Prevalence of common microbes and pattern of their antibiotic
advertisement

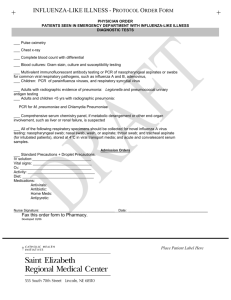
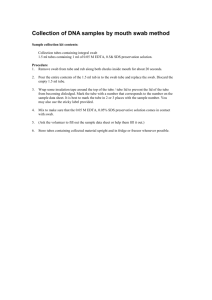
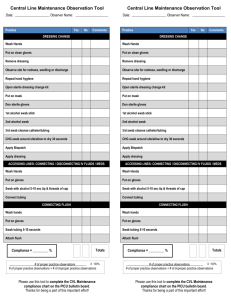
EL-MINIA MED. BULL. VOL. 21, NO. 2, JUNE, 2010 Eldydamouny et al PREVALENCE OF COMMON MICROBES AND PATTERN OF THEIR ANTIBIOTIC SENSITIVITY AND RESISTANCE IN TABUK, SAUDI ARABIA By Mohamad Aly Eldydamouny, *M.D., ** Kazmi Rashed Sayed, M.S. *** Ghada Osman, M.D. and****Ashraf A. Ewis *Consultant of Public Health, Infection Control Program, General Directorate of Health Affairs in Tabuk Region, Tabuk, Kingdom of Saudi Arabia **Microbiologist King Fahad Hospital, Tabuk, Kingdom of Saudi Arabia ***Specialist of Public Health, King Khalid Hospital, Tabuk, Kingdom of Saudi Arabia and ****Dept. of Infection Control & Public Health, Faculty of Medicine, El-Minia University, El-Minia, Egypt ABSTRACT: Objective: The study was aimed to identify common prevalent strains of microorganisms causing infection in Tabuk Region, Saudi Arabia, and to detect their antimicrobial sensitivity and resistance pattern against locally available commonly used antibiotics. Materials and Methods: A total of 2423 culture positive laboratory samples from four main hospitals in Tabuk province were included in this descriptive cross sectional study. The samples were cultured in appropriate media using standard microbiological procedures to identify the microbes. Antibiotic sensitivity and resistance pattern were determined using the Kirby-Bauer disk diffusion method. Sensitivity more than 70% for an antibiotic was regarded as ‘effective’ against the particular microbe. Results: Of 2423 culture positive sample-giver patients, Saudis (84.5%), females (68.6%), and hospitalized patients (64.1%) were predominant. The age of the patients ranged from 1 day to 100 years with a mean of 32.55 ± 27.12 years. Among the samples, the most common variety was high vaginal swab (27.8%), followed by urine (17.9%), wound swab (17%), throat swab (9.4%), sputum (5.2%), ear swab (5%), blood (4.5%), umbilical swab (3.2%), and others. Klebsiella (22.3%) was found as the most prevalent micro-organism, while other identified main microbes were Escherichia coli (20.1%), Staphylococcus aureus (15.1%), Pseudomonas (13.7%), Streptococci (5.7%), Proteus (5.3%), and MRSA (2.8%). Among 595 Staphylococcus-positive samples, Staphylococcus aurius (61.7%) was found as the most prevalent one, followed by MRSA (11.6%), Staphylococcus epidermidis (7.4%), Staphylococcus albus (7.2%), Coagulage negative Staphylococcus (7.1%), and others. Staphylococcus aurius was also predominant among the gram positive samples (n=717), and it was found more in high vaginal swab (79.3%), nasal swab (65%), umbilical swab (61.9%), ear swab (55.2%), wound swab (53.5%), and urine (50.5%). Among the gram negative samples (n=1683), Klebsiella was the most prevalent organism, and it was found mainly in throat swab (70.3%), samples from axilla (57.1%), and umbilical swab (52.6%). Amoxicillin was found as 100% sensitive for Staphylocococcus aurius and E. coli infection, while Ceftriaxone had the same sensitivity pattern against MRSA infection. Amikacin was found sensitive against E. coli (93.9%), Klebsiella (88.9%), Pseudomonas (85.2%), Streptococcus (83.3%), and MRSA (72.7%). Ciprofloxacin was also found sensitive against Klebsiella (89%), Pseudomonas (78.1%), and E. coli (72.6%). Gentamycin was found effective against Klebsiella (81.1%), E. coli (80.5%), Staphylococcus aurius (79.2%), MRSA (76.7%), 257 EL-MINIA MED. BULL. VOL. 21, NO. 2, JUNE, 2010 Eldydamouny et al and Pseudomonas (75.1%). Cefotaxime and Ceftriaxone both were found effective against Streptococcus, E. coli, and Klebsiella. Ampicillin showed the highest resistance pattern against all the top prevalent gram positive and gram negative microbes indicating its general ineffectiveness. Moreover, Cotrimoxazole was found as ineffective against all top three gram negative micro-organisms. Conclusion: Our study found considerably higher occurrence of antibiotic resistance in Tabuk province emphasizing the need for local and country-based surveillance to characterize and monitor the infectious agents, and to develop strategies that would improve the pattern of treatment and control of infection. KEY WORDS: Antibiotic Sensitivity Micro organisms Resistance Infection control expensive to treat. Antibiotic resistant bacteria can cause harm for the patients who suffer from common infections that once could be cured by antibiotics but now has become difficult or impossible to treat.2,3 A recently-discovered strain of Staphylococcus bacteria does not respond to antibiotic treatments at all, leading medical analysts to worry that certain 'super bugs' could emerge that are resistant to even the most potent drugs, rendering some infections incurable.5 INTRODUCTION: Now a days, antibiotic resistance has become a serious health problem worldwide, and United States Centre for Disease Control and Prevention (CDC) calls antibiotic resistance one of its 'top concerns'.1 This is because over the last decade, almost every type of bacteria has become stronger and less responsive to antibiotic treatment when it is really needed. Whenever an antibiotic is used for treatment it promotes the development of antibiotic resistant bacteria. As a consequence when a person takes antibiotics, sensitive bacteria are killed, but resistant germs may survive and continue to multiply causing more harm.2,3 The number of infection caused by resistant pathogens continues to increase in Saudi Arabia like other parts of the world. These infections cause suffering, inability and death, imposing an enormous financial burden on both healthcare systems and on the society in general, because of direct costs due to prolongation of illness and treatment in hospital, indirect costs due to loss of productivity, and societal costs due to morbidity and mortality. This is likely to lead to already-scarce healthcare resources being diverted to infection control efforts, and will have long-term implications due to loss of confidence in the medical profession and in the public healthcare delivery system provided or regulated by Factors contributing towards antibiotic resistance include overuse of broad-spectrum antibiotics, incorrect diagnosis, unnecessary prescriptions, improper use of antibiotics by patients, the impregnation of household items and children's toys with low levels of antibiotics, and the use of antibiotics as livestock food additives for growth promotion.4 Antibiotic resistant bacteria can quickly spread among family members, schoolmates and coworkers, providing opportunity to rise emerging infectious diseases those are more difficult to cure and more 258 EL-MINIA MED. BULL. VOL. 21, NO. 2, JUNE, 2010 governments.6,7 Eldydamouny et al The samples were collected in aseptic condition and cultured in incubator at 37o C for at least 72 hours. The culture was performed in appropriate media using standard microbiological techniques in order to identify the micro-organisms. Gramstaining for isolated microbes were done when and where necessary before proceeding to test for their antibiotic sensitivity and resistance. Kirby-Bauer disk diffusion method was used to determine antibiotic sensitivity and resistance pattern. Sensitivity more than 70% for an antibiotic was considered as ‘effective’ against the respective microbe. Complete aseptic environment was ensured in each laboratory, and highly skilled and experienced staffs performed the entire procedure. Surveillance for hospital acquired infection and conducting research on local antibiogram are always the key strategies for hospital infection control program. Several studies8,9,10 have confirmed that the way of this evidence based practice has been implemented in many standardized hospitals in developed world. We carried out this study to identify prevalent strains of bacterial pathogens causing infection in Tabuk Region, Saudi Arabia, and to determine their antimicrobial sensitivity and resistance pattern against locally available widely used antibiotics. MATERIALS AND METHODS: This descriptive cross sectional study was conducted during a period between 1st January to 31st December, 2008 in Tabuk province which is located along the North-Western part of Saudi Arabia near the Red Sea. Tabuk province possesses a surface area of 108,000 sq km occupied by 573,691 populations according to the KSA Census 2010 (Preliminary results). It consists of five 'Governorates' (Umluj, Duba, Al-Wajh, Haqel and Tayma'a) and one 'Cluster' (Al-Bada). Data were collected from laboratory result sheets and registers using a preformed unified checklist applicable to all study-hospitals. The collected data included information on socio-demographic features of the sample-givers, type and source of tested samples, test results, sensitivity and resistance pattern to commonly used antibiotics. The collected data were undergone several processes such as data cleaning, check for missing values, coding and recoding of variables before they were entered into SPSS (Statistical Package for Social Sciences) version 12 for appropriate statistical analysis. A total of 2423 culture positive laboratory samples from four main hospitals in the province titled: Tabuk Maternity and Children's Hospital, AlWajah hospital, King Khaled Hospital, and King Fahad Hospital) were included in the study. Among nine general hospitals in the province, above-mentioned four hospitals were selected because workingmicrobiologists were available in the laboratories of those hospitals during the study. RESULTS: Table 1 shows the distribution of culture positive laboratory samples by hospital, sex, nationality and source of collection. Of total 2423 culture positive laboratory samples, the highest proportion (41.2%) were from Tabuk Maternity and Children’s Hospital (MCH), followed by 24.2% from Al-Wajh Hospital, 19.9% from 259 EL-MINIA MED. BULL. VOL. 21, NO. 2, JUNE, 2010 King Fahad Hospital (KFH), and the least (14.7%) from King Khaled Hospital (KKH). Most of the culture positive laboratory samples were received from Saudis (84.5%) and females (68.6%). The age of samplegiver patients ranged widely from 1 day to 100 years with a mean age of 32.55 ± 27.12 years. Maximum (64.1%) samples were received from hospitalized patients, while remaining 35.9% were collected from outpatient departments. Figure 1 illustrates the seasonal variation of culture positive laboratory samples by months in the year 2008. Of 2423 samples, 11.4% were collected in the month of Rabi Al Awwal which is quite higher than the samples received in other months. However, the lowest proportion (5.7%) of the culture positive laboratory samples was received in the month of Ramadan. Eldydamouny et al total of nine varieties of Staphylococci strains were isolated from the culture positive laboratory samples [Figure 4]. Among the total 595 Staphylococcuspositive samples, Staphylococcus aurius (61.7%) was found as the most prevalent one, followed by MRSA (11.6%), Staphylococcus epidermidis (7.4%), Staphylococcus albus (7.2%), Coagulage negative Staphylococcus (7.1%), and others [Figure 4]. Of the culture positive laboratory samples, gram positive organisms were found in 717 (29.9%) samples, while gram negative organisms were isolated from 1683 (70.1%) samples. Among the samples those showed gram positive microbes (n=717), Staphylococcus aurius was predominant and it was found highest in high vaginal swab (79.3%), followed by in nasal swab (65%), umbilical swab (61.9%), ear swab (55.2%), wound swab (53.5%), and urine (50.5%) [Table 2]. Streptococci were found higher in samples from axilla (66.7%), sputum (60.3%), and throat swab (50%), while MRSA were found in samples from axilla (33.3%) and nasal swab (25%) [Table 2]. Klebsiella, Escherichia coli and Pseudomonas predominated among the samples those showed gram negative microbes (n=1683). Klebsiella was found more in throat swab (70.3%), samples from axilla (57.1%), and umbilical wound swab (52.6%) [Table 3]. Escherichia coli was found highest in urine (47%), whereas Pseudomonas were plenty in rectal swab (72.7%), eye swab (47.1%), and wound swab (35%) [Table 3]. Figure 2 shows the distribution of culture positive laboratory samples by their type and nature. Of total 2423 samples, the most common variety was high vaginal swab (27.8%), while the proportion of urine sample (17.9%) and wound swab (17%) were nearly equal. Throat swab (9.4%), sputum (5.2%), ear swab (5%), blood (4.5%), and umbilical wound swab (3.2%) were also included in culture positive samples. Moreover, samples from NG tube tip, nasal swab, eye swab, samples from axilla, and rectal swab played important role to identify prevalent organisms irrespective of their total numbers. Klebsiella (22.3%) was found as the most prevalent micro-organism among 2423 culture positive laboratory samples, followed by Escherichia coli (20.1%), Staphylococcus aureus (15.1%), Pseudomonas (13.7%), Streptococci (5.7%), Proteus (5.3%), MRSA (2.8%), and so on [Figure 3]. A Sensitivity and resistance pattern of the locally available antibiotics against top three prevalent gram positive and gram negative microbes has been shown in Table 2 and Table 3. Effectiveness of these 260 EL-MINIA MED. BULL. VOL. 21, NO. 2, JUNE, 2010 antibiotics can be explained by their sensitivity and resistance pattern. Amoxicillin was found as 100% effective for Staphylocococcus aurius and E. coli infection, whereas Ceftriaxone had the same effectiveness against MRSA infection. Amikacin was found effective against E. coli (93.9%), Klebsiella (88.9%), Pseudomonas (85.2%), Streptococcus (83.3%), and MRSA (72.7%). Ciprofloxacin was also found effective against Klebsiella (89%), Pseudomonas (78.1%), and E. coli (72.6%). Gentamycin was found effective against Klebsiella (81.1%), E. coli (80.5%), Staphylococcus aurius Eldydamouny et al (79.2%), MRSA (76.7%), and Pseudomonas (75.1%). Cefotaxime and Ceftriaxone both were found effective against Streptococcus, E. coli, and Klebsiella. Ampicillin appeared as the most ineffective antibiotic to fight against all the top prevalent gram positive and gram negative microbes shown in Table 2 and Table 3. Similarly, Cotrimoxazole was also found as ineffective against all top three gram negative micro-organisms [Table 3]. Moreover, Salmonella was found 100% resistant to Amikacin, Ampicillin, Augmentin, Cephalothin, Cotrimoxazole and Gentamycin [Data not shown in the tables]. Table 1: Distribution of culture positive laboratory samples by hospital, sex, nationality and source of collection, Tabuk, Saudi Arabia, 2008 Variable Hospital (n=2423) Sex (n=2215)a Nationality (n=795)b Source of sample collection (n=2084)c Category Maternity and Children's Hospital (MCH) Al-Wajh Hospital King Fahd Hospital (KFH) King Khaled Hospital (KKH) Male Female Saudi Non-Saudi Admitted patient at indoor Non-admitted patient at outdoor a Frequency (%) 998 (41.2%) 586 (24.2%) 483 (19.9%) 356 (14.7%) 696 (31.4%) 1519 (68.6%) 672 (84.5%) 123 (15.5%) 1335 (64.1%) 749 (35.9%) Sex was unknown for 208 (8.6%) samples due to unavailability of data Nationality was unknown for 1628 (67.2%) samples due to unavailability of data c Source of sample collection was unknown for 339 (14%) samples due to unavailability of data b 261 EL-MINIA MED. BULL. VOL. 21, NO. 2, JUNE, 2010 Eldydamouny et al Figure 1: Seasonal variation of culture positive laboratory samples (n=2423) by months, Tabuk, Saudi Arabia, 2008 Figure 2: Distribution of culture positive laboratory samples (n=2423) by their type, Tabuk, Saudi Arabia, 2008 * Others (3.3%) include stool, pus from abscess, pleural fluid, sample from skin, sample from CVL tip, prostatic discharge, semen, swab from bed sore, urethral discharge, breast nipple discharge, etc. 262 EL-MINIA MED. BULL. VOL. 21, NO. 2, JUNE, 2010 Eldydamouny et al Figure 3: Micro-organisms isolated from culture positive laboratory samples (n=2423), Tabuk, Saudi Arabia, 2008 25.0 22.3 20.1 Percent 20.0 15.1 15.0 13.7 10.0 5.7 5.3 5.0 2.8 2.5 4.1 1.8 1.8 1.7 1.5 1.5 0.0 * Streptococci (5.7%) include Streptococcus Beta-haemolyticus, Streptococcus pneumonae, Streptococcus viridance, etc. ** Others (4.1%) include Staphylococcus haemolyticus, E. cloacae, E. fecalis, Staphylococcus cohnii, Raoultella ornithinolytica, Yersina pestis, Salmonella, Citrobacter fraundii, Micrococcus, Pantoea, Morganella morganii, Diplo viridance, etc. Figure 4: Different strains of Staphylococci (n=595) isolated from culture positive laboratory samples, Tabuk, Saudi Arabia, 2008 70.0 61.7 Percent 60.0 50.0 40.0 30.0 20.0 10.0 11.6 7.4 7.2 0.0 263 7.1 3.0 1.0 0.7 0.3 EL-MINIA MED. BULL. VOL. 21, NO. 2, JUNE, 2010 Eldydamouny et al Table 2: Top three prevalent gram positive microbes by nature of laboratory sample, antibiotic sensitivity and resistance pattern, Tabuk, Saudi Arabia, 2008 Gram positive microbes Nature of laboratory sample High vaginal swab Nasal swab 1.Staphylococcus Umbilical swab aurius Ear swab Wound swab Urine Sample from axilla Sputum 2. Streptococcus Throat swab Eye swab Urine Ear swab Sample from axilla Nasal swab 3. MRSA Sample from ET/NGT tip Wound swab Sputum Eye swab Percentage* Antibiotic sensitivity Percentage* Antibiotic resistance Percentage* 79.3% 65.0% 61.9% 55.2% 53.5% 50.5% 66.7% 60.3% 50.0% 21.4% 15.5% 12.1% 33.3% 25.0% 21.4% Amoxycillin Vancomycin Gentamycin Ceftriaxone Augmentin Amikacin Cefoxitin Vancomycin Ceftriaxone Amikacin Augmentin Cefotaxime Ceftriaxone Vancomycin Bacitracin 100% 82.7% 79.2% 69.7% 65.7% 64.8% 88.9% 85.9% 84.6% 83.3% 82.3% 75.0% 100.0% 97.1% 92.9% Ampicillin Cotrimoxazole Cephalothin Nalidixic Acid Bacitracin Aztreonam Ampicillin Polimixin B Cotrimoxazole Aztreonam Ciprofloxacin Cephalothin Polimixin B Ampicillin Nalidixic Acid 74.5% 58.2% 54.3% 53.2% 53.1% 52.1% 68.9% 68.4% 65.5% 47.5% 46.9% 46.6% 80.0% 78.0% 54.5% 14.3% 9.5% 7.1% Gentamycin Ceftazidime Amikacin 76.7% 75.0% 72.7% Cotrimoxazole Augmentin Aztreonam 50.0% 50.0% 47.8% *Percentage of total number of samples those showed gram positive microbes (n=717) after laboratory test 264 EL-MINIA MED. BULL. VOL. 21, NO. 2, JUNE, 2010 Eldydamouny et al Table 3: Top three prevalent gram negative microbes by nature of laboratory sample, antibiotic sensitivity and resistance pattern, Tabuk, Saudi Arabia, 2008 Gram negative microbes Nature of laboratory sample Throat swab Sample from 1. Klebsiella axilla Umbilical swab Blood High vaginal swab Ear swab Urine High vaginal 2. swab Escherichia Sputum coli Nasal swab Wound swab Ear swab Rectal swab Eye swab 3. Wound swab Pseudomonas Sputum Sample from ET/NGT tip Ear swab Percentage* Antibiotic sensitivity Percentage* Antibiotic resistance Percentage* 70.3% 57.1% Ciprofloxacin Amikacin 89.0% 88.9% Ampicillin Cotrimoxazole 80.2% 64.4% 52.6% 44.6% 35.0% Amoxycillin Gentamycin Cefotaxime 85.7% 81.1% 72.4% Cephalothin Vancomycin Aztreonam 58.3% 55.2% 52.8% 33.8% 47.0% 33.2% Ceftriaxone Amoxycillin Amikacin 71.1% 100% 93.9% Bacitracin Ampicillin Cotrimoxazole 52.5% 76.0% 69.9% 26.6% 23.5% 22.8% 20.0% 72.7% 47.1% 35.0% 34.4% 33.3% Gentamycin Cefotaxime Ceftriaxone Ciprofloxacin Amikacin Ciprofloxacin Gentamycin Bacitracin 80.5% 77.6% 76.7% 72.6% 85.2% 78.1% 75.1% 69.6% Cephalothin Polimixin B Nalidixic Acid Aztreonam Ampicillin Cotrimoxazole Cephalothin Vancomycin Augmentin 59.4% 57.1% 45.3% 42.8% 83.3% 75.5% 69.1% 64.4% 52.8% Polimixin B 50.0% 29.2% *Percentage of total number of samples those showed gram negative microbes (n=1683) after laboratory test 265 EL-MINIA MED. BULL. VOL. 21, NO. 2, JUNE, 2010 Eldydamouny et al Antibiotics are considered as the essential drugs prescribed by the physicians to treat infections, although existing antibiotics are losing their effect at an alarming pace, day by day. In one study, fluoroquinolones were clearly associated with Clostridium difficile infection, which is a leading cause of nosocomial diarrhoea and a major cause of death, worldwide.11 Modern medicine could be seriously threatened if antibiotic resistance is not tackled urgently. DISCUSSION: In our study, maximum (64.1%) samples were received from hospitalized patients, while remaining 35.9% were collected from the outpatients. Source of the sample can give an idea about whether the infection is community acquired or associated with staying in hospital, although confirmation depends upon other clinical and laboratory findings of patient. Our study revealed that the lowest proportion (5.7%) of the total culture positive laboratory samples was received in the holy month of Ramadan, indicating the usual declining number of treatment seeking patients in the study hospitals for being ‘day time fasting’ during this month. Rational use of antibiotics may reduce the chance of development of opportunistic infections by antibioticresistant bacteria. Moreover, selection of the appropriate antibiotic that would target the particular causative pathogen, avoiding antibiotic for a viral infection such as common cold or flu, taking antibiotics only according to the physician’s prescription, not by the patients themselves, might be the ways to prevent antibiotic resistance.2,4 Our study findings showed a similarity with several previous studies11,12,13,14, where increased presence of gram negative bacilli were found in respiratory, urinary tract, and gastro-urinary infections. In our study, Klebsiella, Escherichia coli, and Pseudomonas were found respectively more in throat swab, urine, and rectal swab [Table 3]. This study also revealed similar results in relation to sensitivity and resistance pattern of the antibiotics against different gram positive and gram negative microbes as mentioned in several studies15,16,17,18 conducted previously. Ampicillin appeared as the most out of date antibiotic in this study, which is analogous to the results shown in a number of earlier studies11,12,13,14. The rate of Cotrimoxazole resistance against E. coli was found more than 20% in a study conducted in 19964, which was found almost 70% in our study. However, Cotrimoxazole was found least effective against nearly all strains of Staphylococcus and Streptococcus in our study. Our study finding in relation to the antibiotic resistance warns us to take immediate steps to tackle the situation for microbial resistance. The inevitable fact is that effective antibiotics may not be available to treat seriously ill patients in the near future, if the situation continues like this.15 Acknowledgement The authors acknowledge the remarkable contribution of Dr. Naela Ali Diab, (Microbiologist, Maternity and Child Hospital, Tabuk, KSA). She initiated this study and without her great effort it was not possible to be completed. We would like to thank Mr. Bander Ghabban (Alwajh Hospital, KSA) for his tremendous help and cordial cooperation in data 266 EL-MINIA MED. BULL. VOL. 21, NO. 2, JUNE, 2010 collection. We also acknowledge the significant contribution made by Dr. M. Al Mamun (Public Health Specialist Physician, Department of Primary Health Care and Preventive Medicine, General Directorate of Health Affairs in Tabuk Region, Tabuk, KSA), who thoroughly revised and edited the full manuscript. Eldydamouny et al patient outcomes: Mortality, length of hospital stay, and health care costs. Clin Infect Dis ‘06; 42: 82-89. 8. French, GL. Closing the loop: audit in infection control. J Hosp Infect. 1993;24:301–308. doi: 10.1016/ 0195-6701(93)90062-5. 9. Pellowe, CM; Pratt, RJ; Harper, P; et al; Guideline Development Group. Prevention of healthcare-associated infections in primary and community care. J Hosp Infect. 2003;55:S5–S127. 10. Hay, A. Audit in infection control. J Hosp Infect. 2006;62:270– 277. doi: 10.1016/j.jhin.2005.09.008. 11. McCusker ME, Harris AD, Perencevich E, Roghmann MC (2003). Fluoroquinolone use and Clostridium difficile-associated diarrhea. Emerging Infect. Dis. 9 (6): 730–3. 12. Frost F, Craun GF, Calderon RL (1998). Increasing hospitalization and death possibly due to Clostridium difficile diarrheal disease. Emerging Infect. Dis. 4 (4): 619–25. 13. Centers for Disease Control and Prevention; retrieved from http://www.cdc.gov/ncidod/eid/vol4no4/ frost.htm 14. Kahler J, Acute Infectious Diarrhea. Department of Emergency Medicine, University of Michigan Health System, Ann Arbor, MI. 15. Scheetz, marc h.; hurt, kristin m. et al. Applying antimicrobial pharmacodynamics to resistant gramnegative pathogens. American Journal of Health-System Pharmacy. 63(14): 1346-1360, July 15, 2006. REFERENCES: 1. West L; Antibiotic Resistance is Becoming a Serious Health Issue; retrieved from http://environment. about.com/od/healthenvironment/a/sup erbugs.htm 2. Gupta R. Antibiotic Resistant Bacteria; retrieved from http:// www. buzzle.com/articles/antibiotic-resistantbacteria.html 3. Ranji SR, Steinman MA, Shojania KG, Gonzales R. Interventions to Reduce Unnecessary Antibiotic Prescribing. A Systematic Review and Quantitative Analysis. Med Care 2008;46:847-862. 4. Antibiotic resistance; retrieved from http://www.sciencedaily.com/ articles/a/antibiotic_resistance.htm 5. Mestres H. Why do modern bacteria "resist" antibiotics, confounding medical treatment? Seattle, WA. Retrieved from www. Keepantibioticsworking.com 6. Cosgrove S, Carmeli Y. The impact of antimicrobial resistance on health and economic outcomes. Clin Infect Dis 2003; 36: 1433-1437. 7. Cosgrove S. The relationship between antimicrobial resistance and 267