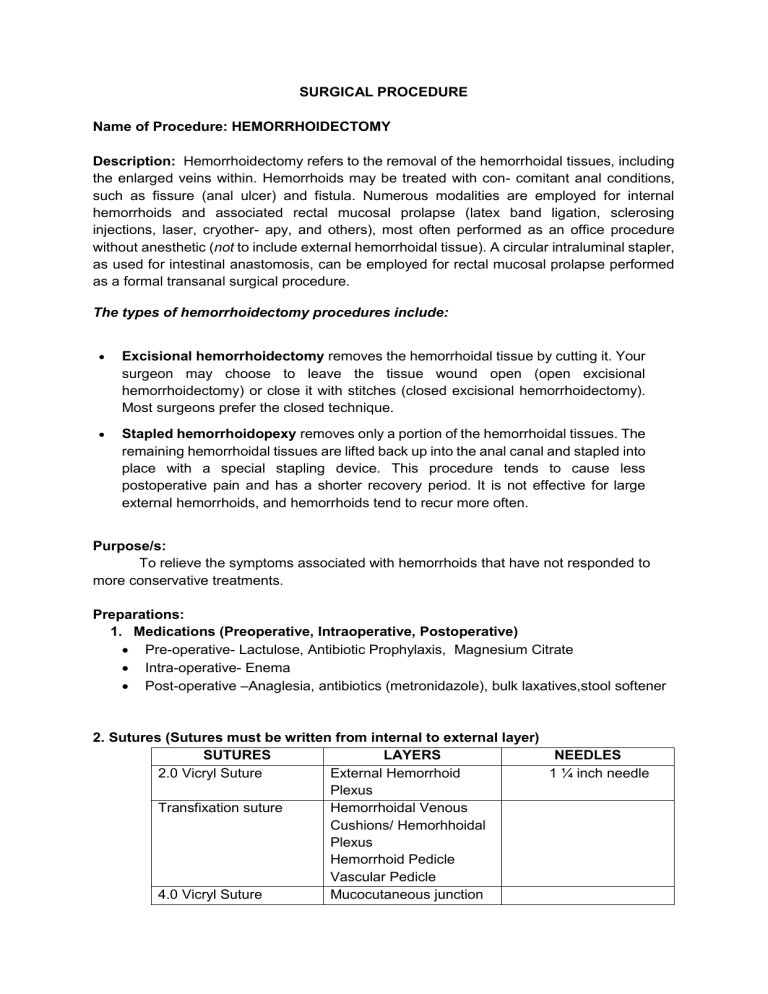
SURGICAL PROCEDURE Name of Procedure: HEMORRHOIDECTOMY Description: Hemorrhoidectomy refers to the removal of the hemorrhoidal tissues, including the enlarged veins within. Hemorrhoids may be treated with con- comitant anal conditions, such as fissure (anal ulcer) and fistula. Numerous modalities are employed for internal hemorrhoids and associated rectal mucosal prolapse (latex band ligation, sclerosing injections, laser, cryother- apy, and others), most often performed as an office procedure without anesthetic (not to include external hemorrhoidal tissue). A circular intraluminal stapler, as used for intestinal anastomosis, can be employed for rectal mucosal prolapse performed as a formal transanal surgical procedure. The types of hemorrhoidectomy procedures include: Excisional hemorrhoidectomy removes the hemorrhoidal tissue by cutting it. Your surgeon may choose to leave the tissue wound open (open excisional hemorrhoidectomy) or close it with stitches (closed excisional hemorrhoidectomy). Most surgeons prefer the closed technique. Stapled hemorrhoidopexy removes only a portion of the hemorrhoidal tissues. The remaining hemorrhoidal tissues are lifted back up into the anal canal and stapled into place with a special stapling device. This procedure tends to cause less postoperative pain and has a shorter recovery period. It is not effective for large external hemorrhoids, and hemorrhoids tend to recur more often. Purpose/s: To relieve the symptoms associated with hemorrhoids that have not responded to more conservative treatments. Preparations: 1. Medications (Preoperative, Intraoperative, Postoperative) Pre-operative- Lactulose, Antibiotic Prophylaxis, Magnesium Citrate Intra-operative- Enema Post-operative –Anaglesia, antibiotics (metronidazole), bulk laxatives,stool softener 2. Sutures (Sutures must be written from internal to external layer) SUTURES LAYERS NEEDLES 2.0 Vicryl Suture External Hemorrhoid 1 ¼ inch needle Plexus Transfixation suture Hemorrhoidal Venous Cushions/ Hemorhhoidal Plexus Hemorrhoid Pedicle Vascular Pedicle 4.0 Vicryl Suture Mucocutaneous junction Mucosa Submucosa 3. Instruments and paraphernalia INSTRUMENTS Retractors PARAPHERNALIA Volkman Retractor 4 Prongs Sharp Anascopes, Speculum, and Probes Hirschman Anascopes Large, Hirschman Anascopes Medium, Hirschman Anascopes Small, Sims Straight Speculum Fenestrated Blades With Set Screw 6", Pratt Crypt Hooks Narrow 8 1/2", Pratt Straight Probe 11", Forceps Haemostatic Forceps, Allis Tissue Forceps 4x5 Teeth 6", Foerster Sponge Forceps Straight 9 1/2" Serrated Jaws, Halstead Mosquito Forceps Straight 5", Thumb Tissue Forceps 1x2 Teeth 5 1/2 " Dressing Forceps 5 1/2" Serrated, Yeoman Biopsy Forceps 4x8mm Bite Complete Ring Handle 14", Allis Tissue Forceps 5x6 Teeth 7 1/2", Pennington Tissue Grasping Forceps 5 1/4", Rochester Pean Forceps Curved 6 1/4", Crile Rankin Hemostatic Forceps Straight 6 1/4", Dressing Forceps 6" Serrated, cautery, laser, or cold instruments Knife, Blades Electrocautery (Cuatery Pencil),Laser Scalpel, Knife Handle No 3, No. 15 or No. 10 scalpel blade and blade handle Other Surgical Accessories Gloves, Stirrups or pillow and roll for positioning, ESU, Buie Suction Tube With Finger Valve 15 Fr, Backhaus Towel Clamp, Minor Basin Set, Lubricants, Surgical scissors Blunt nosed scissors, Metzenbaum Scissors Curved 5 1/2" - Tungsten Carbide, Operating Scissors Sharp Blunt Straight 5 1/2", Mayo Scissors Tungsten Carbide Curved 6 3/4", Mayo Scissors Tungsten Carbide Straight 6 3/4", Mayo Scissors Tungsten Carbide Curved 5 1/2" Wound closure instruments Allis clamps,clips and clamps, needles, needle holder, circular stapling device, surgical adhesives, 4x4 gauze, PPE, Sterilization trays, disinfectants, autoclaves, dry sterilizers Infection Control Products Medicated bandage Anesthesia (types and agents used) General anesthesia is a combination of intravenous (IV) medications and gases that put you in a deep sleep. You are unaware of the procedure and will not feel any pain. You may also receive a peripheral nerve block infusion in addition to general anesthesia. A peripheral nerve block infusion is an injection or continuous drip of liquid anesthetic. The anesthetic flows through a tiny tube inserted near your surgical site to control pain during and after surgery. Regional anesthesia is also known as a nerve block. It involves injecting an anesthetic around certain nerves to numb a large area of the body. You will likely have sedation with regional anesthesia to keep you relaxed and comfortable. Position during Surgery: Prone Jackknife. Folded towels and a laparotomy sheet. Tapes are attached to table sides. Lithotomy. Drape sheet under buttocks, leggings, folded towels, drape sheet over abdomen. Tapes are attached to stirrups. Modified Lateral/Sims. Folded towels and a laparotomy sheet. Tapes are attached to table sides. Preoperative Nursing Goal and Interventions Preoperative Care a. Psychological Care Teach your patient to do the following: o Think positively o Practice relaxation exercises Perform deep-breathing exercises Use visualization and imaging techniques o o Learn about managing pain after surgery Share questions and concerns with doctor b. Health Instructions Stick to healthy foods. Your body needs good nutrition to fight infection and heal following surgery. This is NOT a time for dieting. Avoid dehydration. Drink at least six 8-ounce glasses of fluid per day, preferably water. Practice the post-operative exercises your doctor recommends. The patient will need to do them during and after your hospital stay. c. Physical preparation c.1. Diet Let the patient eat and drink healthily, such as eating fruit, vegetables and protein. But if lost weight or are underweight, have regular high energy/protein snacks. If the patient is a smoker and/or drinks alcohol above the recommended guidelines (14 units a week), try to cut down and stop if possible. Eat a light breakfast and lunch. Avoid greasy foods and red meat. Increase patient’s fiber intake c.2. GIT preparation Patients should not eat or drink anything for 8-12 hours before the surgery. This includes chewing gum. Fasting is necessary before surgery to ensure that the bowel prep is not ruined and helps prevent aspiration, nausea, and vomiting. For their last meal before fasting, instruct patients to go easy and not eat a large meal. Instead, have them eat a light meal of soup or salad, which is quicker for the body to digest. If they have been instructed to take their prescription medication before surgery, they may take it with a small sip of water. If a patient is taking prescription medication, have them bring them with them to the hospital. That way, if they were ordered not to take them before the surgery, they may do so afterwards. Empty patient colon with enema or laxatives c.3. Skin preparation (Illustration) c.4. Fluid administration Drink only clear liquids (no pulp, no dairy) after lunch. Do not let the patient drink anything the last 4 hours before surgery. Nursing Diagnosis/es: Pain (acute or chronic) related to rectal swelling and prolapse Constipation related to ignore the urge to defecate during defecation Anxiety related to plan surgery Intraoperative Period Activities and Care (Steps of the Procedure): Steps Rationale The patient is placed in the jackknife prone, Proper positioning allows the surgeon lithotomy, or left lateral decubitus position. accessibility to the surgical site as well as for The perianal skin is visualized by having an anesthetic administration assistant separate the buttocks or by taping the buttocks apart. The anal canal can be visualized using an Ive's anoscope coated with 2 percent lidocaine jelly. The extent of the hemorrhoidal disease should be assessed and coexisting anal pathology excluded before initiating the procedure. Alternately, anoscopy can be performed after anesthetic administration (injection) when the thrombosed hemorrhoids are exquisitely tender The perianal skin and anal canal are Skin prep aids in preventing surgical site cleansed with povidone-iodine solution. The infection by removing debris from, and base of the hemorrhoid is infiltrated with at cleansing the skin, bringing the resident and least 5 mL of 1 percent lidocaine, using a 25- transient microbes to an irreducible gauge, 1¼-inch needle. minimum, and hindering the growth of microbes during surgical procedure. Lidocaine helps in reducing pain or Avoid making multiple needle sticks in the discomfort caused by the anal tissues. hemorrohoidectomy. The puncture sites can bleed after needle removal. Warn the patient about impending needle insertion into the tender tissues. A fusiform (elliptic) excision is made into the Vigorous bleeding may accompany this anal skin overlying the thrombosis. It is incision and can be controlled with direct preferable to make a radial incision pressure or electrocautery if needed. extending out from the anal canal if the entire hemorrhoid plexus is removed; some physicians prefer a circumferential incision that exposes more clots by crossing over more of the hemorrhoidal sinusoids beneath. A clamp can be placed on the fusiform skin island and traction applied to the skin. The entire hemorrhoid is sharply excised with a no. 15 blade or scissors. The entire hemorrhoidal plexus usually can be removed as one piece attached to the fusiform skin island. Avoid cutting into the muscle sphincter below the hemorrhoidal vessels. The clamp can help to reveal the hemorrhoid below. The anal sphincter is a ring of muscle that opens and closes at the bottom of your anus and plays a large role in controlling bowel function. When the muscle is cut or is damaged or weakened it can cause incontinence—accidental loss of stool. Once the hemorrhoidal plexus and clot have been removed, the base of the wound is examined for residual small clots. Additional hemorrhoidal tissue or clots can be sharply excised. Some physicians chose to close the deep wound with subcutaneous, absorbable, buried 4-0 Vicryl sutures to avoid significant postprocedure bleeding. The sutures should be completely subcutaneous and not penetrate external to the anal skin. The residual blood clot impedes blood flow. The wound should be inspected for adequate hemostasis. If epinephrine is used to anesthetize the wound and the wound is unsutured, late bleeding (up to several hours postprocedure) can develop once the effect of the epinephrine wears off. Topical antibiotic ointment is applied to the surgical site, and 1inch of 4 × 4 gauze is applied over the site between the buttocks. The patient can be given additional gauze for use at home. Hemostasis is important to the success of the procedure, as well as to patient outcomes. Wound closure can reduce bleeding and discomfort at the surgical site. Alternatively, some physicians prefer to leave the wound open. The suture ends are not buried in the skin but exposed outside, which can increase the risk of contamination. The role of topical antibiotics is to reduce the microbial contaminant exposure following the surgical procedure. Special Consideration/s: Chances of problems may be higher for: Patient with Myocardial Infarction within recent 6 months Nursing Responsibilities: Before the Procedure/Examination: Assess patient for the presence of hemorrhoids, discomfort or pain associated with hemorrhoids, diet, fluid intake, and presence of constipation. Instruct patient and/or family regarding causes of hemorrhoids, methods of avoiding hemorrhoids, and treatments that can be performed. Instruct patient and/or family regarding all procedures required. Instruct patient and/or family in comfort measures to use with the presence of hemorrhoids. During the Procedure/Examination: Note for the time the surgery and the general anaesthesia started. Ensure the IV fluids given to the patient. After the Procedure/Examination: Monitor the patient closely in the recovery room. IV fluid should be monitored if working well and enough fluids. Give medications as indicated. Provide warm sitz bath as appropriate Cleanse rectal area with mild soap and water or wipes after each stool and provide skin care. Encourage patient to move around to prevent breathing and circulation problems Postoperative Nursing Assessment 1. Immediate Postoperative (Postanesthetic Period) a. Nursing Assessment Assess air exchange status and note patient’s skin color Verify patient identity. The nurse must also know the type of operative procedure performed and the name of the surgeon responsible for the operation. Monitor the patient upon waking up, the patient may feel pain or upset stomach. Give medications as prescribed. Check for the IV fluids if it is working well and have enough fluids. Encouraged to do deep breathing and circulation exercises. b. Nursing Diagnosis Impaired Urinary Elimination related to the fear of postoperative pain Deficient knowledge related to the lack of information about home care Impaired Urinary Elimination related to the fear of postoperative pain Risk for infection related to inadequate primary defenses c. Goal of Care and Nursing Responsibilities Pain is Relieved or Controlled Encourage patient to report pain Encourage patient to assume position of comfort Review factors that aggravate or alleviate pain Provide comfort measures Provide warm sitz bath as appropriate To accurately verbalize understanding of causes of hemorrhoids, methods of preventing the worsening of hemorrhoids, and comfort measures to employ. Teach the importance of a high-fiber diet (20-35 grams/day) and a fluid intake of at least 2-3 L/day (unless this is contraindicated by a renal, hepatic, or cardiac disorder). Instruct patient and/or family regarding causes of hemorrhoids, methods of avoiding hemorrhoids, and treatments that can be performed. Instruct patient and/or family regarding all procedures required. Instruct patient and/or family in comfort measures to use with the presence of hemorrhoids To help the patient to establish and maintain normal bowel habits Encourage daily fluid intake of 2000 to 3000 ml per day, if not contraindicated medically (Suggest drinking warm, stimulating fluids (tea, hot water) to promote soft stool). Encourage increased fibre in diet (raw fruits, fresh vegetables) to improve consistency of stool and facilitate passage; a minimum of 20 gm of natural dietary fibre per day is recommended. Encourage patient to consume prunes, prune juice, cold cereal, and bean products. Encourage physical activity and regular exercise. Maintenance of Circulation Obtain patient’s vital signs as ordered and report any abnormalities. Monitor intake and output closely. Recognize early symptoms of shock or hemorrhage such as cold extremities, decreased urine output – less than 30 ml/hr, slow capillary refill – greater than 3 seconds, dropping blood pressure, narrowing pulse pressure, tachycardia – increased heart rate. 2. Immediate Postoperative Care a. Nursing Responsibilities Maintaining adequate body system functions Restoring body homeostasis. Pain and discomfort alleviation. Preventing postoperative complications. Promoting adequate discharge planning and health teaching. References and Suggested Readings: Agbo SP. Surgical management of hemorrhoids. J Surg Tech Case Rep. 2011;3(2):68-75. doi:10.4103/2006-8808.92797 Goldman, M. A. (2020). Pocket guide to the operating room. Philadelphia, PA: F.A. Davis Company. Goto, S., Hida, K., Furukawa, T. A., & Sakai, Y. (2016). Subcuticular sutures for skin closure in non‐obstetric surgery. The Cochrane Database of Systematic Reviews, 2016(3), CD012124. https://doi.org/10.1002/14651858.CD012124 Hemorrhoids nursing care plan and management BY RNPEDIA. (2017, July 24). Retrieved April 11, 2021, from https://www.rnpedia.com/nursing-notes/medical-surgical-nursingnotes/hemorrhoids/#:~:text=Nursing%20Intervention&text=Provide%20analgesics%2C %20warm%20sitz%20baths,postoperatively%20for%20drainage%20and%20bleeding. Lewis, S. (2020, November 01). Your complete guide to hemorrhoid removal. Retrieved April 11, 2021, from https://www.healthgrades.com/right-care/hemorrhoid-surgery Medical, I. (2018, February 01). Preparing patients for a hemorrhoidectomy. Retrieved April 11, 2021, from https://www.inxmedical.com/blog/preparing-patients-for-ahemorrhoidectomy/#:~:text=Begin%20A%20Bowel%20Prep,reducing%20the%20risk %20of%20infection. Vera, M., By, -, Vera, M., & Matt Vera is a registered nurse with a bachelor of science in nursing since 2009 and is currently working as a full-time writer and editor for Nurseslabs. During his time as a student. (2019, June 01). 3 hemorrhoids nursing care plans. Retrieved April 11, 2021, from https://nurseslabs.com/hemorrhoids-nursing-careplans/ Zuber, T. (2002, April 15). Hemorrhoidectomy for Thrombosed External Hemorrhoids. Retrieved April 11, 2021, from https://www.aafp.org/afp/2002/0415/p1629.html#:~:text=Acutely%20tender%2C%20thr ombosed%20external%20hemorrhoids,hemorrhoidal%20plexus%20in%20one%20pie ce.