How should continuous infusions of PPIs be given for upper
advertisement

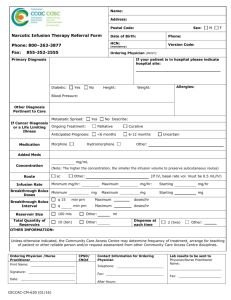
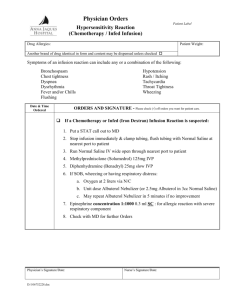
Medicines Q&As Q&A 41.4 How should continuous infusions of proton pump inhibitors be given for acute upper gastrointestinal bleeding? Prepared by UK Medicines Information (UKMi) pharmacists for NHS healthcare professionals Expiry: 30th November 2010 Background Acute upper gastrointestinal bleeding is associated with significant morbidity and mortality. Once the initial episode of bleeding has been controlled usually by endoscopic therapy, the goal is to prevent rebleeding and associated complications. The rebleeding rate after initial endoscopic haemostasis may be as high as 10% to 30% (1). Gastric acid plays a significant part in rebleeding, by impairing haemostasis and causing clot digestion. A low pH will prolong clot formation by prolonging APTT and prothrombin time. Platelet aggregation is nearly completely abolished at a pH of 5.9 or less. Pepsin, which digests clots on the gastric mucosa, is inactivated at pH > 6.0. Therefore suppressing gastric acid production with a target pH of > 6.0 may be beneficial in preventing rebleeding (1). The primary agents used for acid suppression include histamine-2 receptor antagonists (H2RAs) and proton pump inhibitors (PPIs). The degree of acid suppression produced by H2RAs appears to be inadequate to control bleeding or to prevent rebleeding (2,3). This could be due to their failure to raise gastric pH to a level that maintains clot integrity (3), or to the tolerance that develops fairly rapidly to their acid suppressive effects (4). In contrast, PPIs provide more potent and longer lasting acid suppression. They irreversibly inhibit the proton pump, which is the final step in acid secretion (4). Answer Dose A review analysed the results of 16 randomised controlled trials involving a total of over 3800 patients receiving omeprazole infusions for upper gastrointestinal bleeding (2). It revealed that bolus administration plus continuous infusion was more effective than bolus infusion alone in decreasing both rebleeding and the need for surgery. The review further concluded that optimal effect was achieved with an iv bolus of 80mg, followed by continuous infusion of 8mg/hour for 72 hours, after which therapy may be continued with an oral PPI (2). This regimen conforms with current guidance from the British Society of Gastroenterology (5) and a US consensus recommendation (6) and SIGN guidance (7). The consensus document and SIGN guidance suggests that either iv omeprazole or pantoprazole may be given at the same dose. There is very little evidence to support the use of pantoprazole, but nonetheless omeprazole and pantoprazole have similar potency (1). Studies have shown that the regimen of 80mg iv. bolus of pantoprazole or omeprazole followed by immediate continuous infusion of 8mg/hour appears to offer optimal acid suppression (8) with pantoprazole raising intragastric pH to greater than 6.0 for 64%, 84% and 86.5% of the time respectively – see below (9,8,10). This level of acid suppression can be achieved within 20 minutes of administration of an 80mg bolus given over two minutes, but continuous infusion is then required for maintenance of the necessary pH (8). One paper describes two small open-label, single centre pilot studies (n=20 each) in which intragastric pH was measured during continuous infusion with pantoprazole in patients with bleeding peptic ulcer. Following endoscopic haemostasis, all patients received an iv bolus injection of 80mg pantoprazole immediately followed by a continuous infusion of either 6mg/hour or 8mg/hour for 72 hours. The median percentage time that pH 6 during the 0-48 hour interval was 64% for the 8mg/hour group, and 47% for the 6mg/hour group. Compared with the group who received 6mg/hour, the patients who received 8mg/hour pantoprazole showed a lower inter-individual variability of the intragastric pH (9). From the National Electronic Library for Medicines. www.nelm.nhs.uk 1 Medicines Q&As Similar results were seen in a small sub-group (n=15) in a double-blind placebo-controlled study in which the intragastric pH was 6 or more for 86.5% ± 19.8% of the time in patients receiving an iv bolus of 80mg pantoprazole followed by a continuous infusion of 8mg/hour for 72 hours (10). This study also demonstrated that, following successful endoscopic therapy, the use of high dose pantoprazole infusion was significantly more effective than placebo in reducing rebleeding, transfusion requirements and hospital stay (n=203). An intravenous formulation of esomeprazole is also available. The manufacturers have carried out a single-centre, open-label, randomised, five-way cross-over study in 28 healthy subjects to investigate the effect of various doses of intravenous esomeprazole on 24-hour intragastric pH and pharmacokinetics. Each dosage regime was given for a single 24-hour study period with a washout period of at least 13 days between doses. Esomeprazole 80mg (iv bolus infusion over 30 minutes) followed by 8mg/hour iv for the remainder of the 24 hour period provided a greater amount of time with both intragastric pH>4 and pH>6 during the 24-hour period than all other esomeprazole doses except the 120mg (bolus infusion over 2 hours) followed by 8mg/hour regime (11). There is one published randomised company-sponsored placebo-controlled trial for intravenous esomeprazole. After endoscopic haemostasis, placebo or an iv bolus of 80mg esomeprazole followed by an 8mg/hour infusion over 72 hours was administered. After infusion, both groups received oral esomeprazole 40mg daily for 27 days. The primary end point was the rate of clinically significant recurrent peptic ulcer bleeding within 72 hours of endoscopic treatment. There were 375 esomeprazole recipients and 389 placebo recipients, who were all considered high-risk. Fewer patients receiving esomeprazole had recurrent bleeding within 72 hours (22 of 375) than those receiving placebo (40 of 389) [5.9% vs 10.3%; difference, 4.4 percentage points (95% CI, 0.6%-8.3%) p = 0.026]. A post hoc analysis of the study investigated if esomeprazole prevents recurrent peptic ulcer bleeding more effectively than placebo in a multiethnic patient sample. Although 87% of the patients were Caucasian, the authors’ opinion was that efficacy of PPIs is not race-specific (12). Duration Since the half-lives of all the PPIs are short (approximately 40 minutes to 2 hours) (13-16), and proton pumps are continuously being synthesised, a bolus dose is necessary to inactivate existing pumps, followed by a continuous infusion to inactivate newly synthesised pumps. Repeat bolus injections of PPI fail to raise gastric pH consistently above 4.0 (1) and therefore are insufficient to prevent rebleeding. It is unclear how long patients should continue to receive PPI therapy for. In patients with bleeding peptic ulcer, the risk of ulcer rebleeding is highest during the first three days, and most patients rebleed in the first 24 hours (9). The majority of studies have given continuous iv infusions of the PPI for 3 days, followed by oral therapy (17), usually omeprazole 20mg/day until day 21 (1). The exact oral dose and length of treatment may be determined by the individual clinician, on a case by case basis. Further double-blind randomised studies are required to determine the relative efficacy of different PPIs for this indication. Administration The administration details and stability data given below refer to the branded products stated. Omeprazole and pantoprazole are not licensed to be given by continuous infusion (14,15). However, esomeprazole is licensed to be given as a continuous intravenous infusion over a period of 3 days. This is for the prevention of rebleeding, following therapeutic endoscopy for acute bleeding gastric or duodenal ulcers (16). Omeprazole is available as Losec® intravenous infusion and Losec IV injection, both as 40mg vials. The two preparations have different excipients and due to a lack of stability data the injection is not interchangeable with the infusion. After the initial 80mg bolus dose has been given (using the IV injection), one 40mg intravenous infusion vial should be reconstituted with approximately 5ml of sodium chloride 0.9%, immediately diluted to 100ml (14) and then administered at a rate of 8mg/hour, i.e. over 5 hours. This can then be repeated with a new vial each time until the 72 hour period is From the National Electronic Library for Medicines. www.nelm.nhs.uk 2 Medicines Q&As completed. The manufacturer has information to show that the product is chemically and physically stable in sodium chloride 0.9% for 12 hours (14), and a published study shows stability for up to 48 hours (18). Despite this the vial does not contain a preservative and the manufacturer advises from a microbiological point of view that the reconstituted solution should be used within 3 hours (14). However none of the published studies that have utilised the omeprazole infusion regimen make reference to limiting the infusion time to 3 hours. Pantoprazole is available as Protium ® injection in a 40mg vial. Again, an 80mg injection is given initially, followed by a continuous infusion. For infusion each vial should be reconstituted with 10ml sodium chloride 0.9% and then further diluted with 100ml sodium chloride 0.9% or glucose 5%. The SPC states that the reconstituted solution should be used within 12 hours (15), yet a published study again shows chemical stability for up to 48 hours (18). However, note that the SPC also states that, from a microbiological point of view, the reconstituted product should be used immediately. If not, inuse storage times and conditions prior to use are the responsibility of the user (15). In the pilot studies, following the initial bolus dose, three reconstituted vials of 40mg pantoprazole in 30ml sodium chloride 0.9% was infused , protected from direct light, and a fresh solution prepared every 12 hours until the end of the infusion (72 hours) (9). No stability data were given and this concentration of pantoprazole is not licensed by the manufacturer. Esomeprazole is available as Nexium ® IV 40mg powder for solution for injection/infusion. Following therapeutic endoscopy, 80mg should be administered as a bolus infusion over 30 minutes, followed by a continuous intravenous infusion of 8mg/hour given over 71.5 hours (total infusion time including bolus is therefore 72 hours). A solution for infusion of 80mg is prepared by dissolving the contents of two vials of esomeprazole 40mg in up to 100ml of 0.9% sodium chloride for intravenous use. After reconstitution, chemical and physical in-use stability has been demonstrated for 12 hours at 30°C. From a microbiological point of view, the product should be used immediately (16). To date no large-scale head-to-head comparisons of continuous infusions of intravenous PPIs have been performed in patients with peptic ulcer bleeding. Summary For omeprazole, pantoprazole and esomeprazole, limited evidence suggests that optimal effect is achieved with an iv bolus dose of 80mg, followed by continuous infusion of 8mg/hour for 3 days (2,12). After administration of the initial bolus dose, the continuous infusion can be prepared by reconstituting a 40mg vial of either omeprazole (Losec ®) or pantoprazole and further diluting in 100ml of sodium chloride 0.9%. This can be given at a rate of 8mg/hour (i.e. over 5 hours), and repeated with a fresh vial after that time. Depending on the host organisation’s attitude to microbiological stability, infusions could be made up and run over 24-48 hours if necessary since omeprazole (Losec®) and pantoprazole are chemically stable in sodium chloride 0.9% for this period (14,15,18). After administration of the initial bolus infusion of 80mg esomeprazole, the contents of two 40mg vials of esomeprazole are dissolved in up to 100ml of 0.9% sodium chloride and given at a rate of 8mg/hour (i.e. over 5 hours). This is repeated with fresh vials after that time (16). The infusion may be followed by conversion to oral PPI therapy. The exact oral dose and length of treatment may be determined by the individual clinician, on a case by case basis. The use of omeprazole and pantoprazole in the manner described above is unlicensed, and is therefore the responsibility of the prescribing physician. However, esomeprazole has a licence for this method of administration. It is indicated for the prevention of rebleeding, following therapeutic endoscopy for acute bleeding gastric or duodenal ulcers (16). To date no large-scale head-to-head comparisons of continuous infusions of intravenous PPIs have been performed in patients with peptic ulcer bleeding. From the National Electronic Library for Medicines. www.nelm.nhs.uk 3 Medicines Q&As Limitations This Q&A has concentrated on the technical details of how intravenous PPIs are given and not the evidence to support their use for the indications described, nor their safety profiles. The results of studies in this field are complicated by the fact that they look at multiple clinical endpoints, such as recurrence of bleeding, need for blood transfusion or surgery and length of hospital stay, and they do so at varying time intervals. Several recent reviews (17,19,20), meta-analyses and systematic reviews have been published on the use of proton pump inhibitors for acute peptic ulcer bleeding, the most up to date being a Cochrane review, which is a systematic review plus meta-analysis (21). The administration details and stability data included in this Q&A refer to the branded products stated. Disclaimer Medicines Q&As are intended for healthcare professionals and reflect UK practice. Each Q&A relates only to the clinical scenario described. Q&As are believed to accurately reflect the medical literature at the time of writing. See NeLM for full disclaimer. References (1) Hopefl A. Rational Use of Parenteral Proton Pump Inhibitors. Hospital Pharmacy 2001; 36: 344350. (2) Morgan D. Intravenous proton pump inhibitors in the critical care setting. Crit Care Med 2002; 30(6): S369-S372. (3) Lin H-J, Lo W-C, Lee F-Y et al. A prospective randomised comparative trial showing that omeprazole prevents rebleeding in patients with bleeding peptic ulcer after successful endoscopic therapy. Arch Intern Med 1998; 158: 54-58. (4) Pisegna J. Pharmacology of acid suppression in the hospital setting: Focus on proton pump inhibition. Crit Care Med 2002; 30 (6): S356-S361. (5) British Society of Gastroenterology Endoscopy Committee. Non-variceal upper gastrointestinal haemorrhage: guidelines. Gut 2002;51 (Suppl IV):iv1-iv6. (6) Barkun A, Bardou M, Marshall JK. Consensus recommendations for managing patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med 2003;139:843-57. (7) Management of acute upper & lower GI bleeding A National Clinical Guideline. SIGN Guideline 105, September 2008. Accessed on 23rd October 2008 via http://www.sign.ac.uk/pdf/sign105.pdf (8) Brunner G, Luna P, Hartmann M et al. Optimizing the intragastric pH as a supportive therapy in upper GI bleeding. Yale J Biol Med 1996; 69(3): 225-231. (9) Van Rensburg CJ, Hartmann M, Thorpe A et al. Intragastric pH during continuous infusion with pantoprazole in patients with bleeding peptic ulcer. Am J Gastroenterol 2003;98:2635-2641. (10) Zargar SA, Javid G, Khan BA et al. Pantoprazole infusion as adjuvant therapy to endoscopic treatment in patients with peptic ulcer bleeding: Prospective randomised controlled trial. J Gastroenterol and Hepatol 2006;21:716-721. (11) Astra Zeneca Data on File – personal communication 5th November 2008 (12) Sung JJY, Barkun A, Kuipers EJ et al. Intravenous esomeprazole for prevention of recurrent peptic ulcer bleed. Annals of Internal Medicine 2009; 150:455-64. Accessed via www.annals.org/ on 3rd June 2009. (13) Therapeutic Drugs, edited by Colin Dollery. 2nd Edition, 1999. Churchill Livingstone. (14) Summary of Product Characteristics for Losec Infusion (omeprazole), Astra Zeneca. Accessed via http://www.emc.medicines.org.uk/ on 29th October, 2008 [date of revision of text 28th January 2008]. (15) Summary of Product Characteristics for Protium 40mg IV Powder for solution for injection (pantoprazole), Nycomed UK Ltd. Accessed via http://www.emc.medicines.org.uk/ on 29th October, 2008 [date of revision of text January 2008]. (16) Summary of Product Characteristics for Nexium IV 40mg Powder for Solution for injection/infusion (esomeprazole), Astra Zeneca. Accessed on 3rd June 2009 [date of revision of text 21st May From the National Electronic Library for Medicines. www.nelm.nhs.uk 4 Medicines Q&As 2009] via http://emc.medicines.org.uk/medicine/14054/SPC/Nexium I.V. 40mg Powder for solution for injection/infusion/ (17) Armstrong D, Intravenous proton pump inhibitor therapy: a rationale for use. Reviews in Gastroenterological Disorders 2005; 5(suppl 2); S18-S30. (18) Carpenter JF, McNulty MA, Dusci LJ et al. Stability of omeprazole sodium and pantoprazole sodium diluted for intravenous infusion. J Pharm Technol 2006; 22: 95-98. (19) Gralnek IM, Barkun AN, Bardou M. Current concepts: Management of acute bleeding from a peptic ulcer. N Engl J Med 2008; 359 (9): 928-937 (20) Kovacs TOG, Jensen DM. The short-term medical management of non-variceal upper gastrointestinal bleeding. Drugs 2008; 68 (15): 2105-2111. (21) Leontiadis GI, Sharma VK, Howden CW. Proton pump inhibitor treatment for acute peptic ulcer bleeding. Cochrane Database of Systematic Reviews 2006, Issue 1. Art No:CD002094. DOI:10.1002/14651858.CD002094.pub3. Date of most recent amendment Nov 2005. Quality Assurance Prepared by Sandra Hicks (based on earlier work by Kate Pickett), Wessex Drug and Medicines Information Centre, Southampton University Hospitals Trust. Partial revision by Sandra Hicks on 8 th July 2009. Date Prepared 30th October 2008. Checked by Kate Pickett, Medicines Q&A Pharmacist, Wessex Drug and Medicines Information Centre, Southampton University Hospitals Trust. Date of check 14th January 2009. Partial revision checked 15th July 2009 Search strategy Embase via NLH Search 2.0 (search strategy: [exp continuous infusion + exp proton pump inhibitor] limit to: Human and English Language Medline via NLH Search 2.0 (search strategy: [exp infusions, parenteral] OR [exp infusions, intravenous] + [exp omeprazole OR esomeprazole.af OR esomeprazole.af] Limit to: Publication year from 2000 and Human and English Language) Manufacturer - AstraZeneca contacted via email on 4th November 2008. Losec (omeprazole) and Protium (pantoprazole) SPCs via Electronic Medicines Compendium http://emc.medicines.org.uk accessed 29th October 2008. Nexium (esomeprazole) SPC via Electronic Medicines Compendium http://emc.medicines.org.uk accessed on 29th October 2008 and 3rd June 2009. Micromedex. Cochrane Library. NeLH Guidelines finder. From the National Electronic Library for Medicines. www.nelm.nhs.uk 5