Propofol
advertisement

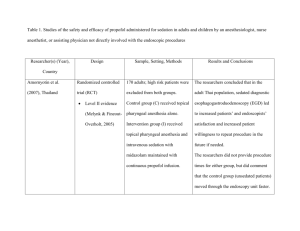
Print Propofol Diprivan® Propofol Emulsion for Injection(Inj 10 mg/ml) [1 of 1 - Click here to see more photos] [ Patient Education ] [ Indications/Dosage ] [ Administration ] [ Contraindications/Precautions ] [ Interactions ] [ Adverse Reactions ] [ Costs ] [ Chemical Structures] Classification: Anesthetics General Anesthetics Description: Propofol (2,6-diisopropylphenol) is an intravenous, nonbarbiturate anesthetic that is chemically unrelated to other intravenous anesthetics. Propofol is used to induce anesthesia that can be maintained by continuous infusion or with inhalation anesthetics. Propofol induces anesthesia as quickly as thiopental, but emergence from anesthesia is 10-times more rapid than with thiopental and is associated with minimal postoperative confusion. Only desflurane has a more rapid recovery time than propofol, but desflurane is associated with nausea/vomiting.[500] Propofol has no analgesic activity and causes sedation at a lower dosage than that needed for anesthesia. Unlike many other general anesthetics, propofol possesses antiemetic activity. Propofol (Diprivan®) received FDA approval in October 1989. In March 1997, the FDA granted exclusivity until 2015 to Zeneca for a modified formulation that contains disodium edetate (EDTA) to retard microorganism growth. A generic formulation of propofol is available, but it contains sodium metabisulfite and not EDTA as the perservative. Mechanism of Action: Propofol appears to inhibit the NMDA subtype of glutamate receptors by channel gating modulation and has agonistic activity at the GABAA receptor. Propofol enhances the amplitude of currents evoked by subthreshold concentrations of gamma-aminobutyric acid (GABA) and directly activates the GABAA receptor in the absence of GABA. Propofol activates chloride channels in the β1 subunit of GABAA, but it is unknown if propofol binds directly to the receptor, binding sites, or if the effects are a result of mediation of distinct mechanisms, such as second messengers. Propofol and benzodiazepines have similar effects on GABAA receptor deactivation but different effects on desensitization. Receptor desensitization causes a fall from a peak (activation) due to agonist application to an apparent steady state. Deactivation is the rate of decay to baseline following the termination of drug application. Both drugs slow the rate of deactivation, but only propofol decreases the rate and extent of receptor desensitization in the presence of saturating concentrations of GABA. In the presence of sub-maximal concentrations of GABA, both drugs slow the rate and extent of receptor desensitization. The anesthetic and amnesic properties of propofol may be wholely or partly a result of NMDA-mediated excitatory neurotransmission depression. The utility of propofol for refractory migraine, status epilepticus, and delirium tremens may be due to enhanced inhibitory synaptic transmission from GABAA receptor agonism or glutamate receptor inhibition. Propofol with hypocarbia increases cerebrovascular resistance and decreases cerebral blood flow, cerebral metabolic oxygen consumption, and intracranial pressure. The decrease in cerebral blood flow and intraocular pressure is likely a result of a decrease in systemic vascular resistance. Propofol does not affect cerebrovascular reactivity to changes in arterial carbon dioxide tension. Propofol has been shown to possess antiemetic properties. Propofol reduces the concentration of serotonin and 5-hydroxyindoleacetic acid in the area postrema. The reduction may be mediated by the GABAA receptor. Propofol also reduces the synaptic transmission in the olfactory cortex, which suggests a decrease in the release of excitatory amino acids like glutamate and aspartate. Propofol does not affect gastric emptying time or dopamine D2 receptors. Pharmacokinetics: Propofol is administered intravenously and, due to its high lipophilicity, is rapidly distributed to all tissues in the body. There is fast equilibration between the plasma and the brain. Loss of consciousness usually occurs within 40 seconds, although the onset of action varies with the dose, rate of administration, and extent of premedication. Propofol crosses the placenta and is distributed into breast milk. Propofol is 95—99% protein-bound. The time to tissue saturation depends on the rate and duration of the infusion. Propofol is metabolized in the liver where it rapidly undergoes glucuronide conjugation to inactive metabolites. Initially, the fall in plasma concentration is roughly 50% due to tissue distribution and 50% due to metabolic clearance. The duration of action of a 2—2.5 mg/kg bolus injection is 3—5 minutes despite a delayed release of drug from deep compartments. The steady state concentration is generally proportional to the infusion rate. The clearance of propofol exceeds estimated hepatic blood flow, which suggests extrahepatic routes of metabolism. The elimination half-life of 3—12 hours is the result of slow release of propofol from fat stores. About 70% of a single dose is excreted renally in 24 hours (90% in 5 days). The terminal half-life is 1—3 days after a 10-day infusion. Recovery from anesthesia is rapid (8—19 minutes for 2 hours of anesthesia) and is associated with minimal psychomotor impairment. The time to awakening is affected by the tissue drug concentration. The longer the infusion, the greater time to awakening, which usually occurs at a propofol concentration of 0.5 µg/mL or less. Emergence from light sedation (Ramsey score from 3 to 2) is usually less than 35 minutes if the infusion has lasted 3 days or less. The emergence time could be up to 3.5 hours or longer for patients that receive more than 3 days of propofol even if the sedation score is kept at 3. The more heavily sedated the patient, the longer the emergence time will likely be, especially for long infusion times. Longer emergence times may occur in obese patients. Significant propofol accumulation may occur with long-term propofol use. Due to peripheral tissue saturation, the rate at which the propofol concentration will fall becomes more dependent on metabolic clearance than tissue redistribution. Special populations: Total body clearance and volume of distribution of propofol are decreased in the elderly whereas these values in children between 3 and 12 years of age are similar to those of adults. The pharmacokinetics of propofol do not appear to be affected by chronic hepatic or renal disease. References 500. Van Hemelrijck J, Smith I, White PF. Use of desflurane for outpatient anesthesia. A comparison with propofol and nitrous oxide. Anesthesiology 1991;75:197—203. Propofol Print Indications...Dosage general anesthesia induction and general anesthesia maintenance: NOTE: After 30 minutes of a maintenance infusion, the rate should be downward titrated in absence of clinical signs of light anesthesia until a mild response to surgical stimulation is obtained. An increase in heart rate, blood pressure, sweating or tearing may be signs of lightening of anesthesia. As about half of the fall in plasma concentration is due to drug redistribution from tissues, around 50% of the initial rate will likely maintain the plasma concentration. Daily assessment of sedation with as needed dosage adjustment is recommended. NOTE: Propofol is indicated for anesthesia induction in children at least 3 years of age whereas propofol is indicated for the maintenance of anesthesia in children 2 months of age and older. Intravenous dosage: Adults < 55 years and ASA I or II: 40 mg every 10 seconds until induction onset (approximately 2.0—2.5 mg/kg IV). For maintenance, 100—200 mcg/kg/minute IV (6—12 mg/kg/hour) or bolus injections of 20—50 mg IV as needed. Allow 3—5 minutes between dosage adjustments in order to assess drug effects. Elderly, debilitated and ASA III and IV patients: 20 mg every 10 seconds until induction onset (approximately 1—1.5 mg/kg IV). For maintenance, 50—100 mcg/kg/minute IV (3—6 mg/kg/hour). Do not use rapid bolus administration because of the possibility of increased hypotension, apnea, airway obstruction, and oxygen desaturation. Infants, Children, and Adolescents and ASA I or II: For anesthesia induction in patients at least 3 years of age, 2.5—3.5 mg/kg IV over 20—30 seconds when unpremedicated or when lightly premedicated with oral benzodiazepines or intramuscular opioids. Within this dosage range, younger children may require larger induction doses than older children. For maintenance (patients at least 2 months of age), 125—300 mcg/kg/min IV (7.5—18 mg/kg/hr). Lower doses are recommended for ASA III or IV patients. Intravenous dosage (intermittent bolus): Adults: Increments of 25—50 mg IV as needed. Bolus does should only be used to rapidly increase the depth of sedation for patients that are unlikely to experience hypotension. •for general anesthesia induction and maintenance during cardiac procedures: Intravenous dosage: Adults: 20 mg every 10 seconds until induction onset (approximately 0.5—1.5 mg/kg IV). For maintenance, 100—150 mcg/kg/minute (approximately 6—9 mg/kg/hour) IV infusion as the primary anesthetic agent or 50—100 mcg/kg/minute (approximately 3—6 mg/kg/hour) IV infusion as the secondary anesthetic agent. When propofol is used as the primary agent, maintenance infusion rates should not be less than 100 mcg/kg/min and should be supplemented with analgesic levels of continuous opiate agonists. When an opiate agonist is used as the primary anesthetic agent, propofol maintenance rates should not be less than 50 mcg/kg/min and care should be taken to ensure amnesia with concomitant benzodiazepines. Higher doses of propofol will reduce the opiate agonist dosage requirements. •for general anesthesia induction and maintenance of neurological patients: NOTE: When increased intracranial pressure is suspected, hyperventilation and hypocarbia should accompany propofol administration. Intravenous dosage: Adults: 20 mg IV every 10 seconds until induction onset (approximately 1—2 mg/kg IV). For maintenance, 100—200 mcg/kg/minute (approximately 6—12 mg/kg/hour) IV infusion. Bolus doses are not recommended, as hypotension can compromise cerebral perfusion pressure. For sedation induction and sedation maintenance of intubated and mechanically ventilated patients during treatment in an intensive care setting: NOTE: Daily assessment of sedation with as needed dosage adjustments is recommended. Do not abruptly discontinue for weaning or sedation assessment. Rapid awakening may be associated with anxiety, agitation, and resistance to mechanical ventilation. Maintain a light sedation level throughout the weaning process until 10-15 minutes before extubation. NOTE: Sedation maintenance dosages were generally higher for patients with adult respiratory distress syndrome or respiratory failure than for other critically ill populations. NOTE: Infusion rates of more than 5 mg/kg/hour may be associated with a greater mortality risk from propofol-infusion syndrome, which may be characterized by cardiac arrest, heart failure, metabolic acidosis, or rhabdomyolysis. Tachyphylaxis to propofol does not occur with prolonged administration. Intravenous dosage: Adults: Initially, 5 mcg/kg/minute for at least 5 minutes (0.3 mg/kg/hour) as an IV infusion. Increase by 5—10 mcg/kg/minute (0.3—0.6 mg/kg/hour) every 5—10 minutes to achieve the desired level of sedation. The usual maintenance is 5—50 mcg/kg/minute IV, or more, depending on the clinical situation and other medications (i.e., opiate agonists). Based on data from six clinical studies, the mean infusion rate required to maintain adequate sedation was 27 mcg/kg/min IV (range: 2.8—130 mcg/kg/min). The infusion rate was lower in patients over 55 years of age (approximately 20 mcg/kg/min IV) compared to patients under 55 years of age (approximately 38 mcg/kg/min IV). In these studies, morphine or fentanyl was used as needed for analgesia. In postCABG patients, maintenance infusion rates are generally low (median: 11 mcg/kg/min IV) due to the intraoperative administration of high opioid doses. Children: Not recommended. Propofol is not indicated for sedation in children in the intensive care unit (ICU) and should not be used for this purpose. There have been anecdotal reports of serious adverse events and death of children with upper respiratory tract infections that received propofol for ICU sedation. •for monitored anesthesia care (MAC) sedation: NOTE: Continually monitor the patient and their oxygen saturation. NOTE: Propofol can be the sole drug for maintenance of MAC sedation during surgical or diagnostic procedures. Intravenous dosage: Adults < 55 years: Slow infusion or slow injection is preferable over rapid bolus administration to minimize the risk of apnea, hypotension, transient increase in sedation depth, and therapy recovery prolongation. Most patients require 100—150 mcg/kg/minute (6—9 mg/kg/hr) IV infusion, or 0.5 mg/kg slow IV injection given over 3—5 minutes. For maintenance infusions in most patients, an IV infusion of 25—75 mcg/kg/minute (1.5 to 4.5 mg/kg/hour) during the first 10—15 minutes, then 25—50 mcg/kg/minute adjusted to clinical response or bolus doses of 10—20 mg IV (not highly recommended). The dose and rate of administration must be individualized. A variable infusion rate is preferable over an intermittent bolus technique. Allow at least 2 minutes between dosage adjustments to determine peak drug effect. Elderly, debilitated and ASA III and IV patients: Most patients require an initiation dose similar to that required by healthy adults given by slow IV injection over 3—5 minutes. For maintenance infusion, an 80% reduction of the healthy adult maintenance dose is suitable for most patients (See adult dosage). Single or repeated rapid bolus doses should not be used because of the possibility of increased hypotension, apnea, airway obstruction, and oxygen desaturation. Children: Not recommended. Safety, effectiveness, and dosing guidelines have not been established. For the treatment of refractory status epilepticus†: Intravenous dosage: Adults: Although a definitive dosage has not been established, a loading dose of 1—2 mg/kg IV, followed by 2—10 mg/kg/hr IV as a continuous infusion has been recommended to induce anesthesia in patients with refractory status epilepticus. The maintenance dose is usually continued for 12—24 hours and adjusted according to EEG results. The primary end-point is EEG burst suppression. After 12—24 hours, the continuous infusion of propofol is withdrawn gradually. If seizures recur, therapy should be resumed for progressively longer periods, as needed.[1679] Children†: In a 9 month old with prolonged, refractory convulsive status epilepticus, seizures stopped promptly (with EEG burst suppression) after administration of propofol 3 mg/kg IV bolus, followed by an IV infusion of 100 mcg/kg/min.[1680] For the treatment of refractory migraine†: NOTE: Due to the anesthetic doses required, propofol should only be administered by an anesthetic care team. Intravenous dosage: Adults: Propofol administration to induce unconsciousness has reduced migraine pain upon awakening. Pain from three refractory headaches was greatly reduced by 0.5—1 mg/kg IV of propofol in one patient, although treatment of two headaches required repeat propofol administration at the same dosage.[4052] For the treatment and prevention of postoperative or chemotherapy-associated nausea/vomiting†: NOTE: The antiemetic effect of propofol is greatest during the infusion with an increased risk of nausea and vomiting after drug administration cessation. NOTE: Prevention of nausea and vomiting appears to be associated with a plasma propofol concentration between 280 and 530 ng/mL. Intravenous dosage: Adults: Use of subhypnotic doses of propofol (0.5 mg/kg IV) at surgery completion helps reduce nausea/vomiting; the effect of a concomitant 5-HT3 receptor antagonist is currently unknown. Administration of propofol in a subanesthetic dose (10 mg IV) produced significant symptomatic improvement in nausea/vomiting as compared to placebo-treated patients.[501] However, relapse occurred at a similar rate to the placebo group. Propofol 20 mg IV given by patient-controlled device with a 5 minute lockout period significantly reduced the average nausea score, emesis episodes, and need for rescue antiemetic therapy as compared to the placebo-treated group.[4053] Use of a 0.1—0.2 mg/kg IV bolus followed by a 1 mg/kg/hour IV infusion of propofol helps prevent and treat chemotherapy-associated nausea/vomiting that is inadequately treated with serotonin antagonists or dexamethasone. Fewer patients that received propofol for induction (2 mg/kg) and maintenance (50—150 mcg/kg/minute infusion) of anesthesia versus isoflurane vomited (19%) within 6 hours of surgery than did patients that received ondanestron (48%), propofol for induction only (64%), or propofol for only the last 30 minutes of anethesia maintenance (52%). Antiemetic use and sedation scores were also significantly lower for the group that received propofol throughout the procedure.[4054] Children: Of 90 children undergoing tonsillectomy, 93% that received propofol 120—140 mcg/kg/minute IV and ondansetron (100 mcg/kg IV) for anesthesia maintenance were emesis-free 4—6 hours after anesthesia compared with 78% of children that received only propofol.[4055] For the treatment of agitation† associated with alcohol withdrawal: Intravenous dosage: Adults: Continuous infusions of propofol controlled agitation and other symptoms of alcohol withdrawal, such as diaphoresis, tremors, and delirium in 4 patients that had a suboptimal response to benzodiazepines. Propofol was titrated to a rate (40—90 µg/kg/minute IV) that achieved sedation with rousability to a light tactile stimulus. Daily attempts were made to wean the dose; patients received propofol for 4—11 days.[4056] Patients with renal impairment: Specific guidelines for dosage adjustments in renal impairment are not available; it appears that no dosage adjustments are needed. The long-term administration of propofol to patients with renal failure has not been evaluated. Patients with hepatic impairment: Specific guidelines for dosage adjustments in hepatic impairment are not available; it appears that no dosage adjustments are needed. The long-term administration of propofol to patients with hepatic insufficiency has not been evaluated. †non-FDA approved indication [ Last revised: 8/25/2003 6:41:00 PM ] References 501. Borgeat A, Wilder-Smith OH, Saiah M et al. Subhypnotic doses of propofol possess direct antiemetic properties. Anesth Analg 1992;74:539—41. 1679. Lowenstein DH, Alldredge BK. Status epilepticus. N Engl J Med 1998;338:970—6. 1680. Harrison AM, Lugo RA, Schunk JE. Treatment of convulsive status epilepticus with propofol: case report. Pediatr Emerg Care 1977;13:420—2. 4052. Drummond-Lewis J, Scher C. Propofol: a new treatment strategy for refractory migraine headache. Pain Med 2002;3:366—9. 4053. Gan TJ, El-Molem H, Ray J, et al. Patient-controlled antiemesis: a randomized, double-blind comparison of two doses of propofol versus placebo. Anesthesiol 1999;90:1564—70. 4054. Gan TJ, Ginsberg B, Grant AP, et al. Double-blind, randomized comparison of ondansetron and intraoperative propofol to prevent postoperative nausea and vomiting. Anesthesiol 1996;85:1036—42. 4055. Barst SM, Leiderman JU, Markowitz A, et al. Ondansetron with propofol reduces the incidence of emesis in children following tonsillectomy. Can J Anaesth 1999;46:359—62 4056. McCowan C, Marik P. Refractory delirium tremens treated with propofol: a case series. Crit Care Med 2000;28:1781—4. Propofol Administration Intravenous Administration •Propofol should only be given by intravenous administration by individuals trained in the administration of general anesthetics when propofol is used for general anesthesia or monitored Print anesthesia care sedation. •Although not a controlled substance, propofol has been abused. Access restriction and accounting procedures are recommended. •Strict aspectic technique must be followed when handling propofol injection, as the lipid-based vehicle is capable of supporting rapid growth of microorganisms. Disinfect the rubber stopper of the vial or pre-filled syringe with 70% isopropyl alcohol. •Prepare the product immediately before use. Use a sterile vent spike to draw propofol out of a vial into a sterile syringe. Label the syringe with the time and date the vial was opened. •In-line filters, if used, must be at least 5 µm. Smaller pores may cause emulsion instability or clog tubings. Continuous monitoring is necessary due to the potential for restricted flow and emulsion breakdown. •Shake well before using. Visually inspect parenteral products for particulate matter and discoloration before administration whenever solution and container permit. Propofol emulsions are milky white, which makes it difficult to detect contaminates. If the emulsion appears to be separated, do not use. •Propofol (Diprivan®) has 0.005% disodium edetate and generic propofol has sodium metabisulfite to retard the growth of microorganisms in the event of accidental extrinsic contamination. Propofol is not an antimicrobially preserved product under USP standards. As propofol is a single-use product, discard unused portions and IV lines at the end of the procedure or within 6 hours of opening the vial or pre-filled syringe, whichever is sooner. The IV line should be flushed every 6 hours and at the end of the anesthesia procedure. If used for ICU sedation, discard tubing and vial after 12 hours if administered directly from the vial or within 6 hours if transferred to a syringe or other container. Dilution: •Dilution is not necessay, but if desired, use only D5W. The concentration should be no less than 2 mg/ml. •Diluted propofol is more stable when in contact with glass than with plastic. •Do not mix with other agents before administration. Direct IV injection: •Shake well before using. •Inject IV over 3—5 minutes and titrate to desired level of sedation. Intravenous infusion: •Propofol should only be administered by persons skilled in the medical management of critically ill patients and trained in cardiovascular resuscitation and airway management. •Propofol is compatible with the following intravenous fluids when administered through a y-type infusion set: D5W, lactated Ringers injection, D5LR, D5½NS, D5¼NS. •The dose and rate of administration must be individualized (see specific Dosage). •Propofol should not be coadministered through the same IV catheter with blood or plasma. Compatability has not been established and aggregates of the globular component of the emulsion vehicle with blood/plasma/serum have been noted in vitro. •Do not infuse more than 5 days in a row. A drug holiday is needed to replace estimated or measured zinc losses from chelation from EDTA. •Syringe pumps or volumetric pumps are recommended to provide controlled infusion rates. †non-FDA approved Interactions Propofol potentiates CNS depression [6892] [7808], and may enhance the sedative, respiratory depressive, and hypotensive effects of anxiolytics, sedatives, and hypnotics including barbiturates [5326], benzodiazepines, ethanol [6341], sedating H1-blockers, local anesthetics, opiate agonists, other general anesthetics, phenothiazines, and tricyclic antidepressants [5480]. A reduced dose of propofol may be needed for induction if it is used in conjunction with other medications that cause CNS depression. Morphine premedication (0.15 mg/kg) with nitrous oxide 67% in oxygen has been shown to reduce the necessary propofol maintenance infusion rate and therapeutic blood concentration when compared to non-narcotic (lorazepam) premedication. Similarly, anesthetic requirements can be reduced when propofol is used concurrently. For example, propofol appears to inhibit the metabolism of alfentanil and sufentanil whereas alfentanil at a concentration of 40 ng/ml elevated the blood concentration of propofol by 20%. The use of isoflurane, enflurane, or halothane with propofol has not been extensively evaluated. The possibility for increased hypotension and decreased cardiac output exists. Additionally, the use of fentanyl with propofol can increase the risk of bradycardia, asystole, and cardiac arrest, especially in pediatric patients. The use of articaine; epinephrine during or following treatment with general anesthetics has been associated with the development of cardiac arrhythmias, and should be avoided if possible.[5731] The administration of high-dose propofol infusions has been associated with the reversal of warfarin anticoagulation in a patient with Crohn's disease. Propofol is emulsified with soybean oil 10%, which contains vitamin K. Close monitoring of the anticoagulation effect of warfarin is recommended for patients requiring concurrent propofol. [2648] Prior to general anesthesia, carbidopa; levodopa may be continued as long as the patient is permitted to take oral medication. If levodopa-based therapy is interrupted temporarily, the patient should be observed for signs of neuroleptic malignant syndrome, and the usual dosage should be administered as soon as the patient is able to take oral medication.[752] [6657] A symptom complex resembling the neuroleptic malignant syndrome has occurred following abrupt withdrawal of antiparkinsonian drugs. Possible signs and symptoms include: muscular rigidity, hyperthermia, mental changes, increased creatine phosphokinase concentration, diaphoresis, and tachycardia. Initially, vasopressors may reduce propofol serum concentrations due to increased metabolic clearance secondary to increased hepatic blood flow. An increase in the propofol dose may be required. Additionally, the vasopressor dose may need to be increased over time due to tachyphylaxis. Thus, propofol and catecholamines may drive each other in a progressively myocardial depressive loop, which could lead to cardiac arrhythmias or cardiac failure. A positive association between the propofol infusion syndrome and norepinephrine and dopamine administration rates has been demonstrated. The propofol infusion syndrome may be characterized by myocardial infarction, metabolic acidosis, or rhabdomyolysis. St. John's wort, Hypericum perforatum, may intensify or prolong the effects of general anesthetics.[4936] The American Society of Anesthesiologists has recommended that patients stop taking herbal medications at least 2—3 weeks before surgery to decrease the risk of adverse reactions.[4937] Adverse Reactions Possible cardiopulmonary adverse effects of propofol include respiratory depression, apnea, hypotension, and sinus bradycardia. Apnea is most common during anesthesia induction. Of 1573 adult patients that received induction with 2—2.5 mg/kg, 43% had apnea whereas 27% of 218 children had apnea after receipt of 1—3.6 mg/kg. The duration of apnea is usually between 30 and 60 seconds, although it was longer than 60 seconds in 12% of adult and 6% of pediatric patients. Hypotension is the most frequently occurring cardiopulmonary effect, reported in 3—10% of adult patients and in 17% of pediatric patients. The drop in arterial blood pressure can be more than 30% and is due to reduced preload and afterload. Patients may experience dizziness, although <1% of patients reported this event during clinical trials. Administration of intravenous fluids or pressors and extremity elevation may be needed. There is usually little to no change in heart rate or cardiac output with the drop in blood pressure for patients that are breathing on their own. In contrast, a reduction in cardiac output and a greater extent of cardiac output depression are more likely for patients with assisted or controlled ventilation. Sinus bradycardia that occurs during a maintenance infusion may be due to a reduction in sympathetic activity or a resetting of the baroreceptor reflex. Propofol has no vagolytic activity. If the inhibitory effect on the heart is detrimental, administration of an anticholinergic drug to modify the increased vagal tone should be considered. Hypertension, sinus tachycardia, premature ventricular contractions (PVCs), premature atrial contractions (PACs), abnormal ECG, QT prolongation, ST-T wave changes, asystole, and cardiac arrest have occurred rarely (< 1% of patients). Fatal cardiac arrhythmias have been seen within 40—60 hours of therapy with propofol > 5 mg/kg/hour in patients with head trauma. Supraventricular tachycardia (SVT) with initially widening QRS seems to be a warning sign of these fatal arrhythmias. Cardiopulmonary adverse effects are largely dependent on the extent of premedication, propofol dosage and rate of administration, and underlying medical conditions. Cardiorespiratory depression is more likely with higher blood concentrations of propofol, which can result from the use of bolus doses or rapid increases in the infusion rate. Debilitated or elderly patients, and those with severe cardiac disease appear to experience more exaggerated responses. Patients with preexisting cardiac conduction abnormalities may have an arrhythmia exacerbation. The cardiovascular depressive effects have been attributed to direct vasodilation and negative inotropy. The respiratory depression may be due to direct suppression of the central inspiratory drive. If hypotension and respiratory depression are profound and refractory, overdose should be suspected. The use of propofol for sedation in pediatric ICU patients has been associated with an increase in mortality. A causal relationship has not been established; however, a propofol infusion syndrome in children has been described consisting of myocardial infarction, metabolic acidosis, and rhabdomyolysis.[3598] A similar syndrome has also been reported in adults.[3599] Seven of 67 patients with head injury developed signs (cardiac dysrhythmias, metabolic acidosis, hyperkalemia, muscle-cell degradation) and symptoms (heart failure) suggestive of a propofol infusion syndrome between 35 and 93 hours after the infusion began. All patients had an increasing need for inotropic and vasopressor support and received a higher mean propofol dose (6.5 mg/kg/hour) than control patients (4.8 mg/kg/hour). Of note, each patient with the syndrome had received an infusion rate of propofol greater than 5 mg/kg/hour for more than 58 hours. Furthermore, the syndrome occurred in 3 of 18 patients that received between 5 and 6 mg/kg/hour and in 4 of 13 patients that got more than 6 mg/kg/hour. Failure of oxygen delivery to tissues may be responsible for the propofol infusion syndrome. All sedative and therapeutic agents used in the intensive care unit, including propofol, should be titrated to maintain optimal oxygen delivery and hemodynamic parameters. To date, there has been no association of malignant hyperthermia with propofol. However, neuroexcitatory symptoms have been associated with propofol during and after drug administration. Neuroexcitatory symptoms may be a result of an imbalance between cortical and subcortical structures and decreased inhibitory output from the formatio reticularis. Perioperative myoclonia, rarely including seizures and a dystonic reaction known as opisthotonus has occurred with a temporal relationship to propofol administration. In clinical trials, hypertonia/dystonia occurred in < 1% of patients. Very rarely the use of propofol may be associated with the development of a period of postoperative unconsciousness that may be accompanied by an increase in muscle tone. A period of brief wakefulness may precede the event and recovery is spontaneous. There have been several cases reported in the literature. One patient became unresponsive and developed massaeter spasm 2 hours after propofol cessation. She awoke after 6 hours and reported being awake during the event. Symptoms occurred in most patients after regaining consciousness, within 7 hours of propofol cessation, and persisted for less than 24 hours, although symptom duration was longer in about a third of patients.[4058] Propofol is isotonic and has a pH between 7.2 and 8.5. An injection site reaction, characterized by burning, stinging, and pain, has been reported in 17.6% of patients enrolled in clinical trials. However, immediate or delayed discomfort may occur in as many as 90% of adults and 85% of children. Phlebitis or thrombosis occurred in <1% of patients in clinical trials. If extravasation occurs, local pain, swelling, blisters, and tissue necrosis may occur. Propofol is directly irritating to the venous intima. Propofol also activates the kallikrein-kinin system, which results in bradykinin production. Bradykinin dilates and increases the permeability of the vein. As a result, the aqueousphase propofol irritates more free nerve endings outside the endothelial layer of the vessel. Less frequent reactions include tingling, numbness, and coldness. Options to decrease discomfort include use of the larger forearm veins, such as those of the antecubital fossa or the use of lidocaine 40 mg or granisetron 2 mg both in normal saline retained in a tourniquet-occluded vein for 2 minutes. The drugs similarly reduced the severity and incidence of pain associated with propofol injection. Lidocaine 1 mL of a 1% solution is commonly used. Other options that have been shown to reduce pain on injection are tramadol 50 mg and ondansetron 4 mg injected into a vein on the dorsum of the hand after a tourniquet has been applied to the forearm. The tourniquet is released after 20 seconds and propofol administered. It appears that propofol is rarely associated with plasma histamine concentration elevation. Pruritus was noted in 2% of children and in <1% of adults that received propofol during clinical trials. Rash (unspecified) occurred in 5% of children and flushing was reported in less than 1% of patients. Anaphylactoid reactions that may include bronchospasm, erythema, hypotension, wheezing, laryngospasm, and angioedema have occurred shortly after administration of propofol. Anaphylactic shock is also possible. Because of concomitant use of other agents, a causal relationship has not been established. Likewise, pulmonary edema has been reported rarely with propofol, but a causal relationship is unknown, although a temporal relationship has been shown. Of 30 patients that received propofol infusions for ICU sedation, one developed hypertriglyceridemia (1148 mg/dl). The patient received concomitant parenteral lipids for nutrition. Discontinuance of propofol and lipids was associated with a return to normal of the triglyceride concentration within 48 hours. Although a causal relationship of pancreatitis with propofol is unclear, pancreatitis after administration of a single dose of propofol and after days of therapy has been noted. Hypertriglyceridemia has not been associated with all cases. Thus, it is speculated that propofol may cause pancreatitis through more than one mechanism. One patient without known risk factors for pancreatitis had an elevation of her serum triglyceride concentration to 1498 mg/dl along with evidence of acute pancreatitis on day 7 of propofol administration. She improved with propofol discontinuation. Subsequent inadvertent administration of a single 200 mg propofol dose was associated with abdominal pain, elevated lipase (564 mg/dl), an serum triglyceride concentration of 380 mg/dl. Zinc deficiency may occur in patients that receive prolonged therapy with propofol. Diprivan® contains 0.005% disodium edetate, which is a chelator of zinc. The mean daily urinary zinc loss in adults and pediatric patients enrolled in clinical trials was 2.5—3 mg and 1.5—2 mg, respectively. Patients at greater risk of zinc deficiency include those with diarrhea, burns, or sepsis. Generic propofol does not contain EDTA. Sepsis should be considered in patients with a fever and low blood pressure. Most studies with propofol have not examined infectious complications (other than contamination) as an outcome.[3597] Failure to use aseptic technique when handling propofol has been associated with microbial contamination of the product with fever, infection, other life-threatening illness, and/or death. Microbial contamination of propofol may occur even with use of aseptic technique. Propofol is not a microbially preserved product according to USP standards and thus, can support rapid growth of microbial organisms. Propofol is a single-use parenteral product; discard any unused portion within the specified time period (see Administration). Do not use if contamination is suspected. As determined from in vitro data, propofol may interfere with lymphocyte function, neutrophil function, and cytokine release. The clinical significance of these effects are unknown but may be greater when propofol is used for extended periods of time. Also, data have suggested that intravenous lipids (including propofol formulations) may alter the immune response to infection (e.g., interference with leukocyte migration and interleukin-2 dependent lymphocyte response). Propofol withdrawal syndrome has been described in a burn patient with concomitant bipolar disease receiving continuous IV infusions of propofol for 95 days to control extreme agitation and assist in ventilation. With each attempt to discontinue propofol, the patient required a restart of the propofol infusion to control abrupt agitation, tremors, tachycardia, tachypnea, and hyperpyrexia.[4282] Long-term infusions of propofol are controversial and no longer supported by the manufacturer, although long-term infusions have been administered without evidence of withdrawal. Although additional case reports of propofol withdrawal syndrome exist, the data are variable and inconclusive as to predict the risk factors for withdrawal. Withdrawal symptoms have been reported in patients with a duration of propofol infusion from days to several months.[4283] A propofol weaning protocol has been suggested (see Contraindications). [ Last revised: 10/11/2004 2:10:00 PM ] References 3597. Fraser GL, Riker R. Advances and controversies in adult ICU sedation, part 3: evolving pharmacological treatment issues. Hosp Pharm 2002;37:362—8. 3598. Bray RJ. Propofol infusion syndrome in children. Paediatr Anaesth 1998;8:491—9. 3599. Sharma ND, Rosman HS, Padhi D, et al. Long-term propofol infusion and cardiac failure in adult head-injury patients. Lancet 2001;357:117—8. 4058. Islander G, Vinge E. Severe neuroexcitatory symptoms after anesthesia - with focus on propofol anesthesia. Acta Anesthesiol Scand 2000;44:144—9. 4282. Cawley MJ, Guse TM, Laroia A et al. Propofol withdrawal syndrome in an adult patient with thermal injury. Pharmacotherapy 2003;23:933—9. 4283. Valente JF, Anderson GL, Branson RD, et al. Disadvantages of prolonged propofol sedation in the critical care unit. Crit Care Med 1994;22:710—12. Patient Education Print Propofol injection Propofol injection What is propofol injection? PROPOFOL (Diprivan®) is a drug that reduces anxiety and tension, and promotes relaxation and sleep or loss of consciousness. Propofol provides loss of awareness for short diagnostic tests and surgical procedures, sleep at the beginning of surgery, and supplements other types of general anesthetics. Generic propofol injection is available. What should my health care professional know before I receive propofol? They need to know if you have any of these conditions: •arrhythmia (rapid, slow, or irregular heart beat) •blood vessel disease •head injury •heart disease •high cholesterol •pancreatitis •seizures (convulsions) •an unusual or allergic reaction to propofol, anesthetics, other medicines, foods, dyes, or preservatives •pregnant or trying to get pregnant •breast-feeding How should I use this medicine? Propofol is for injection into a vein. It is given by trained anesthesia professionals in a controlled environment. Contact your pediatrician or health care professional regarding the use of this medicine in children. Special care may be needed. What if I miss a dose? This does not apply. What drug(s) may interact with propofol? •alcohol •barbiturate medicines for inducing sleep or treating seizures (convulsions) •herbal products, including St. John's wort •medicines for anxiety or sleeping problems, such as diazepam or temazepam •medicines for colds, breathing difficulties, or weight loss •medicines for mental problems and psychotic disturbances •medicines for pain Tell your prescriber or health care professional about all other medicines you are taking, including non-prescription medicines, nutritional supplements, or herbal products. Also tell your prescriber or health care professional if you are a frequent user of drinks with caffeine or alcohol, if you smoke, or if you use illegal drugs. These may affect the way your medicine works. Check with your health care professional before stopping or starting any of your medicines. What side effects may I notice from receiving propofol? Side effects that you should report to your prescriber or health care professional as soon as possible: •difficulty breathing, wheezing, swelling of the throat •fast heartbeat, palpitations •lightheadedness or fainting spells •numbness or tingling in the hands or feet •seizure (convulsion) •skin rash, flushing (redness), or itching •swelling or extreme pain at the injection site •uncontrollable muscle spasm Side effects that usually do not require medical attention (report to your prescriber or health care professional if they continue or are bothersome): •dizziness •pain or irritation at the injection site What should I watch for while taking propofol? You will be closely monitored following administration of propofol. Propofol is a very short-acting drug, and its effects generally wear off in just a few hours. However, propofol may affect your ability to drive or operate machinery for several hours after use. Do not attempt to drive yourself home if you have received propofol for minor outpatient surgery or diagnostic tests. Avoid alcohol, mood-altering drugs, or any other medicines for at least 24 hours after a dose of propofol, unless approved by your prescriber or health care professional. Where can I keep my medicine? This does not apply. [ Last Revised: 4/14/2003 7:05:00 PM ] NOTE: This information is not intended to cover all possible uses, precautions, interactions, or adverse effects for this drug. If you have questions about the drug(s) you are taking, check with your health care professional.