Manejo Actual De Las Hemorroides
advertisement

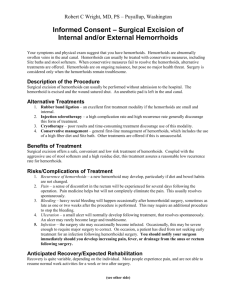
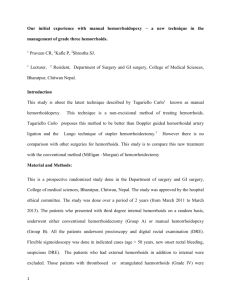
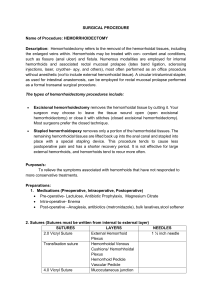
MANEJO ACTUAL DE LAS HEMORROIDES Dr. Stanley Goldberg INTRODUCTION Hemorrhoid disease afflicts over one million Americans per year. Problems with hemorrhoids manifest in several ways, including isolated external disease with thrombosis, mixed internal and external hemorrhoid disease, and primary internal hemorrhoidal disease are common and present with either prolapse, bleeding, or thrombosis. GRADE AND TREATMENTS The severity of the rectal mucosal prolapse in internal hemorrhoidal disease varies from Grade I, with minimal redundant mucosa and no prolapse, to Grades II and III, with increasing degrees of either spontaneously or manually reducible hemorrhoidal mucosa, up to Grade IV, where there is complete prolapse of the hemorrhoidal mucosa that cannot be reduced back into the anal canal. For most patients with symptomatic Grade I disease, we recommend conservative therapy with a combination of supplementary dietary fiber and counseling on bathroom habits. For patients with symptomatic Grade II disease or minimal Grade III disease, we recommend an office procedure such as rubber band ligation to fix the redundant prolapsing mucosa to the underlying muscle. For advanced symptomatic Grade IV disease, we recommend surgery. Approximately 25% of patients who undergo surgery present with acute symptoms and have to be brought to the operating room on an emergency basis. This group includes postpartum patients. We recommend urgent surgery for acute symptoms in postpartum patients if they have had a previous history of symptomatic hemorrhoids. In a recent five-year review of the University of Minnesota experience, with over 20,000 patients who presented with symptomatic hemorrhoids, we found that only 9% of patients required surgery. Conservative therapy was given to 45% of patients, while 46% had an office-based fixation procedure such as rubber band ligation. SURGICAL TECHNIQUE For surgery, we used a variety of anesthetics from general endorectal anesthesia to local anesthesia with intravenous sedation. We prep the patient with two Fleet enemas about 1-2 hours before surgery. We place the patient in the prone position. The incision is started caudal to the dentate line in order to remove present or potential skin tags, then carried cephalad removing only a small wedge of anoderm. The mucosa is undermined and all hemorrhoid tissue is removed down to the internal sphincter muscle. Hemostasis is insured with the cautery. We have found that about 20% of patients will have an associated fissure, especially those with Grade II disease. We perform a partial lateral internal sphincterotomy in these patients and in other patients who have evidence of fibrosis and scarring of the distal internal sphincter muscle. We approximate the mucosal edges with a chromic stitch and often reinforce the proximal dissection with a figure-eight “crown” stitch of 2-0 vicryl. We do not use any packing. We continue to use this standard closed hemorrhoidectomy technique and have not been impressed enough with new techniques, such as laser hemorrhoidectomy, to change our practice. COMPLICATIONS AND LENGTH OF STAY Our complications include a 10-20% urinary retention rate, and a 2% incidence of delayed hemorrhage. Abscessses or cellulitis infections are extremely rare. Our overall length of stay in hospital averages 2.5 days, and has decreased over the past decade from an average of 4 days. EXTERNAL HEMORRHOIDS For isolated external hemorrhoid thrombosis, we recommend early excision of the thrombosed hemorrhoid, not incision. We have had excellent results with this procedure because it immediately relieves the pain of thrombosis and prevents recurrence. CONCLUSION Most cases of symptomatic hemorrhoids can be managed without surgery. For internal or mixed hemorrhoid disease, we recommend a closed technique if surgery is needed. Even though we are limiting surgery to only those patients with the most severe disease, the length of stay for operative therapy is decreasing. We predict that in the future, the incidence of office-based procedures such as rubber band ligation or infrared coagulation will increase, with a decrease In the incidence of operative therapy for symptomatic hemorrhoids.