Anemias
advertisement

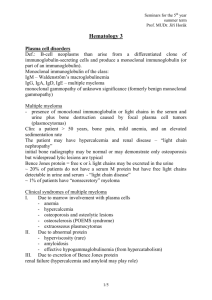
Seminars for the 5th year summer term Prof. MUDr. Jiří Horák Hematology (1) Disorders of the hematopoietic stem cell Myeloaplastic disorders - a deficiency of the production of the cells of the marrow but the cells that are produced are normal; Myelodysplastic disorders - ineffective production of cells that are abnormal in morphology and biochemistry; Myeloproliferative disorders - overproduction of one or more of the cell lineages. The cells may also have dysplastic characteristics. The boundaries among these categories are not always distinct. The myeloaplastic disorders Diminished production of cells in the marrow results in peripheral cytopenia. When the stem cell is affected, the proliferation of all cell lineages is diminished -> pancytopenia ("aplastic anemia"). In other cases, only a single line may be afflicted (e.g., amegakaryocytic thrombocytopenia). Congenital myeloaplastic disorders Congenital defect in the stem cell -> aplastic anemia (Fanconi's syndrome). Acquired aplastic anemia Pancytopenia of variable degree can occur secondary to chemotherapeutic agents or to irradiation, or as an idiopathic acquired condition. The cytotoxic drugs designed to treat malignancy usually interrupt the cell cycle or alter intracellular processes so that cell death supervenes. Stem cell function can also be markedly reduced by viruses. Idiopathic acquired aplastic anemia is thought to be due primarily to autoimmune suppression of the stem cells. Clin: aplastic anemia is a disease of young adults, with peak incidence at age 20 to 25, and of the elderly ~ 60 to 65. Men and women are equally affected. Usually all three cell lines in the peripheral blood are deficient in number but normal in morphology. The reticulocyte count is reduced; the marrow is hypoplastic and may contain primarily lymphocytes. Therapy supportive - transfusions of red blood cells or platelets as needed and the appropriate use of antibiotics. Transfusions should be limited in patients who are candidates for bone marrow transplantation, as they may induce alloimmunization. The most definitive treatment of severe 1/12 Seminars for the 5th year summer term Prof. MUDr. Jiří Horák aplastic anemia is bone marrow transplantation; it is age-limited (< 50 years) and the overall success rate in aplastic anemia is 70%. When bone marrow transplantation is not an option, immunosuppression using antithymocyte or antilymphocyte globulin and cyclosporine (a T cell suppressing agent) is about equally successful. The overall survival is ~ 60%. The myelodysplastic disorders All three lines are usually affected. All may result in acute myeloblastic leukemia. Myelodysplastic syndromes (MDSs). A slow and insidious development of bone marrow failure characterized by anemia and thrombocytopenia or a combination of both. MDSs especially appear to occur after treatment for Hodgkin's disease or ovarian carcinoma but may occur after any chemotherapy with alkylating agents. The anemia in MDSs is typically macrocytic. The bone marrow is typically hypercellular with increased iron stores and morphologically abnormal erythroid precursors. Hypocellular bone marrow in MDSs imparts a poor prognosis. Increased immature myeloid forms (blasts) may herald progression to acute leukemia. Treatment of MDSs is primarily directed toward improving the cytopenias. Transfusions of red blood cells and platelets. Some patients with refractory anemia with ringed sideroblasts respond to large doses of pyridoxine. Growth factors, esp. recombinant human erythropoietin may improve the anemia in some patients. Bone marrow transplantation in younger patients should be considered. Paroxysmal nocturnal hemoglobinuria is an acquired stem cell disorder characterized by intravascular hemolysis, unusual venous thromboses, and evidence of diminished hematopoiesis. It is the result of the somatic mutation of a gene on the X chromosome of a stem cell. Clin: hemoglobinuria results from the intravascular hemolysis of the abnormal cells. The hemoglobinuria is nocturnal because complement is activated at night and is paroxysmal because complement is activated by 2/12 Seminars for the 5th year summer term Prof. MUDr. Jiří Horák infections, physical stress etc. It results in a marked loss of iron in the urine. It can result in acute renal failure and in chronic renal damage. Venous thromboses occur in ~ 40% of patients. Lab: intravascular hemolysis + neutropenia and/or thrombocytopenia. Ham acidified serum lysis test: hemolysis of the abnormal red cells by the activation of complement. Th: bone marrow transplantation. Glucocorticoids may diminish the activation of complement in moderately high doses (15 to 30 mg/day in adults). Anabolic steroids may also improve the anemia. All patients (except those receiving transfusions) should take iron and folic acid supplements. Mean survival is 8 to 12 years. Myelofibrosis is characterized by abnormal hematopoiesis and replacement of the bone marrow by fibrous tissue. Disruption of the structure of the marrow -> circulation of immature cells. Extramedullary hematopoiesis. The primary problem may be dysplasia of the megakaryocytes, which results in the local elaboration of cytokines that promote the growth of fibrous tissue. Clin: myelofibrosis is a chronic disease of the middle aged and elderly. Anemia, hepatosplenomegaly, with time other cytopenias. The bone marrow cannot be aspirated, but the biopsy shows strands of fibrous tissue with nests of hematopoietic cells. Megakaryocytes are plentiful and are often bizzare in morphology, with hyposegmentation of the nucleus. Th: the most definite treatment is bone marrow transplantation. Mild chemotherapy, such as 6-mercaptopurine 100 mg/day may be used in the proliferative phase. Splenectomy may be necessary. The mean survival from diagnosis is 5 to 10 years. Myeliproliferative disorders The cells are normally differentiated (except for the acute leukemias) but appear to have escaped the usual controls on growth. The ultimate result may be acute myeloblastic leukemia. Polycythemia rubra vera A clone of stem cells produces erythroid precursors autonomously. The production of erythropoietin is suppressed. 3/12 Seminars for the 5th year summer term Prof. MUDr. Jiří Horák Clin: older persons are affected. Plethora of the face, splenomegaly in > 60% of patients. Patients may have erythromyalgia of the feet and may have pruritus, esp. after a bath. The hematocrit is usually > 53%. The red cells are normal in appearance but may be hypochromic if iron deficiency is present. The white count is often elevated above 12,000/mm 3, and the platelet count is above 450,000/mm3. Arterial hypoxia is not present. The plasma erythropoietin level is usually undetectable. The leukocyte alkaline phosphatase is often elevated in the absence of infection. Course of the disorder and treatment Polycythemia vera is a chronic disorder that is complicated by thromboses (frequently arterial) that terminates either in leukemia or myelofibrosis. Patients with nonaggressive and mild disease may be treated with phlebotomy, whereas those with increased platelet counts or any tendency to thrombosis should be treated with hydroxyurea. Alkylating agents (chlorambucil) and P32 often lead to leukemia and other neoplasms. Chronic myelogenous leukemia (CML) Def: a malignant stem cell disorder classified as a myeloproliferative disease. The Philadelphia (Ph1) chromosome is a translocation of the long arm of chromosome 22 to chromosome 9. The product of this translocation is a tyrosine kinase, which promotes granulocyte proliferation. CML usually occurs in adults but can occur at any age. CML is often found incidentally when an elevated white blood cell count is found. Thrombocytosis is often present. The spleen is usually enlarged. Bone marrow examination reveals myeloid hyperplasia without a significant increase in blast forms. Megakaryocytes may be increased. Th: the antimetabolite hydroxyurea (a ribonucleotide reductase inhibitor) is used as initial "debulking" treatment (formerly busulfan). Alpha-interferon, alone or combined with cytosine arabinoside, may decrease the number of Ph1-positive cells in the bone marrow and enrich the normal clone of cells. Bone marrow transplantation represents the only potentially curative means of treating CML. Most patients with CML present in the "chronic" phase of the disease, which usually last from 3 to 5 years. Adverse prognostic features include advanced age, basophilia, severe thrombocytosis, or more than one chromosome abnormality. 4/12 Seminars for the 5th year summer term Prof. MUDr. Jiří Horák "Accelerated" phase - the white blood cell count and splenomegaly become more difficult to control. Either thrombocytopenia or marked thrombocytosis may herald the accelerated phase. "Blast crisis" - a genuine acute leukemia, which is usually of myeloid phenotype. The treatment of blast crisis is difficult and unsatisfactory. Usually, blast crisis ends in death between 3 and 6 months after its appearance. Essential thrombocythemia It is due to a clonal growth of stem cells that produce excess numbers of megakaryocytes. The clinical manifestations are primarily those of thrombosis in small or large vessels. Dg: increased platelet count (> 600,000/mm3) in the absence of other causes (infection, iron deficiency, nonhematologic malignancy) that persists over at least 2 months. The platelets may appear abnormal. Splenomegaly may be present. The bone marrow is usually cellular and contains large number of megakaryocytes. Th: plateletapheresis (in patients with cerebral symptoms). Hydroxyurea is commonly used. Patients with essential thrombocythemia rarely progress to leukemia but may have myelofibrosis as a late complication. Acute leukemia The acute leukemias are divided into two broad categories: acute lymphoblastic leukemia (ALL) and acute myeloblastic leukemia (AML). ALL is primarily a disease of children and represents > 90% of the acute leukemias in this age group. AML represents at least 80% of acute leukemias in the age group over 20 years. French - American - British (FAB) classification of acute leukemia Acute myelocytic leukemia M1 M2 acute myelocytic leukemia without differentiation acute myelocytic leukemia with differentiation M3 acute promyelocytic leukemia M4 acute myelomonocytic leukemia M5 acute monocytic leukemia M6 M7 erythroleukemia megakaryocytic leukemia 5/12 Seminars for the 5th year summer term Prof. MUDr. Jiří Horák Acute lymphocytic leukemia L1 predominantly "small cells" (twice the size of normal lymphocyte), homogeneous population; childhood variant L2 larger than L1, more heterogeneous population; adult variant L3 "Burkitt-like" large cells, vacuolated abundant cytoplasm Diagnosis is initially suspected by morphologic evaluation of the peripheral blood and bone marrow aspiration and biopsy and may then be confirmed by using histochemical stains and immunophenotyping of surface and cytoplasmic markers. Chromosome studies are helpful. Clin: anemia, thrombocytopenia -> fatigue, malaise, bleeding, and infection. Th: If the white count is > 100,000/µl, the patient is at high risk for leukostasis (obstruction as small vessels by rigid blast cells). Therapeutic leukopheresis and specific chemotherapy should be initiated immediately. The goal of treatment is to destroy the leukemic cells and produce a complete remission during which leukemia cells cannot be found in the peripheral blood or bone marrow. Initial therapy = induction. In AML: cytosine arabinoside, usually given as a 7-day infusion along with a second drug, usually an anthracycline such as daunorubicin, idarubicin, or mitoxantrone. Induction chemotherapy for AML produces complete remission in ~ 75% of patients under 60 years of age and in ~ 50% of patients over 60. Chemotherapy given soon after the induction of complete remission is termed "consolidation" chemotherapy and may employ the same drugs. In AML, an exact schema is not universally agreed upon. Long-term disease-free survival in younger patients with AML has been described in up to 30% of patients treated by conventional means and in a similar proportion of patients who go on to bone marrow transplantation. Th of ALL: initial induction usually involves multiple agents, including vincristine, prednisone, daunorubicin, cyclophosphamide, and Lasparaginase. In children, up to 90% of patients achieve complete remission, and an increasing proportion of patients are alive and in complete remission > 5 years after initial induction. The aggressive longterm maintenance chemotherapy lasts up to 2 or 3 years with early prophylaxis of the CNS with intrathecal chemotherapy with or without whole brain radiation. Th of acute promyelocytic leukemia is unique. All trans retinoic acid (ATRA, tretinoin) binds to the retinoic acid receptor, a part of the 6/12 Seminars for the 5th year summer term Prof. MUDr. Jiří Horák t(15,17) translocation. In most patients, this stops the process of DIC and may lead to maturation of the leukemic clone into "normal" granulocytes. Disorders of Lymphocytes Lymphocytes are derived from hematopoietic stem cells. From a precursor are derived three cell lines: B cells, T cells, and natural killer (NK) cells. These differentiation steps are directed by cytokines and cellular interactions in a very complex pattern. B cells Steps proceeding from pre-B cells through B cells to plasma cells. The cells at each step are identified by two characteristics: the immunoglobulin genes undergo rearrangements that will permit the expression and secretion of immunoglobulins; cell surface markers appear that can be detected by monoclonal antibodies. The final step consists of differentiation into plasma cells, again under external influence of T cells. Plasma cells lose most of the surface markers. Antibody production is shown by an enlarged Golgi apparatus, which displaces the nucleus, and by deep blue cytoplasm because of the mRNA being generated. T cells Cells destined to be T cells acquire an antigen, CD7, which they maintain throughout their development. These cells migrate from the bone marrow to the cortex of the thymus, where they undergo a series of changes orchestrated by the thymic cells and by various cytokines. As cells migrate toward the medulla of the thymus, they acquire both the CD4 and the CD8 surface markers and begin to synthesise the T cell receptor. This receptor, crucial to many T cell functions, is composed of a heterodimer. The components of these complexes belong to the immunoglobulin superfamily. The cells acquire the CD3 complex as well as the CD4 and CD8 molecules. As they proceed through the thymus, most are destroyed by apoptosis or programmed cell death initiated by self-antigens presented to T-cells by the epithelial cells of the thymus; thus, clonal selection occurs that allows only the T cells bearing non-selfrecognizing receptors to survive. As cells mature, they lose either the CD4 or the CD8 surface molecule. CD4+ cells generally serve as helper cells in the immune system, whereas CD8+ cells generally have suppressor functions. 7/12 Seminars for the 5th year summer term Prof. MUDr. Jiří Horák NK cells Some cells do not bear the defining surface molecules of B or T cells and their immunoglobulin and TcR genes do not undergo rearrangement. These cells are able to destroy cells without using immunoglobulin - like molecules -> natural killer cells. They have large size with abundant cytoplasm, which contains large azurophilic granules; they are sometimes called large granular lymphocytes (LGL). They have the CD56 and CD16 antigens. In lymph nodes, the follicles contain mainly polyclonal B cells; T cells are found throughout the remainder of the lymph node. The distribution of the lymphocytes in the spleen is much like that in the lymph node. In the peripheral blood, the majority of lymphocytes are small, resting cells. About 80 to 85% are T cells; 75 to 80% of these are CD4, and the remainder, CD8 cells. The B cells represent 15% of circulating lymphocytes and are also polyclonal. Disorders of the Lymphatic System Infectious disorders Lymphocytes play a major role in response to any infection → an increase in lymphocytes in the peripheral blood in viral diseases (mumps, hepatitis, varicella, and infectious mononucleosis) or in certain bacterial diseases (pertussis, brucellosis, and some forms of syphilis). This response is always polyclonal. Local or general enlargement of the lymph nodes in infection. Neoplastic disorders Chronic lymphocytic leukemia (CLL) is the most common form of leukemia. > 90% occur in patients over 50 years of age. Men develop CLL twice as often as do women. CLL is often found incidentally – leukocytosis composed primarily of small lymphocytes. Dg: > 15,000 lymphocytes/μl in peripheral blood and at least 40% of the cells in the bone marrow being lymphocytes. Lymphadenopathy and/or splenomegaly are common. Poor immunologic competence → hypogammaglobulinemia and increase in infection or the presence of autoimmune phenomena – Coombs 8/12 Seminars for the 5th year summer term Prof. MUDr. Jiří Horák positive AIHA, immune thrombocytopenic purpura or immune granulocytopenia. Pure red cell aplasia is unusual. CLL represents a clonal proliferation, usually of B lymphocytes. CLL from T lymphocytes has a poorer prognosis and skin involvement is often seen. Human T-cell leukemia virus (HTLV)-1 infection a more virulent form of T-cell CLL. It may present with hypercalcemia, lytic bone lesions, and severe debility; treatment is rarely effective. The cause of CLL is not known, no genetic basis has been discovered. Clinical staging for CLL Level of risk stage descriptions low 0 lymphocytosis only in blood and bone marrow intermediate I II lymphocytosis plus enlarged lymph nodes lymphocytosis plus enlarged liver and spleen (+ enlarged nodes) high III lymphocytosis plus anemia (not autoimmune) (+ enlarged nodes, spleen or liver) IV lymphocytosis plus thrombocytopenia (not autoimmune) (+ enlarged nodes, spleen or liver) Th: patients in stages 0, I or II may be observed without treatment until they develop bulky lymph node enlargement, disease symptoms such as fevers, night sweats, malaise, or fatigue; or cytopenia Initial treatment – usually a single alkylating agent (chlorambucil, cyclophosphamide) with the addition of prednisone if symptoms are present or if autoimmune phenomena occur. In more advanced disease fludarabine → may produce complete remission through apoptosis. Radiation therapy may be used for bulky tumor mass, lymph node enlargement, or large splenomegaly. CLL may transform into a clinically more malignant neoplasm with features of high-grade lymphoma (Richter’s syndrome). Increased infections during the evolution of CLL should be treated with antibiotics. Intravenous gammaglobulin is useful. 9/12 Seminars for the 5th year summer term Prof. MUDr. Jiří Horák Hairy Cell Leukemia (leukemic reticuloendotheliosis) ~ 1 / 2% of all leukemias. It usually presents as a slowly developing pancytopenia with splenomegaly. Hairy cells look like lymphocytes with fine cytoplasmic projections. Unlike typical B cells, they are capable of phagocytosis. Splenectomy may be useful. Chemotherapy with standard alkylating agents does not help. Most patients respond to alpha-interferon, 2’deoxycoformycin, or 2-chlorodeoxyadenosine. Granulocyte colonystimulating factor may correct leukopenia. The median survival is 3 – 5 years. Lymphomas The most common clinical presentation is asymptomatic enlarged lymph node in the cervical, axillary or inguinal region. Non-Hodgkin’s Lymphomas monoclonal proliferation of a malignant cell of lymphoid origin, either a T or a B cell. The Epstein-Barr virus has been implicated in African Burkitt’s lymphoma and in lymphomas arising from immunosuppressive therapy after organ transplantation; HIV in AIDS-related lymphomas. Non-Hodgkin’s lymphomas are classified by pathologic subtype, immunophenotype, and clinical stage. Major lymphoma cell types: - small, well differentiated lymphocytes - small lymphocytes with cleaved nuclei (follicular center cells) - large lymphoid cells Non-Hodgkin’s lymphomas often present with advanced-stage disease and may occur in extranodal sites (GIT, CNS, bone marrow) True stage I or II are unusual; may be treated with local radiation therapy. Patients with stage III and IV disease are usually treated with chemotherapy. In low-grade lymphoma, a single alkylating agent (chlorambucil, cyclophosphamide) may control the disease. Corticosteroids are often added. Vincristine and doxirubicine may be used. Bone marrow transplantation and peripheral stem cells offer the possibility of curing non-Hodgkin’s lymphomas. 10/12 Seminars for the 5th year summer term Prof. MUDr. Jiří Horák Hodgkin’s disease Bimodal distribution - young adults and ~ 60 years Usual presentation: asymptomatic lymph node enlargement “B” symptoms: fever, night sweats, weight loss > 10% Subtypes of Hodgkin’s disease subtype rel. frequency description prognosis lymphocyte 5 – 15% few RS cells favorable often in young; responds to mediastinal radiation often in elderly; many RS cells less sensitive to radiation abundant RS less favorable predominance nodular sclerosis 40 – 75% mixed cellularity 20 – 40% lymphocyte 5 – 15% depletion cells Dg: Reed-Sternberg cells Staging criteria for Hodgkin’s disease stage Ann Arbor criteria I single lymph node region (LNR) or a single extralymphatic site (ELS) II two or more LNRs on the same side of the diaphragm or a solitary ELS and one or more LNRs on the same side of the diaphragm III LNR on both sides of the diaphragm; with spleen involvement or solitary involvement of an ELS or both IV diffuse involvement of the ELSs with or without lymph node enlargement presence of constitutional symptoms = B, absence = A Staging: CAT scan, lymphangiogram, staging laparotomy 11/12 Seminars for the 5th year summer term Prof. MUDr. Jiří Horák Th: depend on stage, bulk of disease, and the presence or absence of symptoms. Radiation therapy alone is recommended in stage I – IIA; II B – IIIA – chemotherapy + radiation; IIIB + IV – chemotherapy MOPP: nitrogen mustard + vincristine + procarbazine + prednisone Prognosis: stage IA and IIA – 5-year survival > 90% IIIA IIIB and IV 5-year survival > 80% 5-year survival > 50% Th of relapses: combination chemotherapy or bone marrow transplantation ------------------ 12/12