Overviewcriticalcare_updatemarch 2009
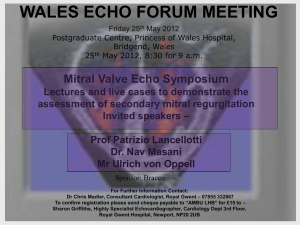
advertisement

National Public Health Service for Wales Critical care public health tool –updated overview of evidence base Critical care public health tool – overview of evidence base Author: Dr Nina Williams, Consultant in Public Health Date: May 2009 Version: 1 Status: Final Intended Audience: Public (Internet) / NHS Wales (Intranet) / NPHS (Intranet) / Critical Care Networks Purpose and Summary of Document: This tool draws together updated evidence upon critical care. It is formatted to assist the critical care networks in identifying current best evidence and to provide summaries of key messages. Publication/Distribution: Publication in NPHS Document Database HSCQ Team Link from NPHS e-Bulletin Link from Stakeholder e-Newsletter Inform networks directly Author: Dr Nina Williams, Consultant in Public Health Version: 1. Published May 2009 Review Date March 2010 Date: 310509 Status: Final Page: 1 of 7 Intended Audience: Public (Internet) / NHS Wales (Intranet) / NPHS (Intranet) / Critical Care Networks Critical care public health tool – updated overview of evidence base National Public Health Service for Wales Critical care public health tool - overview of the evidence base for best practice in critical care This is one of series of regular evidence updates, which are undertaken by LKMS as part of NPHS support to the All Wales Critical Care Advisory Group. The aim is to “research and identify the evidence base for the best practice and new technology for the management of critically ill patients based on a strong national and international evidence base.” 1 A systematic search methodology is followed so the results are easily updated and reproducible. Details of full methodology, search results and literature review are available from LKMS.2 The initial searches identified very few papers of high quality evidence (systematic reviews, RCTs and meta-analyses). Most are single centre primary research studies. The focus is on outcomes in terms of ICU quality measures like average length of stay, ICU mortality, patient/family satisfaction, sub optimal pain management, effectiveness and cost effectiveness, care bundle compliance e.g. prevention of ventilator associated pneumonia, rate of infections related to instrumentation. Intervention Reference National Institute for Health and Clinical Excellence. Rehabilitation after critical illness. London: NICE; 2009 Available at: http://www.nice.org.uk/guidance/CG83 Welsh Assembly Government. Designed for Life: Welsh guidelines for the transfer of the critically ill adult. Cardiff: WAG; 2009 Comment Issued with EH/ML/0010/09. Available at: http://howis.wales.nhs.uk/doclib/EHML-010-09-new.pdf 1 2 Designed for Life: Quality requirements for adult critical care in Wales. EH/ML/008/08 LKMS, National Public Health Service for Wales, NPHS, 36, Orchard St, Swansea. 01792 607331 Email : LKMS Author: Dr Nina Williams, Consultant in Public Health Version: 1. Published May 2009 Review Date March 2010 Date: 310509 Page: 2 of 7 Status: Final Intended Audience: Public (Internet) / NHS Wales (Intranet) / NPHS (Intranet) / Critical Care Networks Critical care public health tool – updated overview of evidence base National Public Health Service for Wales Intervention Care bundles, quality measures Reference Comment See Summary of main findings from the Critical care literature provided for Critical Care Advisory Group Type III evidence Weaning NHS Modernisation Agency Critical care programme. Weaning and long term ventilation. Leicester: NHS Modernisation Agency; 2002. Type III evidence Author: Dr Nina Williams, Consultant in Public Health Version: 1. Published May 2009 Review Date March 2010 Date: 310509 Page: 3 of 7 From Institute for Healthcare Improvement, ventilator and sepsis care bundles describe a collection of evidence based elements put together to improve clinical outcomes and both these bundles were associated with improvement in mortality. The bundles themselves have not undergone RCTs. A systematic review of interventions that improved patient outcomes identified quality measures that could be applied to improve ICU care. Non-invasive ventilation (NIV) reduces the need for intubation, duration of ventilation and mortality in patients with acute exacerbation of COPD. May lead to reduction in ICU admissions. NIV reduces complication rates e.g. reduces infection as a consequence of intubation The number of patients needing prolonged mechanical ventilation and their outcomes can be improved by specific approaches to weaning and the use of weaning protocols. It is estimated that a 50% cost saving per patient day could be made in the UK by caring for chronically ventilated patients at level 2 setting rather than at level 3. Status: Final Intended Audience: Public (Internet) / NHS Wales (Intranet) / NPHS (Intranet) / Critical Care Networks Critical care public health tool – updated overview of evidence base National Public Health Service for Wales Intervention Reference Comment A specialist non-invasive ventilation service is recommended provided by specialist units experienced in the provision of long term and domiciliary ventilatory support. Zilberberg MD et al. Anemia, transfusions and hospital outcomes among critically ill patients on prolonged acute mechanical ventilation: a retrospective cohort study. Critical Care 2008; 12(2):R60, Patients receiving prolonged acute mechanical ventilation (PAMV) are at high likelihood of being transfused with multiple units of blood at relatively high hemoglobin levels. Transfusions independently contribute to increased risk for hospital death, length of stay, and costs. Reducing exposure of PAMV patients to blood may represent an attractive target for efforts to improve quality and efficiency of health care delivery in this population Type IV evidence Patient safety National Public Health Service for Wales. An NPHS review to inform the patient safety initiative in Wales. Cardiff: NPHS; 2007. Author: Dr Nina Williams, Consultant in Public Health Version: 1. Published May 2009 Review Date March 2010 Date: 310509 Page: 4 of 7 updated the evidence base on the Institute of Healthcare Improvement Initiatives http://www.ihi.org/IHI/Topics/CriticalCare / Status: Final Intended Audience: Public (Internet) / NHS Wales (Intranet) / NPHS (Intranet) / Critical Care Networks Critical care public health tool – updated overview of evidence base National Public Health Service for Wales Intervention Reference Type III evidence Comment and recommended 4 for prioritisation which have relevance to critical care: National Institute for Health and Clinical Excellence. Acutely ill patients in hospital. CG50. London: NICE; 2007 Delivering reliable evidence based care for chronic heart failure Reducing health infections Preventing and complications Preventing medicines harm care associated reducing from surgical high risk In addition, physiological track and trigger systems were recommended by NICE in 2007 to monitor all adult patient patients in acute hospital settings. Type II evidence Prevention of ventilator-associated pneumonia National Institute for Health and Clinical Excellence. Technical patient safety solutions for prevention of ventilator-associated pneumonia in adults. London: NICE; 2008. Author: Dr Nina Williams, Consultant in Public Health Version: 1. Published May 2009 Review Date March 2010 Date: 310509 Page: 5 of 7 On the basis of low potential for harm and supported by credible efficacy data and expert advice, the following actions were considered to be relatively easy to implement and associated with little or no Status: Final Intended Audience: Public (Internet) / NHS Wales (Intranet) / NPHS (Intranet) / Critical Care Networks Critical care public health tool – updated overview of evidence base National Public Health Service for Wales Intervention Reference Type II evidence Comment additional resource: Mechanically ventilated patients who are intubated should be positioned with their upper body elevated (in a semi-recumbent or seated position) for as much of the time as possible. For some patients this will not be appropriate (for example, those with spinal injuries). Oral antiseptics (for example, chlorhexidine) should be included as part of the oral hygiene regimen for all patients who are intubated and receiving mechanical ventilation. The Committee examined evidence which suggested that selective decontamination of the digestive tract (SDD) using topical antibiotics may reduce the incidence of VAP and that SDD regimes that include systemic antibiotics may also reduce mortality. However Specialist Advisers stated that UK intensive care specialists had particular concerns about the risk of infection with Clostridium difficile and the induction and/or selection of resistant, including multiresistant, microorganisms as a result of SDD. Therefore the Committee recommended further research into SDD in a UK Author: Dr Nina Williams, Consultant in Public Health Version: 1. Published May 2009 Review Date March 2010 Date: 310509 Page: 6 of 7 Status: Final Intended Audience: Public (Internet) / NHS Wales (Intranet) / NPHS (Intranet) / Critical Care Networks Critical care public health tool – updated overview of evidence base National Public Health Service for Wales Intervention Reference Comment setting. National Institute for Health and Clinical Excellence. Technical patient safety solutions for prevention of ventilatorassociated pneumonia in adults. PSG002. London: NICE; 2008 Although the evidence supported the use of elements of care bundles, there was insufficient evidence to recommend a care bundle of any specific design. Type II evidence Critical care services Wunsch H et al. Variation in critical care services across North America and Western Europe. Critical Care Medicine 2008;36(10):2787-93, e1-9, Type IV evidence Author: Dr Nina Williams, Consultant in Public Health Version: 1. Published May 2009 Review Date March 2010 Date: 310509 Page: 7 of 7 The number of intensive care unit beds per capita is not strongly correlated with overall health expenditure, but does correlate strongly with mortality (the UK did not compare favourably to Germany based on a one year snapshot). These findings demonstrate the need for critical care data from all countries, as they are essential for interpretation of studies, and policy decisions regarding critical care services. Status: Final Intended Audience: Public (Internet) / NHS Wales (Intranet) / NPHS (Intranet) / Critical Care Networks