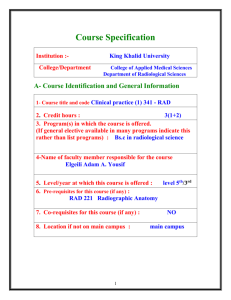
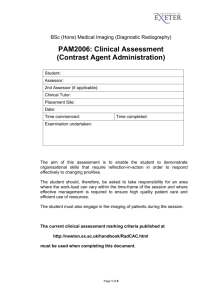
BSc (Hons) Medical Imaging (Diagnostic Radiography) PAM2006
advertisement

BSc (Hons) Medical Imaging (Diagnostic Radiography) PAM2006: Clinical Assessment (Facial Bones, Skull) Student: Assessor: 2nd Assessor (if applicable): Clinical Tutor: Placement Site: Date: Time commenced: Time completed: Examination undertaken: Projections undertaken: 1. 2. 3. As facial bones / skull series (not intra-orbital foreign body examinations) can be infrequent at certain sites, it may be necessary to permit the student to undertake a simulated assessment i.e. by positioning a member of staff and irradiating a skull phantom. The student should analyse the phantom images whilst anonymous patient images should be used for the radiographic awareness section. This option should only be selected after discussion with the Placement Coordinator, and should be limited to either a skull or facial bones series (not IOFB). A skull phantom can be borrowed from the School of Physics, University of Exeter. The current clinical assessment marking criteria published at http://newton.ex.ac.uk/handbook/RadCAC.html must be used when completing this document. Page 1 of 10 The student is expected to provide a verbal commentary throughout the assessment to demonstrate understanding of, and compliance with, safe and proficient practice. Section 1. Exam Preparation Undertaken? Tasks Prompt No Yes THE IMAGING REQUEST Check for Referrer’s signature and date Stop Explain the medical terminology and justify examination under IR(ME)R Stop Discuss correctly the need for a pregnancy check Stop Describe which projections are to be undertaken Stop Consider previous images / reports, whether a duplicate request etc Stop ROOM PREPARATION AND INFECTION CONTROL Tidy the room in line with departmental protocols Clean the room in line with departmental infection control protocols Prepare equipment and accessories Set provisional exposure factors, and explain rationale for choice of exposure factors PATIENT PREPARATION Greet the patient Obtain a positive identification Stop Check for pregnancy (as appropriate) Stop / N/A Correct patient preparation Check area of interest with patient Stop Provide a clear explanation of procedure Gain informed consent prior to undertaking the examination Stop Mark for Section 1: Maximum mark = 10 Page 2 of 10 Section 2: Radiographic Technique (initial projections, not repeats) Projection 1 Tasks No Patient positioning, including ensuring stability, comfort and immobility Stop Positioning of image receptor (use of associated equipment e.g. bucky, cassette stand etc) Stop Handling of tube – centring and angling of beam Stop Collimation (including proficiency & appropriateness) Stop Correct anatomical marker(s) placed in an appropriate place on the image receptor Stop Confirm or modify provisional exposure Stop Communication with the patient throughout (including breathing instructions as appropriate) Stop Radiation protection of self and staff (as appropriate) Stop Section 2: Radiographic Technique (initial projections, not repeats) Prompt Yes Prompt Yes Projection 2 Tasks No Patient positioning, including ensuring stability, comfort and immobility Stop Positioning of image receptor (use of associated equipment e.g. bucky, cassette stand etc) Stop Handling of tube – centring and angling of beam Stop Collimation (including proficiency & appropriateness) Stop Correct anatomical marker(s) placed in an appropriate place on the image receptor Stop Confirm or modify provisional exposure Stop Communication with the patient throughout (including breathing instructions as appropriate) Stop Radiation protection of self and staff (as appropriate) Stop Page 3 of 10 Section 2: Radiographic Technique (initial projections, not repeats) Projection 3 Tasks No Patient positioning, including ensuring stability, comfort and immobility Stop Positioning of image receptor (use of associated equipment e.g. bucky, cassette stand etc) Stop Handling of tube – centring and angling of beam Stop Collimation (including proficiency & appropriateness) Stop Correct anatomical marker(s) placed in an appropriate place on the image receptor Stop Confirm or modify provisional exposure Stop Communication with the patient throughout (including breathing instructions as appropriate) Stop Radiation protection of self and staff (as appropriate) Stop Section 2: Radiographic Technique (initial projections, not repeats) Prompt Yes Prompt Yes Projection 4 Tasks No Patient positioning, including ensuring stability, comfort and immobility Stop Positioning of image receptor (use of associated equipment e.g. bucky, cassette stand etc) Stop Handling of tube – centring and angling of beam Stop Collimation (including proficiency & appropriateness) Stop Correct anatomical marker(s) placed in an appropriate place on the image receptor Stop Confirm or modify provisional exposure Stop Communication with the patient throughout (including breathing instructions as appropriate) Stop Radiation protection of self and staff (as appropriate) Stop Page 4 of 10 Section 2: Radiographic Technique (initial projections, not repeats) All Initial Projections Total Mark Awarded for Section 2: Maximum mark = 10 Section 3. Exam Completion Undertaken? Tasks No Prompt Yes PATIENT AFTERCARE AND RECORD KEEPING Appropriate patient care provided during the checking of the images Appropriate aftercare provided Correct information given (e.g. regarding results etc) Tidy room ready for next patient in line with departmental protocol Clean room ready for next patient in line with departmental infection control protocols Dose Area Product reading / exposure factors recorded Stop All radiology records / archiving / paper work completed Stop Mark for Section 3: Maximum mark = 10 Page 5 of 10 Section 4. Radiographic Awareness Undertaken? Tasks No Check for correct identification information (patient name, date) Prompt Yes Stop Ensure that correct anatomical marker(s) are clearly visible on final image (either primary or added) before archiving Stop Correct identification of all bones Correct identification of bony landmarks / features on bones Correct identification of all visible joints Correct identification of all visible soft tissue anatomy/associated structures Correctly evaluate whether or not the required anatomical features are included on the image Correctly evaluate the patient position, including suggestions for how positioning could be improved (if appropriate) Correctly discuss the exposure factors, including evaluation of under- or overexposure on digital systems (e.g. ‘s-factor’) Correct assessment of image sharpness (including all three causes of image unsharpness) Correct assessment of collimation including impact upon image quality & patient dose Correct assessment of artefacts (including identification of avoidable & unavoidable artefacts) Description of any abnormalities seen using appropriate medical terminology Correct assessment of overall diagnostic quality including identification of the need to repeat or undertake further projections Mark for Section 4: Maximum mark = 10 Page 6 of 10 Section 5. Assessor Evaluation of Conduct Undertaken? Required prompting Tasks Intermittently throughout the assessment Consistently throughout the assessment PATIENT CARE AND PROFESSIONAL CONDUCT Did the student act in the patient’s best interests throughout the examination? Did the student respect the confidentiality and dignity of the patient at all times? Did the student maintain proper and effective communication with the patient throughout the examination? Did the student keep accurate patient records? Did the student deal fairly and safely with the risks of infection? Did the student carry out their duties in a professional and ethical way? Was the student’s conduct throughout the entire examination such that they gained the confidence of the patient? Mark for Section 5: Maximum mark = 10 Page 7 of 10 In your opinion, did the student produce images which were: Unacceptable / Diagnostically Acceptable / Optimal ? (please circle as appropriate) Please comment upon two or more aspects where you have indicated on the assessment form that the student could improve for future practice: 1. 2. Please comment upon two or more aspects where you have indicated on the assessment form that the student has demonstrated a strength or strengths during the assessment: 1. 2. Page 8 of 10 Marking Summary Marks according to criteria Section 1: Exam Preparation Maximum 10 marks Section 2: Radiographic Technique Maximum 10 marks Section 3: Exam Completion Maximum 10 marks Section 4: Radiographic Awareness Maximum 10 marks Section 5: Assessor Evaluation of Conduct Maximum 10 marks Total Marks Overall Total Marks (maximum 50 marks) (Pass mark = 20 marks) Percentage: Clinical Assessor’s Signature: Date Clinical Assessor discussed feedback with Student: Page 9 of 10 Student’s Reflective Comments: Did any of the assessor’s comments surprise you? Where you expecting any of these comments? How will you use these comments to develop your practical radiographic ability? What did you gain from this experience? What did you do well? What could you have done better? How will your future practice change as a result of this assessment? Students signature: Date: Page 10 of 10