Laryngologic Seminar
advertisement
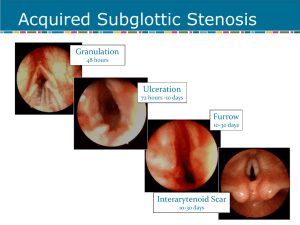
Laryngologic Seminar Mitomycin can reduce granuloma formation 2002-8-28 R3 KST Granuloma: mucosa injury release of plasma protein, blood cells, PLTs + TFs fibrin-fibronectin matrix, migration of capillaries, fibroblasts, inflammatory cells, fibroblast proliferation, formation of collagen & GAGs & fibronectin granulation tissues (about 1 week) collagen maturation, myofibroblast contraction (about 2 weeks) scar formation [6] Previous Mx: limited effects 1. Avoid mucosal injury/ cricothyroidectomy/ high tracheostomy 2. Avoid tube-free self retaining tracheostomy 3. Soft pliable, biocompatible stent /stoma tubes 4. antibiotics, anti-reflux agents 5. steroid (local, systemic) 6. cold humidification 7. penicillamine, beta-aminoproprionitrile, 5-FU, N-acetyl-L-cysteine: inhibit cross-linking of collagen/ scar formation Mitomycin: 1. An aminoglycoside from fungus Streptomyces caespitosus 2. alkylating antineoplastic agents: ssDNA breakage /C-G cross linking inhibit RNA and protein synthesis at higher dose (cytocidal) 3. Systemic form side effects: delayed bronchospasm/lung fibrosis, HUS, GI upset, HF, BM suppression etc. Mitomycin's effects on fibroblasts: 1. increased Fas-expression, small increase in Bax, Bcl-2, bcl-x, but increased apoptosis of fibroblast is not inhibited by Fas receptor blocker some Fas receptor signaling-independent pathway [1] 2. Inhibition of fibroblast proliferation, migration, ECM production, collagen formation by single exposure: but still some growth factors of fibroblast expression, ECM / some scar formation Animal model (dogs in UADT stenosis, rabbits in antrostomy/choanal atresia) 1. Vocal fold healing/ function: Negative consequences of topical MMC on vocal fold function: fewer fibroblasts and less collagen in Reinke’s spaces diminished mucosal wave [8] Microflap excision of mucosa + MMC, LVS before, 2 4 wks, manual adduction, air compressor air flow: 1 2. Laryngeal injury/stenosis: CO2 laser expose cartilage near CA joint1 + 1 % MMC: improved CAJ mobility, decreased granulation tissue, no 2nd vocal granuloma, No Cx [9] Suture arytenoid adduction, mobility by tensiometry 3. Subglottic/glottic stenosis: a. CO2 laser + MMC [10, 15]: decreased submucosal collagen, b. Suction of seretion reduce stenosis c. Repeat MMC days later: no further improvement of stenosis: Single topical use 4. Sinus antrostomies patency: a. Dose-related delayed closure of antrostomy and nasal mucosa healing. b. Ciliary function: initially impaired, normalized within 2 week after MMC, c. No Cx/ permanent microscopic changes, decrease posto stenosis. [11, 13] Clinical practice of mitomycin in reducing granuloma formation: 1. Clinical use: Dose and time-dependent inhibitory effects 2. Most clinical single topical use/studies: 0.1-0.4 mg/ml for 1-5 mins in Grade 0-2 laryngotracheal stenosis 3. Higher dose (e.g.1 mg/ml): cytocidal effect on fibroblast In Ophthalmology: 1. Pterygium: 1st use by Kunitomo and Mori, decrease recurrence: 88% to 2~3% 2. trabecular patency: in glaucoma surgery 3. NLD patency: after DCR 4. Optic nerve sheath fenestration 5. Strasbismus Reported complications: 1. 2nd glaucoma/cataract, scleral/corneal ulceration, scleromalacia, symblepharon, calcification, iritis, ocular hypotonia, decreased wound healing infections, 2. Most single topical use is safe: 0.02 % (0.2 mg/ml) for 5 mins, 0.04% for 3 mins: No significant different effects of fibroblast inhibition. In ENT fields: 1. myringotomy: longer patency 2. Glottic, subglottic, tracheal, hypopharyngeal stenosis +/- LTR or CTR: Endoscopic CO2 laser radial incision+ dilatation+ topical MMC (93%): 14/15 improvement of airway and preoperative symptoms, no complication, e.g. Wegner’s granulomatosis [3] [4, 1st use] [5] [6] 2 Against [12] Subglottic or upper tracheal stenosis s/p LTR: topical MMC at the time of extubation or stent removal, No difference in MMC (+) or N/S groups in stenosis distribution 3. Esophageal stenosis: dilatation+ MMC: minor improvement [6] 4. Choanal atresia: (e.g. CHARGE, VACTERL syndrome) s/p endoscopic drillout, transnasal: unilateral+ some bilateral, some transpalatal, +/postoperative stenting: Msot open decrease need for stenting, dilatations, revision surgery [6, 14] In surgery: 1. Abdominal adhesionalysis: bush cecum and peritoneum induce + laparoscpic MMC 10 days later [2] 2. bilateral bronchial necrosis: a. Restenosis despite Argon-laser, stentin, dilatation many times in cystic fibrosis s/p bilateral lung transplantation b. Open after endoscopic dilatation and stenting + MMC [7] Ischemia induced donor lung infection, bronchomalacia, granuloma Possible applications: (before possible granuloma formation or after removal) 1. In prolonged intubation, tracheostomy, airway trauma at surgery. 2. Before airway stent, while changed, 3. Following dilatation/ laser surgery for UADT stenosis 4. Autoimmune/Granulomatous diseases: Wegner’s granulomatosis, sarcoidosis etc. 5. ? slow-release form over stenting 6. No data indicating what conc., duration, frequency of application of MMC is more efficacious, e.g. in UADT stenosis 3 References: 1. Crowston JG, Chang LH, Constable PH, et al. Apoptosis gene expression and death receptor signaling in mitomycin-C-treated human tenon capsule fibroblasts. Invest Ophthalmol Vis Sci 2002;43:692-9 2. Cubukcu A, Alponat A, Gonullu NN, et al. An experimental study evaluating the effect of Mitomycin C on the prevention of postoperative intraabdominal adhesions. J Surg Res 2001;96:163-6 3. Rahbar R, Shapshay SM, Healy GB, et al. Mitomycin: effects on laryngeal and tracheal stenosis, benefits, and complications. Ann ORL 2001;110:1-6 4. Rahbar R, Valdez TA, Shapshay SM, et al. Preliminary results of intraoperative mitomycin-C in the treatment and prevention of glottic and subglottic stenosis. J Voice 2000;14:282-6 5. Ward RF, April MM. Mitomycin-C in the treatment of tracheal cicatrix after tracheal reconstruction Int J Ped Otorhinolaryngol 1998;44:221-6 6. Rahbar R, Jones DT, Nuss RC, et al. The role of mitomycin in the prevention and treatment of scar formation in the pediatric aerodigestive tract: friend or foe? Arch Otolaryngol Head Neck Surg 2002;128:401-6 7. Erard AC, Monnier P, Spiliopoulos A, et al. Mitomycin C for control of recurrent bronchial stenosis: a case report. Chest. 2001;120:2103-5 8. Garrett CG, Soto J, Riddick J, et al. Effect of mitomycin-C on vocal fold healing in a canine model Ann ORL 2001;110:25-30 9. Spector JE, Werkhaven JA, Spector NC, et al. Preservation of function and histologic appearance in the injured glottis with topical mitomycin-C. Laryngoscope. 1999;109:1125-9 10. Correa AJ, Reinisch L, Sanders DL, et al. Inhibition of subglottic stenosis with mitomycin-C in the canine model. Ann ORL 1999;108:1053-60 11. Rahal A, Peloquin L, Ahmarani C. Mitomycin C in sinus surgery: preliminary results in a rabbit model. J Otolaryngol 2001;30(1):1-5 12. Hartnick CJ, Hartley BE, Lacy PD, et al. Topical mitomycin application after laryngotracheal reconstruction: a randomized, double-blind, placebo-controlled trial. Arch Otolaryngol Head Neck Surg 2001;127:1260-4 13. Ingrams DR, Volk MS, Biesman BS, et al. Sinus surgery: does mitomycin C reduce stenosis? Laryngoscope 1998;108:883-6 14. Prasad M, Ward RF, April MM, et al. Topical mitomycin as an adjunct to chanal atresia repair. Arch Otolaryngol Head Neck Surg 2002;128:398-400 15. Elishar R, Eliachar I, Esclamado R, et al. Can topical mitomycin prevent laryngotracheal stenosis ? laryngoscope. 1999;109:1594-1600 16. Occleston NL, Daniels JT, Tarnuzzer RW, et al. Single exposure to antiproliferatives: long-term effects on ocular fibroblast wound-healing behavior. Invest Opthalmol Vis Sci. 1997;10:1998-2007 4