doctors
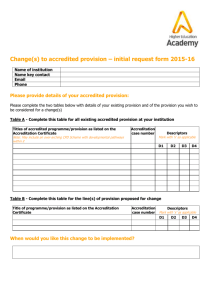
advertisement
http://www.consumerhealthjournal.com/articles/regulated-doctor-shortage.html Regulated Medical School Admissions Protects Doctor Shortage and High Physician Salaries February 2004 by Alison Stewart Have you ever waited to see a doctor even though you were on time for your appointment? Do you feel like doctors are doing you a favor by squeezing you into their schedules? These may be symptoms of a physician shortage that some say is regulated by doctors' organizations to maintain physician salaries and limit competition. From 1990 to 2000, the number of U.S. medical school graduates increased 2 percent, from about 15,400 to 15,700 graduates, according to the Association of American Medical Colleges (source), though during the same period the U.S. population increased 13 percent, according to census data. Although the number of active doctors has increased due to factors like retirement rates, foreign and osteopathic medical school graduates, American medical schools are not keeping up with population growth. "All we're doing right now is forcing a large number of people who want to go to medical school to go to foreign medical schools," said Dr. Martin Litwin, professor of surgery at the Tulane School of Medicine. "We now have a country full of people who weren't trained in the United States," he said. And this stagnation of the number of medical students is occurring at a time of high demand for doctors, high physician salaries and skyrocketing medical costs. The median income for U.S. physicians, after expenses, was $160,000 in 1998, according to the Bureau of Labor Statistics. Compare this with other lucrative professions that require post-college education: According to the Bureau of Labor Statistics, the 2000 median lawyer salary was $88,000 and doctors of Electrical Engineering earned a 2000 median of about $90,000, according to a 2001 National Association of Colleges and Employers survey. These relative high salaries contribute to the ballooning cost of health care. Average per capita health spending in 2001 was $5,035, according to the Heartland Institute, while the median household income in 2001 was $42,200, according to census information. Economic principles say high prices and long waits can be lowered with more supply. So why not graduate more physicians? According to census data, the number of computer science graduate students at doctorate-granting schools increased 24 percent between 1990 and 1999, to meet the needs of our increasingly high-tech society. Why not more medical doctors to lower costs and reduce waits? One argument is the number of applicants is dropping. In 1992, there were about 37,500 applicants. In 2001, there were only about 35,000 applicants. "With our nation facing new health challenges and a possible physician shortage, the apparent flagging interest in the medical profession, as reflected by the shrinking applicant pool over the last several years, has been cause for some concern," said AAMC president Dr. Jordan Cohen in an AAMC, October 30, 2002 press release. "We are now at risk of reducing the quality of medical school grads if we simply increase numbers and seek less well qualified applicants," said Dr. Steven Gambert, professor of medicine at Johns Hopkins University School of Medicine. "This is another reason to keep numbers smaller but quality higher." But though there were fewer applicants to choose from, their quality was higher, based on GPAs and MCAT test scores. In 2001, the mean MCAT scores were higher than in 1992 (an average of 8.9 for the three sections, vs. a 1992 average of 8.2) and the mean applicant GPA rose from 3.24 to 3.45 from 1992 to 2001, according to data on the AAMC website. Even with the higher applicant quality, only 47 percent were accepted, compared with 44 percent in 1992. "Why aren't we building more medical schools and admitting more people to medical school?" Litwin said. There are 126 accredited medical schools in the U.S. There have been two newly accredited schools since 1980: Mercer University School of Medicine in Georgia, which received full accreditation in 1986, and Florida State University College of Medicine, which received provisional accreditation in 2002. That’s an annual increase of less than 0.1 percent, an order of magnitude smaller than the U.S. population growth rate of about .9 percent, according to the 2002 CIA World Factbook. But "It's not as simple as a generalization about the U.S. population size and lots of students generally wanting to enter the profession," said John Whiton, manager of enrollment services for the AAMC. One argument for why there aren't more new schools is that the costs are prohibitive. "It costs quite a bit to start a new medical school" said Dr. David Stevens, vice president of the medical school standards and assessment for the AAMC, and current secretary of the Liaison Committee on Medical Education, or LCME, the group in charge of accrediting new medical schools. Stevens said medical schools are different from other types of schools. "It's a far more complex part of our society than a number of other disciplines so it's not special, it just happens to be more complex," he said. "You as a taxpayer have a much different view. You have a vested interest in that, both as a taxpayer or a person who wants to attain medical care." Stevens said there wasn‘t anything to stop someone from starting a new medical school, but it was thought to be a bad investment. "[The costs are] perceived to be roughly two-to-three times what tuition pays for, and that additional income comes from state subsidies [and] from research grants," Stevens said. However, despite the costs, foreign schools that aren't regulated by the LCME operate without U.S. governmental subsidy, though some argue the schools' standards are not so high as U.S. schools. Another key piece in explaining why the U.S. doesn't have more schools or more medical students is that the medical school system is not entirely marketdriven, but is tightly regulated. U.S. medical schools are accredited by the LCME, recognized by the U.S. department of Education as being qualified to make judgments on the quality of potential and current medical programs. The LCME is jointly run by the Association of American Medical Colleges, or AAMC, and the American Medical Association, or AMA, organizations run by physicians. When U.S. medical schools begin, they must be accredited by the LCME and the schools decide, at that point, how many students they are equipped to admit each year. And after a school is created, it needs to be continually surveyed by the LCME. If it wants to expand, the expansion must be approved. "If a school chooses to increase its class size and it doesn't have the resources, they jeopardize their accreditation," said Dr. Frank Simon, director of undergraduate and graduate medical education, policy and standards for the AMA. However, some drawbacks to this system, in which doctor-run organizations control the accreditation process, were highlighted during the Ross University School of Medicine's bid to open a campus in Casper, Wyoming. Currently, states allow doctors educated in foreign countries to practice medicine, so long as they pass the licensing exam and test of English. But no foreign school has been allowed to create a campus in the United States. Ross University, located on the Caribbean island of Dominica, saw an opportunity in Wyoming because there is no medical school in the state. Outside the medical community, there was support for a medical school that would graduate doctors into the region. The governor at the time, Jim Geringer, wrote in a 1999 statement of support for Ross, "The teaching facility proposed by Ross University in Casper has my continuing support. The efforts by all involved should continue to focus on the benefits that would come to Wyoming's economy and to the health capacity of the nation." And the Casper Area Economic Development Alliance was excited about a Ross school in Wyoming, said CAEDA Vice President Liz Becher. "Our economic development group was very much supportive because of the workforce training [and] jobs that could be created," Becher said. However, many in the medical community resisted, arguing that schools not accredited by the LCME were not up to standard. "The criteria to get into the school is a check that won't bounce," said Casper surgeon Dr. Jerry Behrens, in Elisabeth A. Wright's 1999 article, "Why can't Wyoming get its own med school?" The Natrona County Medical Society, the area medical group, opposed Ross and played a role in Ross's eventual failure to establish a Wyoming campus. "The reservations had to do with accreditation," said Lynne Whalen, executive director of the NCMS. "All American medical schools are accredited. It's a quality check on the physicians that practice in the country," she said. Eventually, Ross withdrew its bid and Wyoming still does not have a medical school. A variety of explanations have been given to why the school failed to create a campus. "Ross wasn't accredited in Wyoming because they didn't apply," said Nicole Buckley, media relations officer to the AAMC. But George Howley, the 1999 director of CAEDA, saw it differently. In Wright's article, he said doctors are opposed to the potential competition, not to the supposed risk of lower-quality care. "To protect the income to the doctors is what it is," he said.