Coding and terminology v1.9 (10.10.07)
advertisement

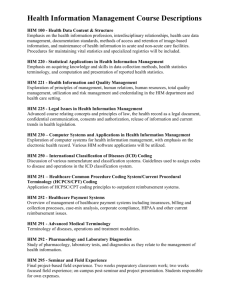
Informing Healthcare National Architecture Design Board Migration to consistent use of coding and terminology in NHS Wales: (Summary version, 1st October 2007) Content of the paper: Use of Coding and Terminology- in the healthcare environment Coding and terminology is required to support consistent communication between individual members of staff, for decision support, for measurement, secondary uses of information and increasingly to support primary uses. Use of coding and terminology – in the UK and European context NHS Wales should maintain and evolve existing links with England, Scotland and other European countries where appropriate. NHS Wales must also monitor the development and evaluation of health information systems that can support new coding systems such as Snomed CT. IHC’s principles and approach to coding and terminology Informing Healthcare plan to use a limited number of large code sets by encouraging sectors and disciplines to coalesce around the one that best suits it, either because many already use it or because a set is best suited to a particular area of care. This process is well advanced, in those areas where historically consistency has been essential for patient safety, such as in pathology systems and pharmacy. Information services and systems to support patient care. Informing Healthcare is developing new information services and systems to support patient care; including the Individual Health Record and the Welsh Clinical Portal. These systems will capture and store information about individual patients, will provide decision support in time and are the source of information for secondary uses in the future. A pragmatic approach to IHCs Programme of work. IHC propose a pragmatic, incremental approach linked to Informing Healthcare’s own programme of work. This in turn is being driven by the needs of the service to provide better information systems to support their staff and manage services. The Welsh Clinical Portal, Laboratory and Radiology systems replacement, support for the Delivering Emergency Care Services (DECS) strategy through the unscheduled care Individual Health Record programme all give opportunities to introduce an orderly, planned use of coding. ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 1 of 29 Consistent and consistently used coding and terminology in NHS Wales - Modified version for use with clinical groups. Purpose This short paper is a modified version of a paper presented at the Informing Healthcare the National Architecture Design Board meeting held in September 2007. This paper describes the pragmatic and incremental approach Informing Healthcare will be taking in relation to clinical coding and terminology and highlights Informing Healthcare’s current understanding of the order in which this work will need to be carried out in Wales. This paper does not explain the detailed approach to choosing appropriate coding systems; this detail is contained within the full document titled ‘Consistent and consistently used coding and terminology in NHS Wales, which is available on request. Use of Coding and Terminology in the healthcare environment Coding and terminology is required to support secondary uses of information and is increasingly being used to support primary uses. Information held within healthcare records serves primary and secondary uses. Primary uses relate to the actual caring for the patient, and secondary uses relate to the uses of information and data that is extracted from them. Primary uses: o Aide memoir o Clinical communication o Clinical decision making o Legal record Secondary uses include: o Health service management o Performance management o Clinical audit o Public health and epidemiology o Clinical and health service research Coding and terminology is required to support consistent recording of information to support clear communications, to enable decision support systems to operate safely, for secondary to support secondary uses, and increasingly to support primary uses: particularly in relation to storing information in electronic systems and re-using that information in different clinical contexts. The ultimate goal is the ability to extract data for secondary uses as a by-product of that collected to support direct patient care. ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 2 of 29 Use of coding and terminology – in the UK and European context NHS Wales should maintain and evolve existing links with England, Scotland and other European countries where appropriate. NHS Wales must also monitor the development and evaluation of health information systems that can support new coding systems such as Snomed CT. NHS England and Scotland are committed to roll-out Snomed CT. Informing Healthcare’s view is that there are inherent difficulties in achieving this: user resistance, lack of suitable systems currently, the scale and complexity of Snomed CT in comparison to Read 2 and 3. We also do not know of any natural language Snomed browsers that are integral to clinical systems, making its long (9 digit) codes difficult to work with. The use of coding and terminology systems around NHS Wales is largely heterogeneous and unplanned. Radiology and Pathology departments both use locally developed code sets, meaning that for any radiology or pathology concept there can be as many as fourteen codes or abbreviations. Pharmacy uses a variety of approaches including First Data Bank’s Multilex and locally developed code sets. Primary care mainly uses Read 2 but some use Clinical Terms Version 3 (CTV3), Multilex (for medicines) and the Emis Egton codes. There are specialist systems in secondary care that use various codes sets, including home-grown ones, for purposes of reporting secondary care uses ICD10 and OPCS4 (OPCS4.3 presently moving to 4.4). The central push by two large national programmes, alongside take-up in other countries, should help to bring about a new generation of health information systems that can effectively use Snomed CT and Informing Healthcare will be closely monitoring progress in this area. IHC’s principles and approach to coding and terminology Informing Healthcare plan to use a limited number of large code sets by encouraging sectors and disciplines to coalesce around the one that best suits them, either because many already use it or because a set is best suited to a particular area of care. This process is well advanced, in those areas where historically consistency has been essential for patient safety, such as in pathology systems and pharmacy. There is currently no single coding system that is demonstrably suitable for all purposes. It does not make sense to try to shoe-horn every clinical discipline and care sector into the constraints of a single set prematurely. We need to balance the need for consistency with the practical issues of what the existing coding systems can actually support and the organisational momentum or direction of travel that drive a sector or discipline towards some special approach. Our plan is to encourage the take-up of common coding systems where this is useful and to take steps to ensure the adoption of a manageably small number of coding systems across NHS Wales as a whole. Whilst acknowledging the difficulties of using coding and terminology systems, codes can help people who are recording clinical information to be consistent. By making clinical information consistent: ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 3 of 29 it is possible to exchange information without the need for extensive accompanying explanations,( provided both individuals in this exchange have the same understanding of the meaning of the coded communication). we can re-use persistent data in documenting care and creating electronic clinical communications, it is easier to process and count information for performance monitoring, analysis and planning, with accompanying rubrics information can be presented more consistently, information can be used for clinical decision support, ( though this does not require a single coding system to be used) when used properly information can contribute to clinical safety by helping to eliminate ambiguity and errors in clinical records. Failure to migrate to a consistent and common set of codes would: hinder organisational change: when health services are amalgamated or otherwise reconfigured they will encounter the obstacle of having to rapidly adopt a common coding system across the new configuration, hinder reconfiguration of health information systems: adversely affect staff mobility: when staff move between departments and organisations they will encounter widely differing approaches to recording and requesting clinical information. There are number of methods by which information can be coded and some are already in widespread use. Post event coding by clinical coders: Here the notes relating to a patient episode (usually inpatient) are manually coded by expert clinical coders. This method is largely used to enable charging, central returns and case-mix for service planning. Data quality can be an issue. Codes assigned as part of using a constrained service or results catalogue: This is being proposed in areas where there are constrained sets of services such as pathology and radiology. For example, in radiology, the national set of procedures, say 500 in total, can be put onto Radis II systems with an accompanying Snomed CT code. This code can then be used in both orders and reports. Code browser – current: Largely used by GP systems to code elements of the patient encounter. Mostly uses Read 2, but also some Egton and Read 3 (CTV3) codes. The browsing is fairly straightforward and is used to get a code that acts as an adjunct to the more detailed free text record of the encounter. Code browser – future: Snomed CT is a more powerful, expressive coding system that enables the recording of a complete term that gives a fuller description of the piece of clinical information being recorded. So, for example, it can record analysable information about anatomical site, laterality, severity and so on. At present we do not have suitable browsers, integrated into clinical applications to do this. It should be borne in mind that few systems in healthcare are capable of fully supporting complex coding systems such as Snomed CT. For the present the regular use of coding in direct patient care will be limited to the use of relatively simple code and service ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 4 of 29 browsers (as described above). These may be ‘mapped’ to Snomed-CT to support interoperability, but this is not the same as full implementation. Information services and systems to support patient care. Informing Healthcare is developing new information services and systems to support patient care; including the Individual Health Record and the Welsh Clinical Portal. These systems will capture and store information about individual patients, provide decision support in time and are the source of information for secondary uses in the future. Ultimately, the new systems and services are likely to replace many of the current reporting flows (e.g. central returns to PEDW, some national clinical audits). However, this is some time away: the new services and systems that are being developed and implemented now, and over the next few years, will take several years to cover the whole of healthcare. It will take them even longer to contain sufficiently complete information to replace all existing flows. Even then it will be necessary to assess whether data captured for direct patient care can fully support the secondary uses, and some existing information flows will persist. It is impossible to be precise about the timescales for this, but it is unlikely to be done on a large scale before 2015 (although some small scale proof of concept work will be undertaken earlier). All that can be said with certainty at this time is the existing systems and new services will run in parallel for the foreseeable future, until such a time exists where the value of the two can be compared. As we help to join up healthcare by integrating electronic systems and services (and displaying the information within them in a way that provides a consistent and complete view of individual’s health and care), we will need to simultaneously introduce consistency in the use of codes and terminologies. This will benefit secondary uses as well by enabling more valid aggregation and analysis. A pragmatic approach to IHCs Programme of work. IHC propose a pragmatic, incremental approach linked to Informing Healthcare’s own programme of work. The Welsh Clinical Portal, Laboratory and Radiology systems replacement, support for the Delivering Emergency Care Services (DECS) strategy through the unscheduled care Individual Health Record programme all give opportunities to introduce an orderly, planned use of coding. The plans will be based on practical, immediate needs of the NHS Wales sectors that we work with: clinical safety, efficiency and improved patient experience. We cannot predict every future requirement of coding in Wales, so we will be flexible and regularly review our strategy. ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 5 of 29 Our current understanding of the order in which this work will need to be carried out in Wales is: Current expectations for coding systems 1. Urgent unscheduled care (Out of Hours and NHS Direct). Consistent standards are needed: Currently Read 2 – this determined by extraction of patient records from GP systems. Follow any changes of use of code sets in primary care. For out of hours IHR in Gwent by October 2006 2. Pathology where modernisation programmes and new information systems planned. Create an all-Wales catalogue of pathology services. Attach the relevant Snomed CT and Read 2 code to each set and individual test. For procurement of new LIMS by September 2008 3. Radiology where, similarly to pathology, modernisation programmes and new information systems planned. Create an all-Wales catalogue of radiology services. Attach the relevant Snomed CT and Read 2 code to each entry in the catalogue. For radiology procedures by December 2008 4. Pharmacy / prescribing where there is an institutional push towards the Dictionary of Medicines and Devices (dm+d), driven by patient safety initiatives around the maintaining an accurate medications record Use dm+d in line with current thinking in the pharmacy community. 5. Welsh Clinical Portal. Consistent and coherent views of clinical information, clinical documentation including: requests, transfers of care, letters, discharges and notes For the foreseeable future, the Portal will receive information using a variety of code types and no codes at all. For DECS by (tbc) For radiology reports by (tbc) For transcription of medicines for piloting by December 2008 For e-prescribing by (tbc) Data capture in the portal will be a variety of codes depending on the type and purpose. Likely to include Read v2, CTV3 and Snomed-CT. 6. Primary care. Clinical documentation for referrals. Read 2 and CTV3 for the foreseeable future. Encourage users of Egton codes to migrate to Read 2. Await developments in primary care systems; i.e. will they migrate to Snomed CT? 7. Cancer care. Discuss options with cancer care community. Presently considering migration to Snomed CT. For test requesting by September 2007 For structured clinical documents by June 2008 For detailed clinical assessments and documentation by (tbc) For referral communications from 1º care by December 2008 For cancer care by (tbc) It is clear that much of this work will need to proceed in parallel given the timescales that are expected for delivery of these developments. ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 6 of 29 Informing Healthcare National Architecture Design Board Document Title: Migration to consistent use of coding and terminology in NHS Wales Document Lead: Robin Mann - Head of Clinical Design Date written: 1st October 2007 Version: QA v1.9 (updated with summary version) For NADB October 2007: V1.8 approved September 2007. This version with summary is for information only. Purpose This paper describes the pragmatic and incremental approach Informing Healthcare will be taking in relation to clinical coding and terminology. It highlights Informing Healthcare’s current understanding of the order in which this work will need to be carried out in Wales. The consistent use of coding and terminology across NHS Wales will have benefits in both the direct provision of care and for planning and management. However, the usefulness and applicability of coding systems is different in each specialist area and we do not propose the immediate mass migration to one system (e.g. Snomed-CT). This paper sets-out to identify those areas where the options are relatively clear cut as well as those where significant uncertainty still exists, and to start the discussions that will be needed to decide the way forward. Coding and terminology systems bring with them difficulties and risks as well as the widely perceived benefits. We describe and discuss some of these problems and how we can address them. The adoption of coding and terminology systems is the concern of bodies including the National Architecture Development Board, the Welsh Information Governance and Standards Board, the Royal Colleges, specialist professional groups and those who are bringing about change on the ground. Informing Healthcare is discussing governance and decision making with the relevant interested parties to arrive at a suitable approach. Recommendation. The Board is asked to approve the pragmatic approach proposed in the paper. Recommendations concerning specific care sectors will be brought to the Board from time to time, for consideration, in the context of the overall approach described here. ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 7 of 29 1 Overview and strategic context 1.1 Introduction Information held within healthcare records serves primary and secondary uses (not to be confused with primary care and secondary care). Primary uses relate to the actual caring for the patient, and secondary uses relate to the uses of information and data that is extracted from them. Primary uses: o Aide memoir o Clinical communication o Clinical decision making o Legal record Secondary uses include: o Health service management o Performance management o Clinical audit o Public health and epidemiology o Clinical and health service research Coding and terminology is required to support secondary uses, and is being increasingly used to support primary uses: particularly in relation to storing information in electronic systems and re-using that information in different clinical contexts. The ultimate goal is the ability to extract data for secondary uses as a by-product of that collected to support direct patient care. Informing Healthcare is developing new information services and systems to support patient care; including the Individual Health Record and the Welsh Clinical Portal. These will capture and store information about individual patients and are a potential source if information for secondary uses, subject to the appropriate information governance controls and restrictions (figure 1). Ultimately, the new systems and services are likely to replace many of the current reporting mechanisms (e.g. central returns to PEDW, some national clinical audits). However, this is some time away: the new services and systems that are being developed and implemented now, and over the next few years, will take several years to cover the whole of healthcare. It will take them even longer to contain sufficiently complete information to replace all existing mechanisms. Even then it will be necessary to assess whether data captured for direct patient care can fully support the secondary uses, and some existing information flows will persist. It is impossible to be precise about the timescales for this, but it is unlikely to be done on a large scale before 2015 (although some small scale proof of concept work will be undertaken earlier). All that can be said with certainty at this time is the existing systems and new services will run in parallel for the foreseeable future, until such a time exists where the value of the two can be compared. ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 8 of 29 When realised, the vision of clinical coding becoming automated as part of clinical care will mean that coding staff will be able to use their skills in far more innovative ways, including the validation of clinical codes destined for secondary uses. Informing Healthcare is leading the professional development of health informatics staff in Wales and will review and support changing roles over time. As we help to join up healthcare by integrating electronic systems and services (and displaying the information within them in a way that provides a consistent and complete view of individual’s health and care), we will need to simultaneously introduce consistency in the use of codes and terminologies. This will benefit secondary uses as well by enabling more valid aggregation and analysis. Figure 1 Possible future state: information captured about individual patients is a source if information for secondary uses, subject to the appropriate information governance controls and restrictions. Existing data flows (e.g. to PEDW) are likely to continue in parallel for some time. 1.2 This document This paper describes our pragmatic approaches to move NHS Wales towards a more coherent and consistent use of clinical coding and terminology. It should be viewed as a description of how this work will be taken forward with the Welsh health informatics community at large, the National Architecture Development Board (NADB), the Welsh Information Governance and Standards Board (WIGSB), clinical professional bodies and Trust informatics leads. There are no ‘locked down’ solutions in this paper. It introduces a pragmatic approach that can be delivered incrementally in Wales, driven by the delivery of new and replacement clinical systems over time. ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 9 of 29 Comments, proposals and information about the planned or current use of code sets in organisations or domains are very welcome and should be emailed to: Dr Robin Mann, Head of Clinical Design, Informing Healthcare: robin.mann@ihc.wales.nhs.uk 1.3 A pragmatic approach We propose a pragmatic, incremental approach linked to Informing Healthcare’s own programme of work. The Welsh Clinical Portal, Laboratory and Radiology systems replacement, support for the Delivering Emergency Care Services (DECS) strategy through the unscheduled care Individual Health Record programme all give opportunities to introduce an orderly, planned use of coding. The plans will be based on practical, immediate needs of the NHS Wales sectors that we work with: clinical safety, efficiency and improved patient experience. We cannot predict every future requirement of coding in Wales, so we will be flexible and regularly review our strategy. Our current understanding of the order in which this work will need to be carried out in Wales is: Consistent standards are needed: 8. Urgent unscheduled care (Out of Hours and NHS Direct). For out of hours IHR in Gwent by October 2006 For DECS by (tbc) 9. Pathology where modernisation programmes and new information systems planned. 10. Radiology where, similarly to pathology, modernisation programmes and new information systems planned. 11. Pharmacy / prescribing where there is an institutional push towards the Dictionary of Medicines and Devices (dm+d), driven by patient safety initiatives around the maintaining an accurate medications record 12. Welsh Clinical Portal. Consistent and coherent views of clinical information, clinical documentation including: requests, transfers of care, letters, discharges and notes For procurement of new LIMS by September 2008 For radiology procedures by December 2008 For radiology reports by (tbc) For transcription of medicines for piloting by December 2008 For e-prescribing by (tbc) For test requesting by September 2007 For structured clinical documents by June 2008 For detailed clinical assessments and documentation by (tbc) 13. Primary care. Clinical documentation for referrals. For referral communications from 1º care by December 2008 ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 10 of 29 Consistent standards are needed: 14. Cancer care. Discuss options with cancer care community. For cancer care by (tbc) It is clear that much of this work will need to proceed in parallel given the timescales that are expected for delivery of these developments (figure 2). Figure 2 Current timescales for selection of coding and terminology for different clinical domains in Wales (dotted lines are for illustration only – these timescales to be confirmed. 1.4 The current situation NHS Wales. The use of coding and terminology systems around NHS Wales is largely heterogeneous and unplanned. Radiology and Pathology departments both use locally developed code sets, meaning that for any radiology or pathology concept there can be as many as fourteen codes or abbreviations. Pharmacy uses a variety of approaches including First Data Bank’s Multilex and locally developed code sets. Primary care mainly ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 11 of 29 uses Read 2 but some use Clinical Terms Version 3 (CTV3), Multilex (for medicines) and the Emis Egton codes. There are specialist systems in secondary care that use various codes sets, including home-grown ones. Clinical coding in secondary care for purposes of reporting uses ICD10 and OPCS4 (OPCS4.3 presently moving to 4.4). Coding and terminology systems. There is no ideal coding and terminology system. There are no computer systems in current use that can manage the structure of Snomed CT. In all of the available systems, terms can be ambiguous and interpretation can differ between individuals and between groups1. The categoric assumption that coding is “the solution to the problem” fails to define either problem or solution. Sections 5.2.2. and 5.2.3 give examples of the pitfalls for the unwary and the broader systemic problems associated with the use of coding systems. 1.5 Principles and approach Whilst taking caution from the difficulties of using coding and terminology systems, codes can help people who are recording clinical information to be consistent, both with other people who are recording clinical information and across their own activities. By making clinical information consistent: it is possible to exchange it without the need for extensive accompanying explanations, we can re-use persistent data in documenting care and creating electronic clinical communications, it is easier to process and count information for performance monitoring, analysis and planning, with accompanying rubrics it can be presented more consistently, it can be used for clinical decision support, and when used properly it can contribute to clinical safety by helping to eliminate ambiguity and errors in clinical records. Failure to migrate to a consistent and common set of codes would: hinder organisational change: when health services are amalgamated or otherwise reconfigured they will encounter the obstacle of having to rapidly adopt a common coding system across the new configuration, hinder reconfiguration of health information systems: similarly to health services, change will have the obstacle of different coding systems, adversely affect staff mobility: when staff move between departments and organisations they will encounter widely differing approaches to recording and requesting clinical information. There is currently no single coding system that is demonstrably suitable for all purposes. It does not make sense to try to shoe-horn every clinical discipline and care sector into Differences in clinical terming and classification by doctors and at Withybush General Hospital. Pembrokeshire and Derwen NHS Trust and The School of Post Graduate Studies, University of Wales College of Medicine, 2000. 1 ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 12 of 29 the constraints of a single set. We need to balance the need for consistency with the practical issues of what the existing coding systems can actually support and the organisational momentum or direction of travel that drive a sector or discipline towards some special approach. It is our plan to mandate a limited number of large code sets and encourage sectors and disciplines to coalesce around the one that best suits it, either because many already use it or because a set is suited to a particular area of care. 1.6 Choosing appropriate coding systems The development of functionality to capture data through the Welsh Clinical Portal, a national approach to Radiology provision (including Radis II system support), Pathology Modernisation and national approaches in other areas of care all require a consistent, planned set of codes. Additionally, we need to provide more useable information for secondary uses such as the Corporate Health Information Programme (CHIP), Access 2009 reporting, statistical analysis, epidemiology, health services research and public health. Each of these programmes of work will drive their own uses of coding systems within the overall strategy adopted across Wales. Reducing the variety of code sets and increasing the take-up of common sets will bring about a more manageable position, enabling organisational change, creating better clinical communication and providing a stepping-off point for a national move towards a single common code set, but only when and if this becomes necessary. We must be careful that coding does not become a solution in search of a problem. Coding is useful, but before effort is expended on introducing and using it in any area of care, we must be clear what the benefits are and how sustainable that use of codes will be. 1.7 The strategic context 1.7.1 NHS Wales 1.7.1.1 Individual Health Record in unscheduled care Informing Healthcare has developed the emergency health record in Gwent. This is the first step towards a national Individual Health Record, which will be introduced across Wales in regions. The development has enabled data from GP systems to be represented in a consistent format to users in the Out of Hours setting. This has shown that it is possible to integrate data that is recorded using different coding systems in a common format for use in direct patient care in this environment. However this has not been a straightforward task and it is clear that a common coding system would be more manageable. Future roll out of the IHR will not be dependent on common GP system coding, but migration to this will support more sophisticated views and information exchange in the future. To further this, IHC will work with the primary care programme in the development of the minimum systems specification for GP systems. 1.7.1.2 Informing Healthcare: the Welsh Clinical Portal and the National Architecture strategy The Welsh Clinical Portal and the National Architecture, two closely interrelated developments, require consistent, predictable use of code sets. 1. The Welsh Clinical Portal will be drawing on Individual Health Record (IHR) and Patient Care Record Service (PCRS) information that has, in turn, been drawn from a number of sources, to ‘view’ the current state of an individual and their historical record of clinical encounters (care events). The portal will need to cope with more ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 13 of 29 than one coding set (pathology and pharmacy alone should account for Read 2, dm+d and Snomed CT), but to ensure the safe representation of information from different sources this variety needs to be predictable and limited to the necessary minimum. The presentation and use of information within the Welsh Clinical Portal will be governed by the application of constraints described in the Generic Information Framework for Individual Health Records (GENIFIR) and related information models. 2. The portal will be used to request tests, other diagnostic services and medicines. These need to be based upon common service catalogues using common codes that can be used by different services around NHS Wales. 3. In the medium term the portal will be used to create documents: referrals, clinic letters, discharges etc.. Consistent and predictable code sets will make this possible. 4. In the longer term, the IHR, PCRS and related information services will be required to provide clinical decision support on the basis of the information in the individual’s record. There is little prospect of being able to do this correctly unless the information uses recognised and orderly code sets. 1.7.1.3 NHS Wales plans A number of plans are in place in NHS Wales where coding issues, and especially the lack of commonality across the service will be encountered. Two of these are briefly described below. Trust reorganisation and service reconfiguration. Amongst other Designed for Life plans, some of the smaller Trusts are being amalgamated and their constituent parts, including diagnostics, will be rationalised. Again coding issues will arise and we should take the opportunity to plan. Pathology and radiology modernisation. Whilst it is not intended to amalgamate all diagnostic services, there is a plan to have a single ‘view’ of radiology and pathology services and information across Wales. This plan includes the replacement of the current diagnostic departmental care management systems (largely Telepath and Radis). The advent of these new systems presents an opportunity introduce a planned approach to coding. 1.7.1.4 Activity reporting National activity, waiting list and central returns from secondary care are drawn from PAS using ICD and OPCS. Primary care contract returns are sent in Read 2 and drawn from the information used in direct patient care. The primary care approach works well because it collects information as a by-product of the core business. Secondary care is less ideal: activity data collected from PAS is not regarded as part of clinical care and activity can be coded twice, once for clinical purposes and once to create returns. It may be possible in the longer term to collect information for the purposes of giving care, probably not using ICD and OPCS, and extracting this information for analysis and returns, possibly using the original clinical coding system. By using a limited set such as Snomed CT, Read 2 or dm+d, it should then be possible for those using this returned information to convert into ICD and OPCS if they need to. ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 14 of 29 1.7.2 England and Scotland NHSs England and Scotland are both committed to roll-out Snomed CT. There are inherent difficulties in achieving this: user resistance, lack of suitable systems, lack of any systems and the complexity of Snomed CT in comparison to Read 2 and 3, especially the need to retain the full clinical context for Snomed information. We also do not know of any natural language Snomed browsers that are integral to clinical systems, making its long (9 digit) codes difficult to work with. However, the central push by two large national programmes, alongside take-up in other countries, should help to bring about a new generation of health information systems that can effectively use Snomed CT. NHS Wales should maintain and evolve existing links with England, Scotland and indeed other countries where appropriate, and monitor the development and evaluation of health information systems that can support Snomed CT. 1.7.3 Maintenance and support for code sets Snomed CT and dm+d are strategic products that are backed by Connecting for Health. Snomed CT is supported by a full roll-out within NHS England by CfH and dm+d is supported by CfH and the Prescription Pricing Authority “The dm+d will become the NHS standard for medicines and device identification”2. The original authors of Snomed CT, the College of American Pathologists and CfH have now handed its future to the newly created International Healthcare Terminology Snomed Development Organisation (IHTSDO) so there is some uncertainty about its future direction, but for the moment we can assume that Snomed CT has a significant future. NHS Wales will be represented on the governing committees of the UK Terminology Centre, which acts as the UK arm of the IHTSDO. Connecting for Health, the owner of Read 2, plans that it will eventually be abolished, and issued a letter entitled “Discontinuation of the Read codes” giving a withdrawal date of 31st December 2005. However, this has since been withdrawn. The use of Read 2 is so extensive, especially in primary care around the UK, that it is likely to be supported for some time into the future. Once support ceases this will not make Read 2 unusable although its value will slowly degrade as new requirements arise which are not incorporated into the code set. 1.7.4 Snomed CT Discussions around Snomed CT can leave the impression that it is complete and ubiquitous. This is not so. As has been mentioned, no current health information systems can manage the full structure of this system and development plans for even the most advanced of these information systems do not envisage adoption until 2013/14. Nonetheless, it is the only set that is sufficiently rich to cover a number of areas of medicine, including histopathology and radiology, and for this reason the use of simple Snomed CT codes/terms is being considered for ordering and reporting of investigations. This simple use does not seek to exploit the full structure of Snomed CT but it indicates a pragmatic step towards full adoption when developments in the code set itself and health information systems allow. In other areas, there is no pressing case to adopt Snomed CT. For example, primary care largely uses Read 2. Two GP system suppliers are planning to adopt Snomed CT. We should await their progress and willingness of Welsh GPs to adopt it. 2 http://www.dmd.nhs.uk/about ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 15 of 29 2 Requirements 2.1 Criteria and constraints Our plan is to encourage the take-up of common coding systems where this is useful and to take steps to ensure the adoption of a manageably small number of coding systems across NHS Wales as a whole. The practical avenues we propose to get to a consistent position are intended to meet certain criteria: consistent clinical communication, processable information for decision support, consistent presentation of information for clinical care, analysable information for national returns, research and statistics, sufficient diversity for a diverse service, but no more than that, achievability within current organisation and system constraints. There are number of methods by which information can be coded and some are already in widespread use. Post event coding by clinical coders. Here the notes relating to a patient episode (usually inpatient) are manually coded by expert clinical coders. This method is largely used to enable charging, central returns and case-mix for service planning. Data quality can be an issue. Codes assigned as part of using a constrained service or results catalogue. This is being proposed in areas where there are constrained sets of services such as pathology and radiology. For example, in radiology, the national set of procedures, say 500 in total, can be put onto Radis II systems with an accompanying Snomed CT code. This code can then be used in both orders and reports. Code browser – current. Largely used by GP systems to code elements of the patient encounter. Mostly uses Read 2, but also some Egton and Read 3 (CTV3) codes. The browsing is fairly straightforward and is used to get a code that acts as an adjunct to the more detailed free text record of the encounter. Code browser – future. Snomed CT is a more powerful, expressive coding system that enables the recording of a complete term that gives a fuller description of the piece of clinical information being recorded. So, for example, it can record analysable information about anatomical site, laterality, severity and so on. At present we do not have suitable browsers, integrated into clinical applications to do this. It should be borne in mind that few systems in healthcare are capable of fully supporting complex coding systems such as Snomed CT. For the present the regular use of coding in direct patient care will be limited to the use of relatively simple code and service browsers (as described above). These may be ‘mapped’ to Snomed-CT to support interoperability, but this is not the same as full implementation. 2.2 General approaches Common coding system within domains. Some domains require their own coding system, or else there is a strong push within that domain to move towards a specific ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 16 of 29 approach. For example in Pharmacy, there is a move towards dm+d (see survey below). What we do need is consistent use of a coding system within a domain. This will make the world into a much more predictable place where, for example, we will know that pharmacy / prescribing will always use dm+d. It is assumed that coded information, from whatever source, will be accompanied by a free-text rubric. This means that we can have consistent communication and presentation because, where the rubric is available for viewing, human readers will quickly adapt to the consistent use of multiple coding systems. With correct mapping between coding systems we will also have information that is countable for analysis (see discussion on translation below.) The main drawback of this approach is that it will be more difficult to process coded information, say for decision support or creating alerts by the IHR. To do these things our processing systems would need to support two things: the ability to process information from multiple code sets, the storage of full provenance of each code used, showing which code set and the version it belongs to. Achievability will depend upon the availability of suitable care management systems, the willingness of people to move over to a new approach or the existing penetration of one of our mandated code sets into the domain. Common coding system within a sector. This is similar to the idea of common coding systems within domains. So, for example, Primary Care could move towards its obvious choice which is Read 2 (5 byte) and the same constraints and criteria would apply. Use of multiple code sets. Whilst our constrained code-set list makes things more manageable, some applications and information users will still need to use multiple coding systems, e.g. The Welsh Clinical Portal, the Patient Care Record Service and the Individual Health Record will draw upon information from different code sets and will expect to display this in an orderly way and also interpret and act on this information. Welsh Assembly Government planners, local planners, public health and researchers, whilst primarily using ICD10 and OPCS4 returns will also be seeing returns using other code sets. The Swansea All-Wales Information Linkage (SAIL) project is an example of a research initiative that is linking data from multiple sources with different code sets, where early outputs indicate that this is effective for many types of analysis. Clinical documents, referrals, discharge communications, clinic letters. These documents will draw on information from various sources and will contain mixed codes depending on the source. Although clinical documents created using the Welsh Clinical Portal may ultimately be created in a common code set there will still be a need to represent clinical terms in other code sets so that they can be transferred to certain other systems (for example, a discharge communication may contain SnomedCT codes for diagnoses, but may also need to contain the Read 2 equivalent to get the information into a particular GP system) To do this successfully will require mappings between code sets that really establish equivalence of meaning between the concepts that each code-set contains. There are mapping tables in existence (see Section 4) and these will need to be assessed for suitability for each need. Whilst accurate mapping between codes and concepts for ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 17 of 29 analysis of returns is highly desirable, errors would not be life-threatening. However, such errors would be unacceptable if they occurred in the Welsh Clinical Portal when the information was being used to support the direct care of an individual. 2.3 Requirement by sector and domain The requirements and choices described below are pragmatic but aimed at bringing about a more uniform use of code sets across NHS Wales. These choices will be validated with those affected and any changes necessary made to the plans. Where there are existing plans within a sector we expect to work in conjunction with those plans. 2.3.1 Overall requirement (summary) Timing Sector / Domain Current position / current thinking To coincide with LIMS replacement. Pathology Requests. Create an all-Wales catalogue of pathology services. Attach the relevant Snomed CT and Read 2 code to each set and individual test. Results. TBD To coincide with RIS replacement. Radiology Requests. Create an all-Wales catalogue of radiology services. Attach the relevant Snomed CT and Read 2 code to each entry in the catalogue. Results. TBD Largely driven by external events: PSU adoption of dm+d, NHS England, MSS. Pharmacy / prescribing / transcription / dispensing Use dm+d in line with current thinking in the pharmacy community. Timing to coincide with the roll-out of the unscheduled care record. Urgent care (OOH & NHSD) + DECS Currently Read 2 – this determined by extraction of patient records from GP systems. Follow any changes of use of code sets in primary care. Starting with Portal 1: September 2007. Welsh Clinical Portal For the foreseeable future, the Portal will receive information using a variety of code types and no codes at all. N/A Primary care Read 2 and CTV3 for the foreseeable future. Encourage users of Egton codes to migrate to Read 2. Await developments in primary care systems; i.e. will they migrate to Snomed CT? TBD Cancer care Presently considering migration to Snomed CT. To coincide with the transfer of care Referrals Probably Read 2 (and dm+d for medications) ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 18 of 29 communications programme. To coincide with the transfer of care communications programme. Additionally allow the use of Snomed CT for referrals from non primary care sources. Discharges Migrate to using the three main codes sets (Read 2, dm+d and Snomed CT). Eventually migrate to Snomed CT. Unified assessment TBA The summarised requirements described above are discussed in more detail below. 2.3.2 Detailed requirement Pathology Objectives Pathology throughout Wales is being modernised and reorganised. In the and future, local labs will pass specialist requests to larger labs and results will be background reported via the same route. In addition, the Welsh Clinical Portal will require information that is predictably coded. It is also possible that there will be a single national results repository. The objective, as part of the modernisation programme, is to support and enable all of these developments by replacing local code sets with a universal code set or sets that enables NHS Wales pathology to be requested and reported consistently. There is a general acceptance within the NHS Wales pathology community that a single code set is needed. Approach Requesting. Welsh pathologists are currently building a pathology services handbook containing some hundreds of order sets and between one and two thousand individual tests. The plan is to attach Snomed CT and (if available) Read 2 codes to each of the items and sets in the catalogue. This means that the codes will be automatically associated with requests as part of the process of selecting tests from the catalogue. Reporting. It may be possible to adopt a similar approach with reports. Indeed, some branches (histopathology and cytology) already use Snomed codes to report. Reporting uses a larger code-set than requesting, requiring more work to set-up. Blood bank. TBA Radiology Objectives Radiology throughout Wales is being modernised and reorganised. In the and future, radiology departments will get requests and report results to a wider background range of service users than at present and it will be necessary to have a universal code set to allow services to be requested and reported consistently. In addition, the Welsh Clinical Portal will require information that is predictably coded. As part of the modernisation programme, replace ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 19 of 29 local code sets with a single code set. Approach Only Snomed CT meets the detailed requirements of imaging.* Similarly to pathology, for requesting codes would be assigned from those contained in a constrained service catalogue. Reporting needs further discussion and investigation with the radiology community. *although recently there have been interim standards for radiology investigations proposed that require evaluation Pharmacy / prescribing / transcription / dispensing Objectives Pharmacy is moving towards dm+d. There are a number of factors and supporting this move: background 1. the Prescribing Services Unit is considering moving all reporting to dm+d, 2. the English Prescription Pricing Authority is moving all reporting to dm+d, 3. the Primary Care IM&T programme’s Minimum Systems Specification (MSS) Scoping Study has proposed that dm+d should be used for primary care prescribing, and in primary care systems’ drugs databases, 4. there is a proposal that, with the exception of chemotherapy, all secondary care pharmacy and prescribing should use dm+d. Each dm+d code carries a Snomed CT code. There is clearly a ‘direction of travel’ in pharmacy and prescribing towards a single code set which should be endorsed. Approach Ensure that dm+d is adopted alongside the arrival of computer supported pharmacy, prescribing, e-prescribing, dispensing and reporting, Urgent care (Out of Hours and NHS Direct) and DECS Objectives Out of hours services in Wales mainly use the Adastra system for care and management. Adastra does not code information. background NHS Direct use the CAS system that does not code information.3 The Informing Healthcare Unscheduled Care Record project is making Read 2, and possibly Read 3 (CTV3) information which has been extracted from primary care systems available to Out of Hours users. This is currently being done in Gwent, and it is planned to extend to other parts of Wales and to other services (such as A&E) in Gwent in the near future. 3 To be confirmed ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 20 of 29 The Unscheduled Care Record project provides a “view” of the patient’s record that is divided into areas such as current problems, current medications and allergies. These views come from multiple types of source system and the only way of arranging them into the correct categories is to have a clinical code associated with each data item that can be used to decide where it belongs. In the future we should plan for Out of Hours clinicians to enter new information onto the unscheduled care record. Our objective here is to maintain a manageable unscheduled care record and to stay in line with developments in primary care computing. Approach The only available option is to accept Read 2 and Read 3 information that has been extracted from primary care systems. Information input by users of the unscheduled care record should use Read 2. Urgent care records will increase their footprint to ambulance and A&E as the Delivering Emergency Care Services (DECS) strategy comes on-stream and it will be necessary to review at this point to ensure that these new sectors are incorporated in an orderly fashion. Welsh Clinical Portal Objectives The Welsh Clinical Portal will accept information from a number of sources and and for the foreseeable future these will be coded using different code sets background and none. Patient information will also be entered into the portal. Our objective is to decide upon a ‘native’ coding system for information entered on the Welsh Clinical Portal. Approach From the obvious choices of Read 2 or Snomed CT the current option would be Read 2. This is because, at present, we do not know of any suitable Snomed CT browsers that could be incorporated into the portal. When it becomes available it may be possible to incorporate a Snomed CT integrated browser. Primary care Objectives Encourage the majority of practices that already have Read 2 to maintain it. and If possible wean the practices that use Egton and home-grown coding background systems off these and towards Read 2. Enter into discussion with practices that use CTV3 and their suppliers to find ways of enabling them to provide Read 2 mappings on exported datasets and messages. The Prescribing Services Unit and Primary Care Division are mandating dm+d for prescribing returns so primary care systems will use both Read 2 and dm+d. ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 21 of 29 Approach Continue with Read 2 and dm+d. Monitor the commitment of CfH to continue to maintain Read 2 and, when and if necessary, migrate primary care to Snomed CT. When and if Read 2 support is withdrawn, the degradation of Read 2 will be gradual, so the move to Snomed CT does not need to be rapid. Cancer care Objectives Currently use Read 2, ICD10 and OPCS4 and plan to migrate to Read 3 and (CTV3). background The current plan takes the cancer community outside the ‘approved’ codes. Snomed CT is arguably a better candidate than CTV3 because it has greater detail of cancer types, staging, and complex operations and procedures. Approach Discuss migration to Snomed CT with representatives of the cancer community. Look at the feasibility of using Snomed CT via a browser that is not integrated into ISCO. Discuss the option of integrating a Snomed CT browser into ISCO. Referrals Objectives The objective of including clinical codes in referrals is to improve accuracy and and to enable the referrals to be more easily processed and reported at the background receiving end. Most referrals that could be generated by a computer would come from primary care so Read 2 would be the natural choice. IHC is examining the Scottish SCI gateway system as a suitable way of making referrals. SCI Gateway can carry codes from any code set, so there is no impediment to Read 2 if SCI Gateway is selected. Approach Adopt Read 2 (and dm+d for medications) as the code set for use in referrals but additionally allow the use of Snomed CT or Read 2 for referrals from non primary care sources. Plan to migrate all referrals to Snomed CT as primary care systems migrate to Snomed CT. Use codes and terms in the context of the use of HL7 CDA (Clinical Document Architecture) as the structure for referral documents. Discharges Objectives and The objective of including clinical codes in discharges is to improve accuracy and to enable the referrals to be more easily processed and reported at the ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 22 of 29 background receiving end. The contents of discharge communications are collected from several sources: wards, pharmacy, pathology, radiology, theatre etc. and generally they are not prepared using computerised support other than a word processor. Furthermore many of the sources do not have clinical systems and, of those that do, some (possibly most) use local, non standard, code sets. We envisage that the first opportunity to support the widespread preparation and dispatch of electronic discharge letters will come with the Welsh Clinical Portal. This will be a mixture of text and coded information. In the longer term Referrals should reflect the three choices we have allowed: Snomed CT, Read 2 and dm+d. It is possible that any one communication could contain all three code sets and each instance of coded information should be accompanied by code set and version identifiers. Approach For the foreseeable future, discharge communications will reflect the diversity of use of local and normative code sets in NHS Wales. This diversity will gradually resolve itself, first into the ‘approved’ code sets and then towards the use of Snomed CT alone. Use codes and terms in the context of the use of HL7 CDA (Clinical Document Architecture) as the structure for discharge documents. Unified assessment Objectives TBA and background Approach ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 23 of 29 3 Implementation and migration approach It is neither necessary nor practical to push all sectors and organisations in NHS Wales towards some ideal solution immediately. Proposed approaches within sectors should be chosen where there is some urgency and where current organisational developments can be “leveraged” to bring about a solution. Activities can be phased to enable planning to take place in good time, whilst also dealing with urgent cases. The stages listed below are not intended to be consecutive, there is intended to be considerable concurrency. 3.1 Stage 1 – Immediate Immediate gains can be made in sectors where there are already plans in place to change working practices, reorganise and implement new information systems. The three clear candidates for immediate change are: Pathology where modernisation programmes and new information systems planned. Radiology where, similarly to pathology, modernisation programmes and new information systems planned. Pharmacy / prescribing where there is an institutional push towards dm+d. 3.2 Stage 2 – Planned development Here we can take advantage of existing or planned use of clinical codes within a sector to consolidate the position. Welsh Clinical Portal. Adopt a ‘native’ set for information that is put onto the portal (see previous section). Primary care, consolidate around Read 2. Urgent care (Out of Hours and NHS Direct). Consolidate around Read 2 encoded records that are being extracted from Primary Care. Cancer care. Discuss options with cancer care community. As more information becomes available, we will add further sectors (e.g. elective care, networked care, specialist care). 3.3 Stage 3 – Review As sectors and domains coalesce around a limited number of common sets, it will be possible to assess the desirability of having a single national code set. The obvious candidate is Snomed CT which is intended to be global. Its history lies in primary care and pathology and it does have the expressive range to deal with complex fields such as histology, and the UK’s Clinical Terms contribution drew on a wide range of disciplines and domains. IHC will actively review the development and implementation of Snomed CT and support its evaluation. However, any move to a single set and the choice of that set should be based on a realistic assessment of actual clinical and organisational benefits of such a move, and not on abstract notions of the desirability of adopting what appears to be the future lingua franca. ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 24 of 29 4 Governance and decision making We are proposing a pragmatic programme, adapting to the needs and current situation of sectors and domains, but with the general thrust of rationalising the use of clinical codes across NHS Wales and encouraging the adoption of common code sets. The programme will collaborate with the Service ensuring that the choice of code sets and sub-sets are usable and safe. The governance process will require further development to ensure that the choices made will deliver enhanced safety and enable better information for all secondary uses. Governance and decision making will require close collaboration by The National Architecture Development Board (NADB) who determine those code sets which are required for the safe development and use of clinical systems. The Welsh Information Governance and Standards Board (WIGSB) who set standards for national reporting and corporate use of information. Professional bodies: such as Royal Colleges and specialist professional working groups. Will give advice on the suitability and usefulness of national code sets in their own clinical settings. We will consult and work with those who are undertaking developments such as Pathology Modernisation and accompanying system renewal and similar developments in Welsh Radiology. This will provide a pragmatic, practical way to bring a strategic perspective to the adoption of common code systems during these and other activities. Similarly, when the early adopter sites for the Welsh Clinical Portal have been chosen, Informing Healthcare and the NHS Wales development teams will assess and evaluate existing use of these systems and what needs to be done to support the portal. ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 25 of 29 5 Brief survey: NHS Wales and available coding systems 5.1 Coding systems currently in use in Wales There is such a variety of uses of coding systems around NHS Wales that it is impossible to survey and summarise it all. However, the summary given below helps to illustrate the present position. 5.1.1 Radiology Each radiology department has its own unique code set or set of recognised abbreviations. So, for example, the following as used by two different Trusts: BM 309 BASW BARIUM MEAL/SWALLOW BARIUM SWALLOW BARIUM SWALLOW Trust 1 Trust 1 Trust 2 5.1.2 Pathology Most pathology requests are sent to the lab as handwritten pro-formas attached to the sample(s). These are uncoded. The requests are then entered onto the laboratory systems (usually Telepath) where they are coded using a local coding system. There are as many local coding systems in use as there are local pathology departments. Branch Requesting Processing Reporting Microbiology None None None Biochemistry None None None Haematology None None None Cytology None Snomed RT None Histopathology None Snomed RT None Blood bank None None None Histology and cytology use M (morphology), T (topology) and E (aetiology) codes taken from Snomed RT. 5.1.3 Primary Care Apart from prescribing, primary care systems use Read 2 or, in a small number of cases (Healthysoft and Phoenix partnership), Clinical Terms Version 3 (CTV3). However, the use of the coding system varies between GP systems, meaning that care has to be taken even when using the same code sets. Primary care systems preponderantly use the First Databank (FDB) Multilex Drug File (MDF) for prescribing. These can be translated into Read 2 for export, although Read does not keep up with MDF and temporary codes sometimes need to be used. FDB is not implemented in Emis. Some GP systems are now using dm+d for prescribing. ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 26 of 29 5.1.4 Pharmacy Pharmacy primarily uses a range of local systems. There is a move, lead by the Prescription Pricing Authority in England, to move to dm+d. The NHSW Prescribing Services Unit also plans to adopt dm+d. All dm+d codes are supplied with a Snomed CT mapping. 5.1.5 Cancer Most Trusts in Wales use the Velindra ISCO/CANISC system that presently uses Read 2, ICD10 and OPCS4 for recording care, findings and procedures. They plan to migrate to CTV3 in the very near future. 5.2 Stock-in-trade, what is available 5.2.1 Applicability of coding systems There is no ubiquitous coding system that is applicable to all needs. Some, which are intended to be general, betray their origins and are better suited to certain clinical areas, and some are specifically designed for a specialised area. dm+d is intended for pharmacy. It arose out of the UKCPRS (UK Standard Clinical Products Reference Source). It is being adopted by the Prescription Pricing Authority in England (PPA) and probably by the Prescribing Services Unit (PSU) in Wales. Read 2 was developed from the original Read coding system by the Centre for Coding and Classification in England. The Read codes originate in primary care from their founder James Read, a GP. They are still heavily used in UK Primary Care, but also in some other areas. Bounded Code List for Pathology. This is a list of about 2,800 codes that are used for pathology reporting to GPs in England and Scotland. The Bounded list is a limited list of (Read coded) pathology investigations and results4. CTV3 - Clinical Terms Version 3. A further development and something of a departure from Read 2. Instead of the single hierarchy principle that Read 2 was based on, CTV3 uses multiple hierarchies, so allowing a code to inherit its characteristics from more than one source. Also CTV3 distinguishes between the concept and one or more possible terms for that concept, each of which has a code. CTV3 is also considerably richer than Read 2 having drawn widely on UK clinical disciplines. Snomed CT. The result of bringing together the US College of American Pathologists Snomed (Standard Nomenclature of Medicine) with the UK CTV3, thus combining pathology, primary care and CTV3’s richer set.. Snomed CT is intended to cover as wide a range of medicine as possible. ICD9 and 10. The International Classification of Diseases, endorsed by the WHO and used by WHO member states since 1994. ICD is used for reporting, public health and epidemiological analysis. Not generally considered to be suitable for direct clinical care. OPCS4. The Office of Population Censuses and Surveys Classification of Surgical Operations and Procedures. Developed for and used by the NHS for statistical purposes. Not generally considered to be suitable for direct clinical care. 4 Supporting a set of Read coded terms for use in pathology messaging, Robinson D, Holland M, Pill S., Journal of Informatics in Primary Care 2000 (February):8-11, http://www.primis.nhs.uk/informatics/feb2000/feb4.htm ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 27 of 29 LOINC (Logical Observation Identifiers Names and Codes) is a US coding system that primarily focuses on Laboratory. 5.2.2 Coding does not give us all the answers The Snomed CT code set gives five codes for ‘fundus’, related to the gall bladder, uterus, stomach, eye and abomasum (in ruminants). It gives two codes for aspirin as virtual and actual therapeutic agents. There is a code for Urea and Electrolytes (252167001), but not all U&E sets in Wales are the same. In older versions of Snomed there has been a code for hysterectomy that does not specify whether it includes removal of the cervix, causing some women to be removed from screening list when they still have a cervix (this appears to have been corrected in Snomed CT). The example shown below is taken from the authors of Clinical Terms Version 3 (CTV3) and shows how, even a fairly sophisticated, Snomed-like, system can be misleading unless care is taken. In the example, the term ‘cord compression’ is a shortening and a synonym of the preferred terms for both umbilical cord compression and spinal cord compression, clearly very different things. The concept for each (spinal and umbilical) is separately coded, but care must be taken to ensure that the preferred term is always shown in addition to a synonym. Read Code (CTV3) Term Preferred term / synonym Term-id X40Cc Umbilical cord compression Preferred term YaaGm X40Cc Cord compression Synonym Y40xj Xa0NK Spinal cord compression Preferred term Ya1XS Xa0NK Cord compression Synonym Y40xj The term alone does not provide all the required context. For example where a diagnostic code has been used as a header for a routine check-up, use of the code alone without the contextual information leaves the reader unable to distinguish check-up from primary diagnosis. There are many other pitfalls and inconsistencies in coding and they get more unpredictable and treacherous with the increasing sophistication of the coding system. These kinds of ambiguities are well understood by experts in the use of coding systems, but they could trap the inexperienced and unwary. 5.2.3 Mappings between code sets The table below gives our, incomplete, understanding of the possible mappings between code sets. Accurate, clinically safe, mappings between sets are difficult to do and the existence of a mapping should not be taken to indicate such safety. Rather, mappings can be used to provide management and research information and general guidance as to the clinical content of a record. The reference point must always be the original code assigned by the author of the information. ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 28 of 29 √ (nc) means that the result of the mapping cannot be used for direct clinical care. Mappings between Read 2 and CTV3 are between the Read 2 code and the equivalent CTV3 term. This is because CTV3 distinguishes between the concept (CTV3 code) and the term (CTV3 term and term code). Effectively CTV3 treats Read 2 codes as terms. ______________________________________________________________________________________________________ Migration to consistent use of coding and terminology in NHS Wales Page 29 of 29