively. Inhibition of gastric acid secretion further declined over 2 to 5 days (Lind et al, 1983). 2) The prolonged duration of gastric acid inhibition seen after single doses of omeprazole is not due to sustained plasma levels (Cederberg et al, 1985; Lind et al, 1983). The exact mechanism is unknown; however, the AUC for omeprazole has been noted to correlate strongly with its inhibitory effect (Lind et al, 1983; Muller et al, 1982). 3) The duration of gastric acid inhibition is shorter with intravenous omeprazole than with oral. Two 80-mg doses of intravenous omeprazole (every 12 hours) will raise intragastric pH to greater than 4, however will not consistently maintain it over the subsequent 22 hours. Increasing the frequency to every 8 hours will increase gastric pH for most of 24 hours (Walt et al, 1985a). 4) The median percentage of time the gastric pH was greater than 4.5 was 93% on day 1 and 96% on day 3 with continuous infusion omeprazole. Mean doses on day 1 and 3 for omeprazole were 235 mg and 134 mg, respectively (Walt et al, 1985a). 2) Multiple Dose a) PEPTIC ULCER DISEASE: unquantified (Olbe et al, 1986; Muller et al, 1982). 1) With repeated dosing of omeprazole, the gastric acid inhibitory effect accumulates over the first few days and stabilizes after 3 to 5 days (Olbe et al, 1986; Muller et al, 1982). 2.2 Drug Concentration Levels A) Therapeutic Drug Concentration 1) PEPTIC ULCER DISEASE, not well established (Clissold & CampoliRichards, 1986a; Regardh et al, 1985). a) The normal therapeutic range for omeprazole is 0.19 to 19.4 micromol/L (Clissold & Campoli-Richards, 1986a; Regardh et al, 1985). Despite the dose-dependent gastric acid inhibition seen with omeprazole, plasma levels of omeprazole do not correlate with its antisecretory effects (Clissold & Campoli-Richards, 1986a; Cederberg et al, 1985; Lind et al, 1983). b) The distribution of the drug to the parietal cells of the stomach is responsible for the major impact on gastric acid inhibition. There is no method, currently, to conveniently estimate drug concentration at this site (Clissold & Campoli-Richards, 1986a). B) Peak Concentration 1) adult: enteric-coated granules, single-dose, 668 ng/mL; repeated dosing, 1458 ng/mL (Prod Info PRILOSEC(R) delayed release capules, 2005) 2) pediatric: age 2 to 5 years, weight less than 20 kg, 10 mg single-dose enteric-coated granules, 288 ng/mL; 10 mg repeated-dosing enteric-coated granules, 539 ng/mL (Prod Info PRILOSEC(R) delayed release capules, 2005) 3) pediatric: age 6 to 16 years, weight greater than 20 kg, 20 mg single-dose enteric-coated granules, 495 ng/mL; 20 mg repeated-dosing enteric-coated granules, 851 ng/mL (Prod Info PRILOSEC(R) delayed release capules, 2005) a) Following a single 20-milligram dose of either the enteric-coated tablet or the capsule, the mean peak concentration (Cmax) was 1.53 and 1.09 micromoles/liter, respectively. Despite the higher Cmax for the tablet, there is no difference between the two formulations in terms of suppressing intragastric acidity over 24 hours (Thomson et al, 1997a). b) Peak plasma levels are approximately proportional up to doses of 40 mg/day, but due to saturation of the first-pass effect, a greater than linear response in peak levels occurs with higher doses (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005). c) There was a mean 25% decrease in peak concentration (unknown clinical relevance) when enteric-coated granules are administered with applesauce (Prod Info PRILOSEC(R) delayed release capules, 2005). C) Time to Peak Concentration 1) ORAL: 0.5 to 3.5 hours (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005). 2) Delayed-release capsules: 30 minutes to 3.5 hours (Prod Info PRILOSEC(R) delayed release capules, 2005) 3) Immediate-release capsules/suspension: 10 to 90 minutes (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006) a) Absorption of oral omeprazole varies among formulations. The time to peak serum concentrations varies markedly; omeprazole solutions attain peak serum levels in less than 20 minutes, powder for oral suspension in 30 minutes, immediate-release capsules in 30 minutes, and delayed-release capsules (containing enteric-coated granules) in 0.5 to 3.5 hours (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005; Clissold & CampoliRichards, 1986a; Regardh, 1986). b) Following a single 20-milligram dose of either the enteric-coated tablet or the capsule, the mean time to peak concentration (Tmax) was 2.03 and 1.59, respectively (p=0.036). Despite the shorter Tmax for the tablet, there is no difference between the two formulations in terms of suppressing intragastric acidity over 24 hours (Thomson et al, 1997a). c) Following a single 30-mg oral dose of omeprazole (enteric-coated formulation) a mean peak plasma concentration of 558 micrograms/L (range 223 to 1160 micrograms/L) was attained within 1.5 hours. However, after repeated dosing with omeprazole 30 mg/day, absorption was variable with peak serum levels attained from 1 to 5 hours after omeprazole (Howden et al, 1984). d) Omeprazole suspension 40 mg had a slower time-to-peak and a lower maximum concentration when given by the nasogastric route compared with administration via a duodenal or jejunal tube (t-max, 108.3 min versus 12.1 min, respectively (p less than 0.001); c-max, 0.97 mcg/mL vs 1.833 mcg/mL, respectively (p=0.006)); however, the area under the plasmaconcentration curve (AUC) was similar (not statistically significantly different) for administration via nasogastric tube versus duodenal/jejunal tube (AUC, 415.1 vs 396.7 mcg x hr/mL; p=0.91). The study was performed in 9 critically ill surgical patients, who were residing in the surgical intensive care unit and had mechanical ventilation and NPO status; all were considered at-risk for stress ulcers. The suspension was prepared by dissolving the contents of two 20-mg capsules in 20 mL of 8.4% sodium bicarbonate. Adequate gastric pH control (pH above 4.0) was provided with nasogastric, duodenal, or jejunal administration (Phillips et al, 2001a). D) Area Under the Curve 1) adults: single-dose enteric coated granules, 1220 ng x h/mL; repeated dosing, 3352 ng x h/mL(Prod Info PRILOSEC(R) delayed release capules, 2005) 2) adults: single-dose oral suspension, 1665 ng x h/mL; second dose, 3356 ng x h/mL (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006) 3) pediatric: age 2 to 5 years, weight less than 20 kg,10 mg single-dose enteric-coated granules, 511 ng x hours/mL; 10 mg repeated-dosing entericcoated granules, 1179 ng x h/mL (Prod Info PRILOSEC(R) delayed release capules, 2005) 4) pediatric: age 6 to 16 years, weight greater than 20 kg, 20 mg single-dose enteric-coated granules, 1140 ng x h/mL; 20 mg repeated dosing entericcoated granules, 2276 ng x h/mL (Prod Info PRILOSEC(R) delayed release capules, 2005) a) Following a single 20-milligram dose of either the enteric-coated tablet or the capsule, the mean area under the time-concentration curve (AUC) was 2.15 micromoles x hour/liter (mmol x h/L) and 1.85 mmol x h/L, respectively. Despite the greater AUC value for the tablet, there is no difference between the two formulations in terms of suppressing intragastric acidity over 24 hours (Thomson et al, 1997a). b) In a single-dose omeprazole 20-milligram pharmacokinetic study, a fourfold increase in AUC was observed in Asian subjects compared to Caucasians (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005). c) The AUC is approximately proportional up to doses of 40 mg/day, but due to saturation of the first-pass effect, a greater than linear response in AUC occurs with higher doses (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005). d) The maximum plasma concentration (Cmax) and area under the curve (AUC) of omeprazole increases when administered concomitantly with clarithromycin. In one study involving healthy volunteers, the administration of omeprazole 40 milligrams daily and clarithromycin 500 milligrams every 8 hours resulted in the increase of Cmax and AUC (time 0 to 24 hours) of 30% and 89%, respectively (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005). e) The AUC for omeprazole has been noted to correlate strongly with its inhibitory effect (Lind et al, 1983; Muller et al, 1982). f) Omeprazole suspension 40 mg had a slower time-to-peak and a lower maximum concentration when given by the nasogastric route compared with administration via a duodenal or jejunal tube (t-max, 108.3 min versus 12.1 min, respectively (p less than 0.001); c-max, 0.97 mcg/mL vs 1.833 mcg/mL, respectively (p=0.006)); however, the area under the plasmaconcentration curve (AUC) was similar (not statistically significantly different) for administration via nasogastric tube versus duodenal/jejunal tube (AUC, 415.1 vs 396.7 mcg x hr/mL; p=0.91). The study was performed in 9 critically ill surgical patients, who were residing in the surgical intensive care unit and had mechanical ventilation and NPO status; all were considered at-risk for stress ulcers. The suspension was prepared by dissolving the contents of two 20-mg capsules in 20 mL of 8.4% sodium bicarbonate. Adequate gastric pH control (pH above 4.0) was provided with nasogastric, duodenal, or jejunal administration (Phillips et al, 2001a). 2.3 ADME 2.3.1 Absorption A) Bioavailability 1) ORAL: 30% to 40% (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005; Regardh, 1986). a) Following oral doses of 20 to 40 mg of both the immediate-release products and the extended-release products, the absolute bioavailability is 30% to 40% (compared with intravenous administration). The bioavailability of omeprazole increases with repeated administration 65% of steady state. The low degree of bioavailability is primarily due to presystemic metabolism (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005; Andersson, 1996a; Regardh, 1986). b) The absorption rate of omeprazole may increase with multiple doses resulting in improved antisecretory effect (Markham & McTavish, 1996d). c) Due to the enteric coating, the granules of omeprazole are absorbed only after leaving the stomach, and absorption is rapid (Prod Info PRILOSEC(R) delayed release capules, 2005). d) The bioavailability of omeprazole increased up to approximately 100% compared with an IV dose in patients with chronic hepatic disease (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005). e) Bioavailability of omeprazole is greater in elderly compared to younger patients. The bioavailability following a single oral dose of 40 mg as a buffered solution was 76% compared to 58% in younger subjects (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005). f) The mean bioavailability of omeprazole in patients with ZollingerEllison syndrome (68%) is not significantly different from the bioavailability in healthy elderly (79%) or young (54%) patients (Vinayek et al, 1991). g) The mean systemic availability of omeprazole 40 mg orally in patients with chronic renal insufficiency (creatinine clearance 10 to 62 mL/min/1.73 m(2)) was 70% (Naesdal et al, 1986a). B) Effects of Food 1) The rate, but not the extent, of absorption is affected by food (Thomson et al, 1997; Andersson et al, 1990g). a) Omeprazole should be taken before eating (Prod Info PRILOSEC(R) delayed release capules, 2005). Omeprazole powder for oral suspension and immediate-release capsules should be taken 1 hour before a meal (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006). b) When the powder for oral suspension or immediate-release capsules was administered 1 hour after a meal the Cmax and AUC were reduced by 63% and 24%, respectively (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006). c) Absorption of omeprazole is delayed by food. When enteric-coated granules are administered on an empty stomach, the time between administration and the morning meal is not important (Pilbrant & Cederberg, 1985). d) The time to peak concentration (Tmax) was prolonged when omeprazole was administered after breakfast as compared to fasting conditions (3.5 hours versus 2.21 hours; p = 0.6109). No significant difference was noted for Tmax between before breakfast administration and fasting conditions (Thomson et al, 1997). 2.3.2 Distribution A) Distribution Sites 1) Protein Binding a) 95% to 96% (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005); (Anderson, 1996)(Regardh et al, 1985). 1) The drug is primarily bound to serum albumin and alpha-1-acid glycoprotein (Regardh et al, 1985). 2) The mean plasma protein binding (95.2%) of omeprazole in patients with chronic renal insufficiency (creatinine clearance 10 to 62 mL/min/1.73 m(2)) was not significantly different from healthy volunteers (Naesdal et al, 1986a). 2) OTHER DISTRIBUTION SITES a) FETAL TISSUE, good (Mears & Kaplan, 1996b) 1) Omeprazole achieves fetal tissue concentrations similar to that achieved in the plasma (Mears & Kaplan, 1996b). b) TISSUES, excellent (Regardh et al, 1985) 1) Omeprazole distributes rapidly to extravascular sites. Thirtyminutes after intravenous administration in rats, the highest concentrations (12 to 23 nanomol/g tissue) were found in the liver, kidneys and duodenum. Comparatively high concentrations were also observed in the stomach and thyroid gland. Penetration into red blood cells is low; the ratio between concentration of drug in whole blood and plasma being 0.6. Omeprazole, and its metabolites, cross the blood-brain barrier only to a very limited extent (Regardh et al, 1985). 2) The distribution pattern following oral omeprazole is similar to intravenous administration, however the stomach and duodenum contained the highest concentration of drug during the first 6 hours after administration (Regardh et al, 1985). B) Distribution Kinetics 1) Volume of Distribution a) 0.34 to 0.37 L/kg (Regardh, 1986). 1) The Vd of omeprazole has been observed to be smaller in the elderly than in young healthy subjects. According to one study, a Vd of 0.24 L/kg was reported in the elderly as compared to 0.34 to 0.37 L/kg in young subjects (Regardh, 1986). 2) The Vd of omeprazole 40 mg orally in patients with chronic renal insufficiency (creatinine clearance 10 to 62 mL/min/1.73 m(2)) was within the range of that reported for healthy subjects (Naesdal et al, 1986a). 3) The mean Vd of omeprazole in patients with Zollinger-Ellison syndrome was not significantly different from that reported for elderly healthy subjects and young healthy volunteers (Vinayek et al, 1991). 2.3.3 Metabolism A) Metabolism Sites and Kinetics 1) LIVER, extensive (Regardh et al, 1985; Regardh et al, 1985). a) After administration of radiolabeled omeprazole (intravenous and oral), 60% of total radioactivity was collected in the urine during the first 6 hours. Over the next 4 days, 75 to 78% of the administered dose was recovered in urine and 18 to 19% in feces. Insignificant amounts of unchanged drug are eliminated via the kidneys or stools (Regardh, 1986). b) At therapeutic doses, omeprazole is not an enzymatic inducer of a subfamily of P450 cytochromes called P4501A2 (Rizzo et al, 1996). c) However, a major enzyme involved in the metabolism of omeprazole is the polymorphically expressed cytochrome P450 (CYP) isoform Smephenytoin hydroxylase also known as CYP2C19. Some patients who are deficient in this enzyme system will be slow metabolizers of omeprazole. Patients who are slow metabolizers can produce plasma concentrations 5 or more times higher than patients with the enzyme present (Andersson, 1996a) d) In elderly patients, the plasma clearance of omeprazole is decreased and the area under the plasma concentration-time curve in increased in comparison to younger healthy adults. Changes in these pharmacokinetic parameters are due to decreased metabolism secondary to decreased liver blood flow and liver volume (Andersson, 1996a). B) Metabolites 1) HYDROXYOMEPRAZOLE, inactive (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005; Regardh, 1986). 2) OMEPRAZOLE SULFONE, inactive (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005; Regardh, 1986). 3) OMEPRAZOLE SULFIDE, inactive (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005; Regardh, 1986). 2.3.4 Excretion A) Kidney 1) Renal Excretion (%) a) 77% (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005). 2) Following a single oral dose of a omeprazole solution, little if any unchanged drug was eliminated renally. Most of the dose (ie, 77%) is excreted in the urine in the form of 6 metabolites or more. The remaining amount of the dose was excreted in the feces (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005). 3) In patients with chronic renal impairment, creatinine clearance between 10 and 62 mL/minute/1.73 m(2), the elimination of omeprazole metabolites slowed in proportion to the decreased creatinine clearance (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005) B) Total Body Clearance 1) 500 to 600 mL/minute (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005). a) The total body clearance decreases to 70 mL/minute in patients with chronic hepatic disease (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005). b) The plasma clearance decreases to 250 mL/minute in geriatric patients (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005). C) Other 1) OTHER EXCRETION a) FECAL, significant (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005; Regardh et al, 1985). 1) Biliary excretion appears to play a significant role in the elimination of omeprazole metabolites (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005; Regardh et al, 1985). Biliary elimination of omeprazole following intravenous and oral administration, has ranged from 16% to 19% (Lind et al, 1987; Regardh et al, 1985). The fecal excretion of omeprazole appears to be due to biliary excretion (Lind et al, 1987). 2) Following a single oral dose of a omeprazole solution, approximately 77% of the dose was excreted in the urine in the form of 6 metabolites or more. The remaining amount of the dose was excreted fecally (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005). b) BILE, significant (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005; Regardh et al, 1985). 1) Biliary excretion appears to play a significant role in the elimination of omeprazole metabolites (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005; Regardh et al, 1985). Biliary elimination of omeprazole following intravenous and oral administration, has ranged from 16% to 19% (Lind et al, 1987; Regardh et al, 1985). The fecal excretion of omeprazole appears to be solely due to biliary excretion (Lind et al, 1987). 2.3.5 Elimination Half-life A) Parent Compound 1) ELIMINATION HALF-LIFE a) 0.5 to 1 hour (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005; Clissold & Campoli-Richards, 1986a). 1) The half-life increases up to almost 3 hours in patients with chronic hepatic disease (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005). 2) The mean plasma half-life of omeprazole in patients with chronic renal insufficiency (creatinine clearance of 10 to 62 mL/minute/1.73 m(2)) is 0.6 hours; which is not significantly different from healthy volunteers (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005; Naesdal et al, 1986a). 3) The plasma half-life in geriatric patients is 1 hour, averaging about twice that of young healthy patients (Prod Info ZEGERID(R) oral capsules, powder for oral suspension, 2006; Prod Info PRILOSEC(R) delayed release capules, 2005) 4) The mean plasma half-life of 80 mg of omeprazole administered orally in patients with Zollinger-Ellison syndrome was 2.4 +/- 0.5 hours (range 1.2 to 5.6 hours). This half-life is significantly longer than that of healthy volunteers, but not significantly different from elderly healthy subjects (Vinayek et al, 1991). 2.3.6 Extracorporeal Elimination A) Hemodialysis 1) Dialyzable: No (Howden et al, 1985aa). a) Hemodialysis has no effect on gastric acid output, peak plasma concentration, time to reach peak plasma concentration and area under the curve (AUC) (Howden et al, 1985aa). 3.0 Cautions 3.1 Contraindications A) Hypersensitivity to omeprazole or to any of its components (Prod Info Prilosec(R), 2001) 3.2 Precautions A) Bartter's syndrome (powder for oral suspension contains 1680 milligrams (20 milliequivalents of sodium bicarbonate)-use with caution (Prod Info Zegerid(TM), 2004) B) Hypocalcemia -contraindicated (powder for oral suspension contains 1680 mg (20 mEq) of sodium bicarbonate) (Prod Info Zegerid(TM), 2004) C) Hypokalemia (powder for oral suspension contains 1680 mg (20 mEq) of sodium bicarbonate)-use with caution (Prod Info Zegerid(TM), 2004) D) Long-term administration of bicarbonate with calcium or milk can cause milkalkali syndrome (Prod Info Zegerid(TM), 2004) E) Long-term omeprazole therapy; risk of atrophic gastritis (Prod Info Prilosec(R), 2001) F) Metabolic alkalosis-contraindicated (powder for oral suspension contains 1680 mg (20 mEq) of sodium bicarbonate) (Prod Info Zegerid(TM), 2004) G) Patients on a sodium-restricted diet (powder for oral suspension- 460 mg sodium per dose) (Prod Info Zegerid(TM), 2004) H) Respiratory alkalosis (powder for oral suspension contains 1680 mg (20 mEq) of sodium bicarbonate)-use with caution (Prod Info Zegerid(TM), 2004) I) Symptomatic response to omeprazole therapy does not preclude the presence of gastric malignancy (Prod Info Prilosec(R), 2001) 3.3 Adverse Reactions 3.3.1 Cardiovascular A) Cardiovascular finding 1) Less than 1% of patients have developed chest pain or angina, tachycardia, bradycardia, palpitations, or peripheral edema; the relationship to these effects and omeprazole has not been determined (Prod Info Prilosec(R), 2001a). 2) A single report of palpitations has occurred with omeprazole in a patient with duodenal ulcers. The palpitations resolved despite continued dosage and could not be clearly attributed to omeprazole (Prichard et al, 1985). B) Peripheral edema 1) Reversible peripheral edema occurred in 5 female patients (range 26 to 58 years of age) after use of omeprazole, lansoprazole, or pantoprazole for 7 to 15 days. Doses ranged from 20 to 40 milligrams/day orally. Other symptoms included weight gain and decreases in urine output. Swelling of legs and/or hands developed within 11 to 21 days of initiation of the protonpump-inhibitor (PPI). Symptoms re-occurred when the patients were rechallenged. In one patient, a decrease in creatinine clearance occurred during PPI treatment. Edema resolved within 2 to 3 days of PPI discontinuance. Kinetic assessments revealed that 3 of the patients were slow metabolizers of the PPI. A subsequent study of intravenous (IV) omeprazole found edema to occur in 3 of 6 female subjects, but no male subjects, when high doses were used (80 mg bolus followed by 24-hour continuous 8 mg/hr infusion), along with large volumes of fluids. Similar outcomes (though less severe) were found with IV pantoprazole. Edema resolved within 24 hours of stopping the infusion (Brunner et al, 2001). 3.3.2 Dermatologic A) Alopecia 1) A 48-year-old female experienced diffuse alopecia while taking omeprazole therapy. Diffuse loss of hair stopped and started with discontinuation and initiation of omeprazole, respectively. Resolution of hair loss occurred within 2 to 3 weeks of discontinuing therapy (Borum & Cannava, 1997). The manufacturer reports alopecia in less than 1% of patients receiving omeprazole (Prod Info Prilosec(R), 2001a). B) Dermatological finding 1) Photosensitivity, exfoliative disease, bullous eruption, and erythema multiforme have been reported as suspected adverse reactions associated with omeprazole therapy (Anon, 1991a). A severe case of EXFOLIATIVE DERMATIITIS developed in a patient who had been treated with therapeutic doses of omeprazole. Skin abnormalities were noted 3 months after omeprazole treatment. Involved areas included the back, trunk, and legs (Rebuck et al, 1998). 2) Cutaneous leukocytoclastic vasculitis occurred in a 71-year-old woman 4 weeks after initiation of OMEPRAZOLE 20 mg/day for epigastric pain. The patient presented with pruritus and an erythematous macular, papular rash (1 to 10 mm in diameter) on her hands, thighs, and lower abdomen. A skin biopsy specimen revealed small vessel vasculitis with neutrophilic infiltration, nuclear dust, and focal fibrinoid deposits within the vessel walls. There was also evidence of complete fibrinoid necrosis of some blood vessels and erythrocyte extravasation in the adjacent dermis. Omeprazole was withdrawn from therapy and treatment with budesonide and amiodarone continued. Within a few days, all skin lesions resolved completely. No re-challenge was performed. Omeprazole was the causative agent of this patient's CUTANEOUS VASCULITIS (Odeh et al, 2002). 3) A case of angioedema and urticaria with a positive rechallenge was reported in a 34-year-old women receiving omeprazole therapy. Over a 5day period, the patient developed a variety of symptoms following each omeprazole dose. Symptoms included shortness of breath, cough, and diffuse wheezing. Chest radiograph revealed a right pleural effusion and laboratory findings were significant for eosinophilia. On the 4th day of therapy, she developed swollen, erythematous lips and eyelids consistent with mild angioedema and shortness of breath. On the 5th day, rechallenge with omeprazole resulted in generalized total body urticaria and pruritus that responded to diphenhydramine (Bowlby et al, 1994). C) Erythema nodosum 1) Omeprazole treatment (20 mg as needed) was associated with erythema nodosum in a 35-year-old female and later confirmed with rechallenge. In this case report, the patient presented with multiple tender erythematous nodules over the lower extremities, fever, and difficulty in walking. Other medications included conjugated estrogen 0.625 mg. Upon rechallenge with omeprazole, tender erythematous nodules and fever returned within 12 hours of administration. Other causes of erythema nodosum were ruled out as defined by physical exam, laboratory tests, and x-rays (Ricco & Deering, 1996). D) Rash 1) Rash rarely occurs with omeprazole therapy (Prod Info Prilosec(R), 2001a). In a study of 104 assessable patients, only 1 patient reported an adverse drug reaction which was a RASH. This study was evaluating the efficacy of omeprazole for treating gastroesophageal reflux disease in intellectually disabled patients (Bohmer et al, 1997). 3.3.3 Endocrine/Metabolic A) Endocrine finding 1) A case of Gynecomastia in a 53-year-old man treated with omeprazole 20 mg per day was reported (Santucci et al, 1991). The patient received omeprazole 20 mg daily for eight weeks to treat a duodenal ulcer. Bilateral gynecomastia developed during therapy. Liver-function tests and hormone levels remained normal. Gynecomastia regressed four weeks after termination of omeprazole therapy. Upon rechallenge, after a four-month drug-free interval, there was a second onset of painful gynecomastia, and treatment was suspended. 2) A case of gynecomastia in a 68-year-old man treated with omeprazole 20 mg per day was reported (Convens et al, 1991). The patient received omeprazole 20 mg daily for three months to treat reflux esophagitis. Bilateral gynecomastia developed during therapy. Hormone levels, thyroid, liver, and renal function tests were normal. Omeprazole was discontinued and gynecomastia regressed in about three weeks. The patient refused a rechallenge. B) Metabolic finding 1) Hypoglycemia, fever, hyponatremia and weight gain have occurred in less than 1% of patients receiving omeprazole and the relationship to these effects and the drug are unclear (Prod Info Prilosec(R), 2001a). 2) A case report describes a 35-week gestation male that developed hyponatremia and hypokalemia following omeprazole therapy of 2 mg/kg/day. The patient was being treated for esophagitis who previously failed to respond to cimetidine, Domperidone and Gaviscon therapy. After 10 days of omeprazole therapy, serum sodium dropped to 129 mmol/L and serum potassium to 3.5 mmol/L despite aggressive replacement therapy. After discontinuing omeprazole, both serum potassium and sodium returned to normal levels within 24 hours (Melville et al, 1994). 3) Hypercalcemia, renal lesions, and acute interstitial nephritis were associated with omeprazole therapy in a 31-year-old female. After pregnancy (complicated by high blood pressure) and delivery of a healthy baby girl, the patient was stabilized on nifedipine (long-acting 30 mg/day) for hypertension, with omeprazole 20 mg/day her only other medication. Over 8 weeks, she developed asymptomatic hypercalcemia (serum calcium 3.22 mmol/L; normal, 2.2 to 2.7 mmol/L) and renal function deterioration. A percutaneous renal biopsy found intense eosinophilic infiltrates and tubuledestructive granulomata. Omeprazole had been discontinued 2 weeks prior to the biopsy. The patient was given prednisolone 40 mg/day, leading to normalization of serum calcium and improvement in kidney function; at 18 months follow-up, mild renal dysfunction persisted. The authors concluded that omeprazole induced the granulomatous lesions and associated hypercalcemia (Wall et al, 2000). 4) Long-term omeprazole therapy (ie, greater than 3 years) has been shown to decrease vitamin B12 (cyanocobalamin) absorption in a dose-dependent fashion (Mears & Kaplan, 1996a). C) Vitamin deficiency 1) Long-term omeprazole therapy can decrease serum vitamin B12; folate levels appear to be unaffected. According to a study of 111 patients with Zollinger-Ellison Syndrome, a significant reduction (p=0.04) of serum vitamin B12 was noted after a mean of 4.5 years (range, 0.2 to 12 years). Patients at greatest risk are those with sustained acid hyposecretion. These data suggest that patients with Zollinger-Ellison Syndrome receiving longterm omeprazole therapy should have serum vitamin B12 concentrations measured on a periodic basis (Termanini et al, 1998). 3.3.4 Gastrointestinal A) Abdominal pain 1) Abdominal pain (2.4% to 5.4%) has been associated with omeprazole therapy (Prod Info Prilosec(R), 2001a)(Cullen, 1998)(Yeomans, 1994a; Skoutakis et al, 1995d). B) Atrophic gastritis 1) Helicobacter pylori eradication and gastric-acid-reducing OMEPRAZOLE therapy appeared to mitigate gastric corpus atrophy and to stimulate restitution of glandular epithelium to normal levels in patients with endoscopic signs of reflux esophagitis (Savary-Miller grades 1 to 4). These findings were based on a randomized prospective trial in 71 patients with gastroesophageal reflux disease (48 H. pylori-positive; 23 H. pylorinegative). The H. pylori-positive patients were randomized to a 1-week course of placebo (n=21) or to eradication treatment (omeprazole 20 mg, amoxicillin 1 gram, clarithromycin 500 mg, all twice daily for 1 week; n=27). Subjects across all treatment groups received OMEPRAZOLE 40 mg/day for 12 months. Biopsies of gastric corpus mucosa were performed at baseline and after 3 and 12 months of omeprazole. In those who received eradication treatment, the volume percentage of glandular epithelium (VPGL) increased from 63% at baseline to 71.5% at 12 months (p less than 0.001), while the volume percentage of stroma (VPS) and of infiltrate decreased significantly (p less than 0.001 and p=0.04, respectively). The lower the VPGL at baseline, the greater was the percent increase at 12 months. In the H. pylori-persistent group (H. pylori-positive patients allocated to placebo), VPGL and VPS did not change significantly over 12 months, while volume percentage infiltrate (VPI) increased significantly (p=0.01). In the H. pylori-negative group, mean VPGL increased from 71.9% to 75.2% (p=0.03), while VPS and VPI were not significantly altered. In the eradication group, mean values of VPGL, VPS, and VPI returned after 12 months of therapy to levels similar to those in the H. pylori-negative group at baseline and at 12 months (representing close to normal restitution). One- year omeprazole therapy did not appear to dispose the H. pylori-negative patients to gastric atrophy (Van Grieken et al, 2001). C) Clostridium difficile diarrhea See Drug Consult reference: "PROTON PUMP INHIBITORS AND CLOSTRIDIUM DIFFICILE-ASSOCIATED DISEASE" D) Constipation 1) Constipation (1.1% to 1.5%) has been associated with omeprazole therapy (Prod Info Prilosec(R), 2001a)(Cullen, 1998)(Yeomans, 1994a; Skoutakis et al, 1995d). E) Diarrhea 1) Diarrhea (3% to 3.7%) has been associated with omeprazole therapy (Prod Info Prilosec(R), 2001a); (Cullen, 1998)(Yeomans, 1994a; Skoutakis et al, 1995d). F) Excessive upper gastrointestinal gas 1) Flatulence (2.7%) has been associated with omeprazole therapy (Prod Info Prilosec(R), 2001a)(Cullen, 1998)(Yeomans, 1994a; Skoutakis et al, 1995d). G) Fundic gland polyposis of stomach 1) Fundic gland polyps (FGP) were associated with long-term omeprazole therapy. In a case report of 6 patients, long-term omeprazole was being used to treat Barrett's esophagus. FGP was noted after 1 (2 patients), 2 (2 patients), 4 (1 patient), and 5 years (1 patient) of continuous omeprazole 20 milligrams once daily therapy. None of the patients were infected with Helicobacter pylori. Serum gastrin concentrations were elevated in 2 of the 6 patients. Malignant or adenomatous changes have not been associated with fundic gland polyps (El-Zimaity et al, 1997). H) Gastric cancer 1) In animal studies, a significant increase in gastric carcinoid tumors and ECL (enterochromaffin-like) cell hyperplasia has been reported with omeprazole. Human biopsies have been obtained from more than 3000 patients treated with omeprazole in long-term studies. These data show that the incidence of ECL cell hyperplasia increases with time. Despite these results, no case of ECL cell carcinoids, dysplasia, or neoplasia has been found in these 3000 subjects. Long-term studies are required to rule out the possibility of an increased risk of gastric tumors in patients receiving longterm omeprazole therapy (Prod Info Prilosec(R), 2001a). 2) Patients with Zollinger-Ellison syndrome have developed gastric carcinoids who received long-term omeprazole therapy. However, these developments are believed to be due to a manifestation of the underlying disease, which is known to be associated with such tumors, rather than a result of therapy (Prod Info Prilosec(R), 2001a). 3) Gastric polyps developed in 3 patients after 1-year of therapy with omeprazole. It is not known if omeprazole caused these polyps. The polyps were not malignant when they were discovered. However, it is not known if these changes were pre-malignant (Graham, 1992). Close monitoring of patients on long-term omeprazole therapy is recommended. I) Gastrointestinal tract finding 1) Anorexia, dry mouth, irritable colon, fecal discoloration, esophageal candidiasis, taste perversion, abdominal swelling, and mucosal atrophy of the tongue have occurred in less than 1% of treated patients; however, the relationship to omeprazole was unclear (Prod Info Prilosec(R), 2001a; Nielsen et al, 1985; Lauritsen et al, 1985). 2) In a case-control study, the gastric antisecretory action of omeprazole was associated with a 10-fold increase in the risk of campylobacter enteritis in patients aged 45 and older (n=211), particularly if the drug had been ingested within one month of infection (dose and therapy duration not provided). The authors ascribe this increased risk to campylobacter acid sensitivity combined with decreased gastric eradication of ingested organisms as a result of acid suppression. There was no correlation with previous gastric surgery, pernicious anemia, or concomitant medications, and H2 receptor antagonists demonstrated a dramatically lower relative risk in comparison (Neal et al, 1996). 3) An incidence analysis done in England showed that adverse effects associated with proton pump inhibitors (PPI) are infrequent and generally occur to a similar extent for each of the different PPI medications. The most common adverse events are diarrhea, abdominal pain, nausea/vomiting, and headache. A slightly higher incidence of diarrhea was found for lansoprazole users, especially in older patients. The incidence of diarrhea per 1000 treatment days was 0.18 for omeprazole, 0.39 for lansoprazole, and 0.23 for pantoprazole (p less than 0.001 lansoprazole compared to omeprazole) (Martin et al, 2000b). 4) Two case reports of esophageal candidiasis in patients receiving omeprazole are reported (Larner et al, 1992). There were no predisposing factors for the development of candidiasis in either patient. Omeprazole therapy was discontinued in both patients and anti-candidal therapy led to resolution of infection. The virtual abolition of intragastric acidity may predispose omeprazole-treated individuals to enteric infection. J) Hypergastrinemia 1) Omeprazole 20 milligrams once daily for 6 months in patients with healed duodenal ulcers was not associated with significant increases (p less than 0.05) in serum gastrin levels (Di Mario, 1996b). The effect of omeprazole treatment beyond 6 months on serum gastrin levels in humans has not been evaluated (Di Mario et al, 1996a). K) Nausea 1) Nausea (2.2% to 4%) has been associated with omeprazole therapy (Prod Info Prilosec(R), 2001a)(Cullen, 1998)(Yeomans, 1994a; Skoutakis et al, 1995d). L) Superinfection, Gastrointestinal 1) In patients with duodenal ulcers with pre-existing mycotic infection, antiulcer therapy for 6 weeks including omeprazole, was associated with increased fungal growth. The implications of this study suggest that omeprazole therapy may foster the growth of pre-existing saprophytic fungus to a level of pathogenic significance (Goenka et al, 1996). M) Vomiting 1) Vomiting (1.5% to 3.2%) has been associated with omeprazole therapy (Prod Info Prilosec(R), 2001a)(Cullen, 1998)(Yeomans, 1994a; Skoutakis et al, 1995d). 3.3.5 Hematologic A) Hematology finding 1) Less than 1% of patients taking omeprazole have experienced pancytopenia, thrombocytopenia, neutropenia, anemia, leukocytosis, and hemolytic anemia; however, the relationship to these events and omeprazole has not been determined (Prod Info Prilosec(R), 2001a). 2) A case of hemolytic anemia was reported in a 57-year-old female taking omeprazole 20 mg daily for esophagitis and duodenitis (Marks et al, 1991a). Two days after starting omeprazole therapy the patient developed weakness, lethargy, and shortness of breath. Two weeks after the initiation of therapy, her hematocrit had decreased from 44.1% to 20.4%, and she had a positive direct Coombs anti-globulin test and an elevated indirect bilirubin. Omeprazole was discontinued and her hematocrit gradually returned to normal with resolution of symptoms. The mechanism by which omeprazole can cause hemolytic anemia is unknown. 3) Another case involved a 75-year-old man treated with omeprazole and metoclopramide for esophagitis who developed anemia, azotemia, and elevated creatinine (ie, 3.48 mg/dL). Omeprazole and metoclopramide were discontinued and prednisolone started. Renal function improved with creatinine decreasing to 2.2 mg/dL. Two years later, the patient was retreated with omeprazole for esophagitis. Upon the start of therapy, the patient developed dyspnea, wheezing, diminished urinary output, raised jugular venous pressure, bilateral rales, and distended abdomen. Serum creatinine was 15.65 mg/dL. Omeprazole was discontinued, dialysis treatment ensued, and the patient's symptoms quickly resolved (Assouad et al, 1994). 4) A case report describes a 63-year-old man that developed fever, malaise, arthralgia, pronounced erythematous swelling in the metacarpophalangeal joints, Raynaud's phenomenon, and pitting edema after 2 weeks of starting omeprazole 20 mg daily. Erythrocyte sedimentation rate was 62 mm/h, IgA 563 mg/dL, and autoantibody screen revealed an antinuclear antibody titer above 1280. Omeprazole was discontinued and symptoms improved. There was no report of rechallenge (Sivakumar et al, 1994). 5) Neutropenia was described in a case report involving a 77-year-old woman receiving 3 weeks of omeprazole therapy for reflux esophagitis. The woman presented with episodes of syncope and was also receiving diazepam 2 to 5 milligrams (mg) nightly for 20 years and diflunisal 250 mg twice daily for osteoarthritis for 10 years. A complete blood count 10 months prior had been normal. A bone marrow aspirate indicated a deficiency of mature neutrophils with preservation of neutrophil progenitors and all other cell types. Following no significant neutrophil recovery after 7 days of discontinuing all medications, a single dose of granulocyte colonystimulating factor was administered, generating a restoration of the neutrophil count. Diazepam and diflunisal administration were resumed without a recurrence of neutropenia. The woman was not rechallenged with omeprazole (Holt et al, 1999). B) Hemolytic anemia 1) A case report describes the association of omeprazole with Heinzbody hemolytic anemia (HBHA). A 76-year-old female was admitted for "acute on" chronic renal failure. The patient had been started on omeprazole two months prior to admission. Before starting omeprazole therapy, the hemoglobin (Hgb) was 132 gram/liter (g/L). On admission, Hgb was 86 g/L. Blood histology revealed HB hemolysis with irregular spherocytes, bite cells, and polychromasia. Five days later, Hgb decreased further to 78 g/L. Upon discontinuation of omeprazole, Hgb almost immediately increased to 90 g/L with less HB bodies. Six weeks later, HB bodies were not detected and Hgb was 125 g/L. Due to the temporal relationship between omeprazole therapy and HBHA, it is suggested that omeprazole played a major role. However, additional reports with more conclusive evidence is needed to establish the relationship between omeprazole and HBHA (Davidson et al, 1997). C) Megaloblastic anemia 1) A 51-year-old male who received long-term omeprazole treatment (3 years of 40 to 60 mg daily) for gastroesophageal reflux disease developed megaloblastic anemia secondary to cobalamin deficiency. A 9-day treatment of intramuscular hydroxocobalamin 1000 mcg/day corrected the anemia within 3 months. The cause of this complication was attributed to a lack of release of dietary cobalamine caused by omeprazole therapy. The transfer of protein-bound cobalamin to R binder and intrinsic factor requires a normal secretion of hydrochloric acid and pepsin; a process affected by omeprazole therapy (Bellou et al, 1996). 3.3.6 Hepatic A) Hepatotoxicity 1) Incidence: rare 2) Hepatitis, including hepatic failure (rarely), and elevations in ALT (alanine aminotransferase, or serum glutamic oxalocetic transaminase (SGOT)), gamma glutamyl transpeptidase, alkaline phosphatase, and bilirubin resulting in JAUNDICE) have developed in less than 1% of patients; however, the relationship to omeprazole was unclear (Prod Info Prilosec(R), 2001a; Mears & Kaplan, 1996a; Gustavsson et al, 1983). 3) In another study, omeprazole 40 mg/day for 2 weeks did not alter serum alanine aminotransferase concentrations and there was no difference between omeprazole and placebo with respect to other liver function tests (Clissold & Campoli-Richards, 1986; Loof et al, 1984). 4) A case of fulminant hepatic failure and death was believed to be caused by omeprazole (Jochem et al, 1992). The patient was being treated with omeprazole 20 mg/day for erosive esophagitis. After seventeen days of treatment he presented to the hospital with worsening epigastric pain, anorexia, nausea, and vomiting. Liver function tests were markedly increased (they were normal before treatment started). The patient was given supportive care; however, the patient's condition worsened and he died. All serological tests for viruses were negative and other causes of hepatic failure were ruled out. 3.3.7 Immunologic A) Anaphylaxis 1) A 57-year-old male developed anaphylaxis after second exposure to omeprazole. Six weeks before the anaphylactic reaction, the patient was given omeprazole 20 mg orally. Treatment was discontinued due to urticaria. Upon second exposure to oral omeprazole (20 mg), the patient developed urticaria, angioedema, hypotension, became unconscious, then developed asystole. The patient later recovered without further complications. Skin tests, performed during a follow-up visit, confirmed that the patient was allergic to omeprazole. Although anaphylactic reactions to omeprazole are rare, clinicians should be aware of this potential reaction to omeprazole (Ottervanger et al, 1996). 2) A 35-year-old male with a history of hepatitis and pancreatitis from ethanol abuse experienced omeprazole-induced anaphylaxis demonstrated by skin tests and increased serum tryptase levels. The patient was administered intravenous (IV) omeprazole 40 milligrams (mg) diluted in 100 milliliters (ml) of saline solution twice daily and metamizole IV (an analgesic) for abdominal pain due to worsening pancreatitis. The patient had been previously hospitalized on multiple occasions for abdominal pain and was taking ranitidine, vitamin K, and metamizole at home. Omeprazole had been administered on other occasions. Following two days of therapy and within a few minutes after starting an omeprazole infusion, the patient experienced sweating, paleness, abdominal pain, itching on his legs, dyspnea, and hypotension (70/40 millimeters of mercury). No other medications had been administered during the previous 12 hours. Blood pressure returned to normal and symptoms resolved within one hour following administration of IV methylprednisolone, chlorpheniramine, and oxypolygelatin (fluid gelatin used as vascular filler in hypotension). Elevated serum tryptase levels (5.1 units/liter) were detected 6 hours after the onset of anaphylaxis and were normal at 24 and 48 hours (less than 2 units/liter). Skin intradermal tests were performed two months later and were positive with omeprazole IV (4 mg/ml), omeprazole capsules diluted in saline solution (20 mg/ml), and lansoprazole capsules diluted in saline solution (30 mg/ml). The same intradermal skin tests were negative in six control subjects. Serum specific IgE anti- omeprazole was not detected by an radioimmunoassay (Galindo et al, 1999). B) Carcinogen effect 1) The manufacturer reports experience with long-term use of omeprazole in over 3000 patients. The incidence of ECL cell hyperplasia did increase with time; however, none of the patients developed carcinoids, dysplasia, or neoplasia (Prod Info Prilosec(R), 2001a). 2) According to the FDA Gastrointestinal Drugs Advisory Committee, the risk of atrophic gastritis, intestinal metaplasia, or gastric adenocarcinoma are not increased by long-term antisecretory drug treatment (Langtry & Markham, 1999). 3) High-dose omeprazole has caused an increase in gastrin concentrations in animals. In a majority of the test animals, a prolonged period of increased gastrin concentration led to the development of precursor cells to gastric carcinoma. However, the correlation in humans between gastrin concentration and gastric carcinomas is weaker than that observed in animal studies. Gastric biopsies of over 5,000 patients receiving long-term omeprazole therapy have shown no signs of hyperplasia or neoplasia (Skoutakis et al, 1995d) C) Cellular change 1) Cellular changes associated with omeprazole maintenance therapy include enterochromaffin-like cell hyperplasia, parietal cell protrusions (hypertrophy), and increased development of fundic gland cysts, based on a randomized, double-blind trial (n=83) (Cats et al, 2000). Parietal cell protrusion occurred in both Helicobacter-positive and -negative patients, developed in the first months of omeprazole therapy, and was significantly associated with increased serum gastrin levels. The prevalence of parietal cell protrusion increased from 18% at baseline to 79% at 3 months and 86% at 12 months (p less than 0.001). Prevalence of fundic gland cysts increased from 8% at baseline to 17% and 35% at 3 and 12 months, respectively (p less than 0.05, 12 months); fundic gland cysts developed more often in H pylori-eradicated patients compared with H pylori-persistent patients. Whether fundic gland cysts may further enlarge and progress to fundic gland polyps is uncertain. 2) Omeprazole therapy was shown to induce parietal cell hypertrophy and hyperplasia in humans (Driman et al, 1996a). Parietal cell height, mass, and number were increased in omeprazole-treated patients compared to ranitidine-treated patients and patients on neither drug. Overall, 33 biopsies of patients using omeprazole were examined; doses of omeprazole ranged from 20 to 80 mg daily, and duration of therapy varied from 4 weeks to 5 years. Though not significant, there was a trend toward increased parietal cell enlargement correlating with greater length of omeprazole treatment. The authors suggested that hypergastrinemia may be one of the mechanisms contributing to parietal cell changes. It was also noted that in patients who terminate omeprazole, rebound acid hypersecretion is likely to be the result of parietal-cell hypertrophy and hyperplasia. D) Genetic mutation 1) The manufacturer reports experience with long-term use of omeprazole in over 3000 patients. The incidence of ECL cell hyperplasia did increase with time; however, none of the patients developed carcinoids, dysplasia, or neoplasia (Prod Info Prilosec(R), 2001a). 2) According to the FDA Gastrointestinal Drugs Advisory Committee, the risk of atrophic gastritis, intestinal metaplasia, or gastric adenocarcinoma are not increased by long-term antisecretory drug treatment (Langtry & Markham, 1999). 3) High-dose omeprazole has caused an increase in gastrin concentrations in animals. In a majority of the test animals, a prolonged period of increased gastrin concentration led to the development of precursor cells to gastric carcinoma. However, the correlation in humans between gastrin concentration and gastric carcinomas is weaker than that observed in animal studies. Gastric biopsies of over 5,000 patients receiving long-term omeprazole therapy have shown no signs of hyperplasia or neoplasia (Skoutakis et al, 1995d) 3.3.8 Musculoskeletal A) Hip fracture 1) Long-term use of proton pump inhibitors (PPI) has been associated with increased risk of hip fractures in a dose-response and duration-response manner. In a United Kingdom, case-control study utilizing 15 years of data (1987 to 2003) from the General Practice Research Database (GPRD), 13,556 hip fracture cases and 135,386 controls were identified. The mean age was 77 +/- 9.3 years and the vast majority (80%) of patients were female. Eligible participants had at least 12 months of cumulative use of acid suppressive therapy and the last prescription filled was no less than 6 months prior to the index date. The estimated crude hip fracture incidence rate was 4 per 1000 person-years among long-term users of PPI and 1.8 per 1000 person-years among acid suppression non-users. Accounting for all potential confounders, such as patient demographics, risk factors for falling, medication exposure, and comorbidity status, the adjusted odd ratio (AOR) for hip fracture was 1.44 (95% confidence interval (CI), 1.3 to 1.59; p less than 0.001) associated with PPI therapy beyond 1 year, and 1.23 (95% CI, 1.14 to 1.39; p less than 0.001) with histamine-2 receptor antagonists (H2RA) therapy. The corresponding AOR for hip facture was statistically higher for long term therapy of PPI than H2RA (1.34; 95% CI, 1.14 to 1.38; p less than 0.001). The hip facture risk of PPI therapy increased further when PPI-only users were compared with acid suppression non-users (AOR 1.62; 95% CI, 1.41 to 1.89; p less than 0.001). The association of hip fracture risk increased progressively with the duration of PPI therapy: AOR 1.22 (95% CI, 1.15 to 1.3) for 1 year, AOR 1.41 (95% CI, 1.28 to 1.56) for 2 years, AOR 1.54 (95% CI, 1.37 to 1.73) for 3 years, and AOR 1.59 (95% CI, 1.39 to 1.8) for 4 years (all p less than 0.001). There was also a doserelated increase in hip fracture risk among long-term users of PPI therapy: AOR 2.65 (95% CI, 1.8 to 3.9) above 1.75 average daily dose vs 1.4 (95% CI, 1.26 to 1.54) at or below 1.75 average daily dose. Of note, the associated hip facture risk with long-term use of PPI therapy was stronger among men (odd ratio (OR) 1.78; 95% CI, 1.42 to 2.22) than women (OR 1.36; 95% CI, 1.22 to 1.53) (p=0.04) (Yang et al, 2006). B) Musculoskeletal finding 1) Muscle cramps, myalgias, joint pain, and leg pain have developed in less than 1% of patients during treatment; however, the relationship between these events and omeprazole is unclear (Prod Info Prilosec(R), 2001a). 2) Back pain has developed in 1.1% of patients receiving omeprazole therapy (Prod Info Prilosec(R), 2001a). 3.3.9 Neurologic A) Asthenia 1) Asthenia (1.2%) has developed during omeprazole therapy (Prod Info Prilosec(R), 2001a; Mears & Kaplan, 1996a; Skoutakis et al, 1995d). B) Central nervous system finding 1) Psychic disturbances including depression, aggression, hallucinations, confusion, insomnia, apathy, nervousness, anxiety, somnolence, abnormal dreams, vertigo, paresthesias, hemifacial dysesthesias, fatigue, and malaise have developed in less than 1% of patients (Prod Info Prilosec(R), 2001a); (Dive et al, 1986)(Meyrick-Thomas et al, 1984). However, the relationship to these events and omeprazole has not been determined (Prod Info Prilosec(R), 2001a). 2) One case report suggests that omeprazole was the cause of gait ataxia in a 27-year-old female. The patient, taking omeprazole for 4 months to treat heartburn, experienced unsteadiness of stance and gait, the sensation of near-falling, and transient horizontal diplopia. Upon withdrawal of the drug, patient reported a complete clinical recovery. No other cases of omeprazole-induced ataxia have been reported (Varona, 1996). C) Dizziness 1) Dizziness (1.5%) has developed during omeprazole therapy (Prod Info Prilosec(R), 2001a; Mears & Kaplan, 1996a; Skoutakis et al, 1995d). D) Headache 1) Headache (2.9% to 6.9%) has developed during omeprazole therapy (Prod Info Prilosec(R), 2001a; Mears & Kaplan, 1996a; Skoutakis et al, 1995d). E) Mental state finding, Changes 1) A case report describes a 64-year-old male who experienced serious mental changes after 2 months of omeprazole therapy. Other symptoms included headaches, diarrhea, and DROWSINESS. Upon withdrawal of omeprazole, the patient regained full awareness within 2 days. The patient was rechallenged with omeprazole 40 milligrams once daily. Changes in the patient's mental status were observed which included dizziness and headaches. Within 13 days, lethargy developed along with periods of ABSENTMINDEDNESS and INCOHERENT SPEECH. Upon withdrawal after omeprazole rechallenge, the patient experienced a quick recovery. The temporal relationship between the central nervous system side effects and omeprazole therapy (start and withdrawal of therapy) provides the only evidence that omeprazole may have been the causative agent (Meeuwisse et al, 1997). 3.3.10 Ophthalmic A) Disorder of eye 1) Nineteen cases of unspecified visual disturbances, in some cases leading to blindness, during intravenous or oral omeprazole therapy have been reported in Europe. The manufacturer states that all cases occurred in patients who were critically ill or had predisposing factors and that a causal relationship to omeprazole cannot be determined (Prod Info Antra(R), 1994). A review of case reports describing ocular toxicity concluded that omeprazole had no role in ocular effects (Creutzfeldt, 1994a). 2) Another large cohort study demonstrated that the ocular disorder, incidence rate ratio among omeprazole users is 0 (95% CI: 0 to 12.1). Past users of omeprazole demonstrated a rate ratio of 3.2 (95% CI: 0.43 to 16.2). These results indicate that omeprazole is associated with minimal to no increased risk for ocular disorders (Mannino et al, 1998). 3) A cohort study involving 33,988 patients demonstrated only a small increase in the relative risk (1.8; 95% CI 0.5 to 6) of ocular vascular or inflammatory disorders associated with omeprazole use. Data from this study demonstrated that omeprazole is not associated with a MAJOR increase in risk of ocular toxicity (Rodriguez et al, 1996). B) Eye / vision finding 1) Ocular effects occurring in less than 1% of patients include blurred vision, double vision, eye irritation and dry eye syndrome. Other reported ocular effects include optic atrophy, anterior ischemic optic neuropathy, and optic neuritis (Prod Info Prilosec(R), 2003a). 3.3.11 Otic A) Tinnitus 1) Tinnitus has developed in less than 1% of patients; however, the relationship to this effect and omeprazole has not been determined (Prod Info Prilosec(R), 2001a). 3.3.13 Renal A) Interstitial nephritis 1) Summary a) Several case reports have described omeprazole- induced interstitial nephritis. The onset varies from 1 week to 6 months of starting omeprazole therapy. Upon discontinuing omeprazole, symptoms rapidly resolve. 2) Incidence: rare 3) A case of acute interstitial nephritis occurred in a 74-year-old woman treated with omeprazole 20 mg daily for reflux esophagitis. After six months of omeprazole therapy the patient presented with generalized malaise, fatigue, and anorexia. Her BUN and creatinine levels were elevated. She was diagnosed with drug-induced acute interstitial nephritis secondary to omeprazole. Omeprazole was discontinued and her laboratory abnormalities resolved. A rechallenge 5 weeks later with omeprazole 20 mg daily produced generalized malaise, fatigue, anorexia, and abnormal renal function tests after only two days of therapy. The omeprazole was discontinued and her symptoms resolved rapidly (Ruffenach et al, 1992). 4) A case report involving 2 elderly patients demonstrated the association of omeprazole (20 milligrams/day) therapy with acute interstitial nephritis. In one patient, the symptoms occurred within 2 weeks of initiating omeprazole. The other patient had developed symptoms after 3 months of initiating omeprazole. In both cases, the symptoms improved upon withdrawal of therapy and redeveloped after rechallenge (Badov et al, 1997). 5) A 70-year-old woman was diagnosed with omeprazole-induced interstitial nephritis within 3 weeks of starting omeprazole for dyspepsia. One week after starting omeprazole, the patient developed fatigue for 2 weeks which was then followed by fever. Twenty-four hours after the patient developed fever, she visited her physician. Laboratory (lab) tests suggested a urinary tract infection and the patient was prescribed ofloxacin. Five days later, the patient's white blood cell count (16,000/mm(3)), BUN (56 mg/dL), and serum creatine (5.2 mg/dL) were still high and had increased from the first set of tests. Upon further evaluation, the patient was diagnosed with omeprazole-induced interstitial nephritis. Within 2 weeks of discontinuing omeprazole, the patient's symptoms resolved and lab tests were almost normal (Portera-Calliau & Salazar, 1999). 6) Hypercalcemia, renal lesions, and ACUTE INTERSTITIAL NEPHRITIS were associated with OMEPRAZOLE therapy in a 31-year-old female. After pregnancy (complicated by high blood pressure) and delivery of a healthy baby girl, the patient was stabilized on nifedipine (long-acting 30 mg/day) for hypertension, with omeprazole 20 mg/day her only other medication. Over 8 weeks, she developed asymptomatic hypercalcemia (serum calcium 3.22 mmol/L; normal, 2.2 to 2.7 mmol/L) and renal function deterioration. A percutaneous renal biopsy found intense eosinophilic infiltrates and tubuledestructive granulomata. Omeprazole had been discontinued 2 weeks prior to the biopsy. The patient was given prednisolone 40 mg/day, leading to normalization of serum calcium and improvement in kidney function; at 18 months follow-up, mild renal dysfunction persisted. The authors concluded that omeprazole induced the granulomatous lesions and associated hypercalcemia (Wall et al, 2000). B) Urogenital finding 1) In less than 1% of patients, development of urinary tract infections, microscopic pyuria, urinary frequency, proteinuria, hematuria, glycosuria, testicular pain, and elevated serum creatinine has occurred. However, the relationship to these events and omeprazole has not been determined (Prod Info Prilosec(R), 2001a). 2) Painful NOCTURNAL ERECTIONS have been reported with omeprazole (Anon, 1991). 3) An 86-year-old woman with a 10-year history of esophagitis received omeprazole 40 mg/day after failing ranitidine and cimetidine therapy. Two months later, she was admitted for renal failure (creatinine 11 mg/dL). Renal biopsy revealed interstitial inflammation. Several years later, she was again treated with omeprazole and within a week developed diminished renal function which progressed to anuria. Omeprazole was discontinued but renal function remained severely affected; after 3 months serum creatinine declined from 11 to 5 mg/dL (Christensen et al, 1993). 3.3.15 Respiratory A) Community acquired pneumonia 1) The risk of community-acquired pneumonia (CAP) may be higher among users of gastric acid-suppressive drugs, including proton pump inhibitors (PPI) and histamine-2 receptor antagonists (H-2RA); a dose-response relationship was observed for PPI use and risk of CAP. These findings were based on a retrospective analysis of 364,683 medical records of Dutch patients seen by general practitioners (tracked in the Integrated Primary Care Information database). Rates of pneumonia were 2.5 per 100 personyears in PPI users, 2.3 per 100 person-years in H-2RA users, and 0.6 per 100 person-years in non-users of PPI or H-2RA drugs. Average duration of use was 5 months for PPI and 2.8 months for H-2RA. The unadjusted relative risk of CAP amounted to 1.0 among non-users compared with 4.63 (95% confidence interval (CI) 3.84 to 5.43) for the PPI group and 4.24 (95% CI 3.18 to 5.43) for the H-2RA group. A further examination included a nested case-control analysis where each case of pneumonia during or after PPI or H-2RA use was matched with up to 10 controls (acid suppression user, current or in the past, but no CAP), and odds ratios (OR) were derived for PPI and H-2RA classes, as well as individual medications. For current users of acid-suppressive drugs, the adjusted OR for CAP was 1.27 (95% CI 1.06 to 1.54). For current PPI users, the adjusted OR for CAP was 1.73 (95% CI 1.33 to 2.25); for H-2RA users, it was 1.59 (95% CI 1.14 to 2.23). In current OMEPRAZOLE users, OR was 1.74 (1.28 to 2.35). Overall, there was roughly 1 case of pneumonia for every 226 patients treated with a PPI and 1 case per 508 patients treated with a H-2RA. The mechanism for a higher CAP risk was thought to be a reduction of gastric acid secretion, facilitating oral infections (Laheij et al, 2004). B) Respiratory finding 1) Cough has been observed in 1.1% of patients (including duodenal ulcer, Zollinger-Ellison syndrome, and resistant ulcer patients) on omeprazole therapy (Prod Info Prilosec(R), 2001a). 2) Epistaxis and pharyngeal pain have occurred in less than 1% of patients; however, a relationship between these side effects and omeprazole is unclear (Prod Info Prilosec(R), 2001a). 3.4 Teratogenicity/Effects in Pregnancy/Breastfeeding A) Teratogenicity/Effects in Pregnancy 1) U.S. Food and Drug Administration's Pregnancy Category: Category C (Prod Info Prilosec(R), 2002) (All Trimesters) a) Either studies in animals have revealed adverse effects on the fetus (teratogenic or embryocidal or other) and there are no controlled studies in women or studies in women and animals are not available. Drugs should be given only if the potential benefit justifies the potential risk to the fetus. 2) Australian Drug Evaluation Committee's (ADEC) Category: B3 (Batagol, 1996) a) Drugs which have been taken by only a limited number of pregnant women and women of childbearing age, without an increase in the frequency of malformation or other direct or indirect harmful effects on the human fetus having been observed. Studies in animals have shown evidence of an increased occurrence of fetal damage, the significance of which is considered uncertain in humans. See Drug Consult reference: "PREGNANCY RISK CATEGORIES" 3) Crosses Placenta: Yes 4) Clinical Management a) The manufacturer has received several reports of congenital abnormalities in infants born to women who were given omeprazole during pregnancy (Prod Info Prilosec(R), 2002). However, several studies and case reports have failed to demonstrate an increase in congenital abnormalities with omeprazole (Diav-citrin et al, 2005; Nikfar et al, 2002; Kallen, 2001). Although adverse effects have been reported in humans, a direct cause and effect relationship has not been proven. Omeprazole achieves fetal tissue concentrations similar to that achieved in plasma (Mears & Kaplan, 1996).