Slide 1 - Dayton Children`s Hospital
advertisement

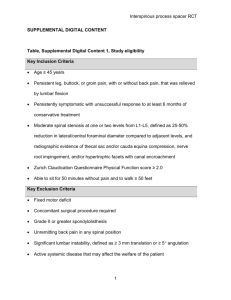
Acquired Subglottic Stenosis Granulation 48 hours Ulceration 72 hours -10 days Furrow 10-30 days Interarytenoid Scar 10-30 days Acquired Subglottic Stenosis Pathogenesis • Intrinsic Factors: o Shape and size of larynx o Infection o Wound healing o Malnutrition o Chronic Disease o Activity/ movement o GERD/ LPR • Extrinsic Factors: oEndotracheal tube • Size • Traumatic intubation/ Multiple reintubations • Duration of intubation oTracheostomy oNasogastric Tube trauma • Chronic inflammation will exacerbate changes induced by ETT • Higher rate of GER in patients with SGS than the general population Gould SJ, Young M. Sublgottic ulceration and healing following endotracheal tube intubation in the neonate. Annals ORL; 1992, 101: 815. Acquired Subglottic Stenosis Pathogenesis • Endotracheal Tube Factors: o Size of ETT • < 20 cm H2O pressure air leak appropriate o ETT material • Silicone or Polyvinyl chloride tubes safest o Duration of Intubation • Adults <7-10 days • Longer for premature infants o Shearing motion of ETT • Increased trauma to mucosa Increases traumatic changes o Maintenance and care of ETT and patient • Aggressive suctioning, endoscopy, reintubation Subglottic Stenosis Cotton Myer Grading System Myer CM, O’Connor DM, Coton RT. Proposed grading system for subglottic stenosis based on endotracheal tube sizes. Ann Otol Rhinol Laryngol, 1994; 103: 319-323. Grading Subglottic Stenosis ETT Size Patient Age Premature No Detectable Lumen 0-3 ½ mos 3 ½- 9 ½ mos 9 ½- 2 yrs 2 yrs 4 yrs 6 yrs Grade IV 2.0 2.5 3.0 3.5 4.0 4.5 5.0 5.5 40 58 68 75 80 84 86 89 30 48 59 67 74 78 81 26 41 53 62 68 73 22 38 50 57 64 20 35 45 54 19 32 43 17 30 16 Grade III Grade II Grade I 6.0 Subglottic Stenosis Grade I: <50% Stenosis Grade II: 50-70% Stenosis Grade III: 70-99% Stenosis Grade IV: No Detectable Lumen Subglottic Stenosis- Treatment • Grade I and low Grade II o Can usually be observed o Close follow up, endoscopy for surveillance • High Grade II o May require surgical repair o Endoscopic dilation o Open surgical repair • Grade III and IV o Require surgical repair o Open surgical repair o Tracheostomy as temporizing measure Surgical Treatment- Dilation Anterior Cricoid Split • Described in 1980 by Cotton as alternative to tracheostomy for patients with acquired subglottic stenosis • Patient selection: o o o o > 2 failed extubations due to SGS Weight >1500 grams Off ventilator support for 10 days <30% O2 requirement • Airway improved by: o Improved circulation to the cricoid and decreased edema o Opening the cricoid allows it to “spring open” Laryngotracheal Reconstruction • Anterior Graft o Use for lower grade and primarily anterior stenoses • Anterior and Posterior Grafts o Use for posterior glottic stenosis, circumferential stenosis, or near total/ total subglottic stenosis Single Stage Laryngotracheal Reconstruction • Traditional LTR with cartilage grafts and simultaneous tracheal decannulation • Indications: o o o o SGS without associated tracheal stenosis or tracheomalacia Weight greater than 4 kg Gestational age > 30 weeks No craniofacial or vertebral anomalies • Aim to avoid complications of long term stenting and tracheostomy • Postoperative care critical! o Nasotracheal tube “stenting” o Titrated sedation versus Paralysis “Mini” Laryngotracheal Reconstruction • Anterior cricoid split with thyroid ala cartilage graft • Small retrospective series show shortened operative time compared with costal cartilage graft and no significant difference in operative outcomes • Expands the age group for LTR to younger patients Endoscopic Posterior Cricoid Split • Described by Inglis et al in 2003 for management of posterior glottic stenosis with or without subglottic stenosis o 5/ 7 children decannulated within a year after surgery • Posterior cricoid lamina is endoscopically divided and expanded with a costal cartilage graft Inglis AF, Perkins JA, Manning SC, Mouzakes J. Endoscopic posterior cricoid split and rib grafting in 10 children. Laryngoscope 2003; 113(11):2004-2009. Conclusions • The most common causes of congenital stridor include laryngomalacia, subglottic stenosis. o Tracheomalacia is the most common cause of lower airway stridor, however is much less common than laryngomalacia • Diagnostic work up should include careful history and physical examination. o Office laryngoscopy and/ or direct laryngoscopy and bronchoscopy should be used to make definitive diagnosis • Many congenital airway lesions can be treated expectantly or medically • Surgical treatment options are available, and should be tailored to the individual patient. Thank You! http://www.nationwidechildrens.org/ear-nose-throat Fundraising Driving Online Interaction and Giving