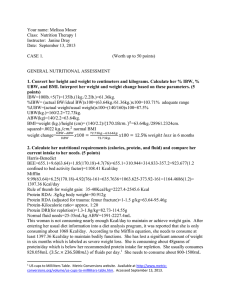
NUTRITION ASSESSMENT
advertisement

NUTRITION ASSESSMENT I. Importance A. Identify problems so corrective action can be taken to improve nutritional status. B. Determine if a person is well nourished enough to survive surgery or other treatments. II. Components A. Historical information B. Anthropometric data C. Biochemical (laboratory) data D. Physical exam III. Historical information A. Health history - may impact nutritional status 1. Previous or present alcoholism 2. Previous or present disease conditions a. diabetes b. cancer c. renal disease d. thyroid disorders 3. Previous or present eating disorders 4. Family history of obesity 5. Previous surgeries 6. Mental impairment 7. Weight changes 8. Dentition 9. Exercise habits B. Socioeconomic history - personal, environmental, financial influences onfood intake 1. Eating alone 2. Lack of money 3. Inadequate food preparation facilities 4. Poor education (eg, reading) 5. No transportation 6. Family problems that may result in low self esteem (eg. Excessive value of appearance in the family of a patient with eating disorders) 7. Drug history a. antidepressants - increase or decrease appetite b. diuretics - may waste potassium c. antacids (baking soda may contribute to sodium intake) d. vitamin/mineral supplements C. Diet history - provides a record of a person's food intake so that nutrient intake can be estimated and provides information so dietitian can predict how well the client will accept diet changes (in general, the fewest changes from usual diet, the better the compliance) 1. Information obtained a. types of foods consumed b. quantity of foods consumed (food models help client estimate) c. how foods are prepared d. dining out frequency e. beverage consumption (including alcohol) f. supplement consumption 2. Accuracy of data collected a. NON-JUDGMENTAL - some people are very sensitive about eating habits and weight b. technique of asking questions (avoid leading questions) 3. Tools a. 24-hour recall - record everything eaten in the last 24 hours 1. memory problem 2. may not be typical day 3. can do computerized diet analysis b. Usual intake (probably used most for diet histories) 1. good for people who have regular eating habits 2. sometimes used in combination with 24 hour recall 3. can give overall impression of diet, snacking patterns, consumption of sweets, etc. c. Food frequency checklist - how often the person eats food on a list (several times a day, daily, weekly, monthly) 1. not extremely precise 2. list of foods must be extensive 3. can give general impression of eating habits 4. sometimes used in combination with 24 hour recall d. Food diary - prospective record of foods eaten over a period of time (usually 3 days or 7 days). Average daily intake is calculated for each nutrient. 1. 3 days is pretty accurate if you have 2 weekdays and 1 weekend day 2. Can get info on time, place, with whom, and hunger and emotional state 3. Just keeping a record may change a person's food intake and therefore affect accuracy 4. Can compare overall food habits to guidelines (pyramid) for general impression of dietary adequacy 5. If computerized analysis is done, can compare individual nutrients to RDAs a. RDAs are designed for healthy people b. computer analysis implies more accuracy than reality a. substitutions b. incomplete data on some nutrients c. nutrient levels in food composition tables are averages d. accuracy of portion sizes 6. Caveats a. Adequate intake doesn't guarantee adequate nutritional status (may not absorb) b. Inadequate intake doesn't always indicate deficiency 7. Bottom line - diet history gives the dietitian a rough estimate of food intake so that problems or potential problems can be identified. Ultimate nutritional status can only be determined when diet history information is considered along with other components of nutritional assessment II. Anthropometrics A. In general 1. Gives information on body composition a. initial measurement provides baseline to monitor changes in nutritional status b. monitors progress of growth in pregnant women and infants and growing children c. detects undernutrition and obesity 2. Measures are compared to standards from population studies a. problem - population data may not apply to a particular individual b. use a variety of anthropometric measures for most accurate anthropometric assessment B. Anthropometric measures 1. Height and weight - most common a. Height 1. special equipment needed for kids under age 3 - lie kid down on special table with head at head board, straighten out legs and take length measurement at heel 2. adult - use stadiometer a. without shoes, heels together b. inflexible object on top of head c. use a stool if you are shorter than person d. can be estimated by 2X measurement from sternal notch to fingertips e. can be estimated from knee height b. Weight - beam balance, electronic most accurate 1. infants - weigh in balance scale that allows kid to lie (naked without diapers) 2. adults a. for repeated measures, same scale, same time of day, after voiding, in same weight clothing, without shoes, morning before breakfast is probably best 3. Scales have upper limits - can add weights to beam balance to increase limit 4. Remember that a lot of people are sensitive about their weight, so don't show judgment c. Interpretation 1. infants to age 20 use CDC growth charts a. get percentile for height and weight for age 1. 50th percentile is average 2. height and weight should be within 2 percentile ranges 3. there are charts for weight for height BMI, and head circumference b. Low percentiles may not de due to undernutrition or poor health, may be due to genetics (are parents short?, is weight for height OK?) c. Types of malnutrition indicated 1. acute (recent poor intake) a. height normal, low weight b. weight is affected by malnutrition before height (lose body stores first, then linear growth slows) 2. acute on chronic - continuing long term poor intake a. low weight and height percentiles b. weight for height low c. length of time undernourished has affected linear growth as well as body stores 3. past chronic a. low height, OK weight b. weight for height may be OK c. past long term undernutrition has affected linear growth,but body stores have been repleted (it takes longer for linear growth to catch up than body stores) Note: if growth plates on bones have closed, catch up growth will not occur d. Look for trends in growth curve,sudden slows in growth are a concern e. Obese - try to have weight gain slow and let height "catch up" to weight 2. Adults a. Height-weight tables (Metropolitan,1983) 1. based on mortality rates of insured population (mostly white) a. Divided into frame size categories 1. ht(cm)/wrist circ. (cm) = r = small medium large men >10.4 9.6 - 10.4 <9.6 women >11.0 10.1 - 11.0 <10.1 2. elbow breadth b. other countries use other standards (FAO/WHO), Indonesia has own h-w tables b. Calculation of ideal body weight (IBW) 1. Traditional a. women 1. 100 # for 1st 60 in 2. add 5 # for each in, over 60 3. large frame, add 10%; small frame,subtract 10% 4. eg b. men 1. 106# for 1st 60 in. 2. add 5 # for each in. over 60 3. add or subtract 10% depending on frame size 2. Newer (closer to Ins. Tables) a. Women: 119+3# for every in. over 60 in. (frame size adj) b. Men 135+3# for every in. over 63 in. (frame size adj) c. d. e. f. g. Can add 10% for those over 50 Subtract 5-10% for paraplegic; 10-15% for quadraplegic Range of weights may be best Problem - can be overweight without being over fat. What to use in calculations 1. Adjusted body weight (for obese) a. useful for equations to calculate energy and protein needs b. .25(Current BW - IBW) + IBW 2. Actual body weight for those within normal weight range 3. Desirable body weight if underweight i. Clinical interpretation % IBW >200 >120 or 130 110 - 120 80 - 90 % UBW 85-95 Nutritional status morbidly obese obese overweight mildly undernourished 70-79 <70 75-84 <75 mod. undernourished severely undernourished 2. BMI (Body Mass Index) a. weight (kg)/ht2 (m) b. 20 - 25 - least risk of death c. BMI > 25 is associated with obesity and greater risk of death d. Grades of obesity according to BMI I 25 - 29.9 II 30 - 40 III 40+ 3. Circumferences a. Head - used in children, estimates brain growth b. measure at largest part of head c. compare value to NCHS chart 4. Waist-to-hip ratio a. waist - measure at umbilicus (controversial) b. hip - measure at largest circumference c. divide waist by hip d. interpretation 1. women > .8, apple (android) 2. men > 1.0, apple (android) e. android body fat distribution is associated with a greater risk for some chronic diseases compared to gynoid or peripheral distribution 5. Body composition a. percent body fat 1. methods a. multiple site skinfold b. bioelectrical impedance c. dual energy x-ray absorptiometry d. body fat wand e. estimation by circumferences f. bod pod - air displacement 2. interpretation a. appropriate levels not well defined – need to collect a lot more data over many years to correlate % body fat to longevity b. average < 30 y/o men > 30 y/o men < 30 y/o women > 30 y/o women 12 - 15% 18 - 27% 22 - 29% 25 - 34% In general, over 25% in men and 33% in women is considered overfat; under 3% in men and 12% in women is underfat b. Somatic protein measures 1. hand grip strength - new, not widely used - strength is correlated with malnutrition 2. Mid-arm muscle circumference (MAMC) circumference of biceps muscle declines with malnutrition as protein reserves are depleted 3. measurement a. Measure triceps skinfold b. Measure midarm circumference c. calculation MAMC = Midarm circumference (cm) - (.314 triceps fatfold (mm)) III. Biochemical indices - tells what's going on internally A. useful in assessing protein, vitamin, mineral status B. Sensitivity - ability of a test to indicate abnormality when abnormality exists 1. some tests will not catch a problem in early stages, other, more sensitive tests will 2. eg., hb/hct are less sensitive than ferritin for determining iron deficiency, so hb/hct does not diagnose until anemia is advanced C. Specificity - ability of a test to indicate normal when no abnormality is present 1. Some tests of nutritional status can be abnormal for reasons other than nutritional problems 2. eg., Albumin could be low due to liver disease, not deficient protein intake D. blood 1. serum (blood minus cells and clot forming materials) 2. plasma (blood minus cells) 3. tests a. SMA - simultaneous multiple analysis b. CBC - complete blood count 4. dehydration concentrated blood and can falsely elevate values 5. hemodilution can falsely lower values 6. deficiency can be in progress before lab values reflect because stores may be released into blood 7. metabolites with short half-lives reflect recent nutritional status, metabolites with long half lives reflect long term status a. albumin - half life 23 days b. pre-albumin - half life 3 days (detects quick changes in nutritional status) D. Urine 1. specific gravity - hydration status 2. nitrogen balance 3. creatinine excretion E. Common tests related to nutritional state 1. Protein nutrition a. albumin 1. low values indicate prolonged protein malnutrition (long halflife and albumin can shift out of the cells into blood to slow decline) 2. slow to respond to nutrition therapy so not good indicator of improvement of status 3. disease states may affect albumin levels b. prealbumin – shorter half life – tells recent changes in protein status c. transferrin (protein that transports iron) 1. short half life, small body pool 2. not accurate indicator of protein status if iron status is poor d. retinol binding protein (carries vitamin A) and prealbumin are sensitive indicators e. total lymphocyte count (TLC) - protein malnutrition depresses the immune system 1. run with CBC 2. Calculation - WBC (mm3) X % lymph f. Antigen skin testing (delayed hypersensitivity (DH)- antigens to which most people are immune are injected just under the skin. After 48 hours site is checked for induration (hard raised area), and is scored from 0-2. If little or no induration - impaired immune status.(Other factors can affect this test, so it should not be the sole biochemical test for malnutrition) g. Nitrogen balance - assesses rate of depletion or repletion 1. Nitrogen input = protein intake (g)/6.25 2. Nitrogen output = amount of nitrogen in a 24 hour urine collection (UUN) plus 4 (skin, fecal, etc losses) 3. nitrogen bal = input - output h. Urinary creatinine excretion 1. creatinine is a breakdown product of phosphocreatine an energy source in skeletal muscle 2. amount excreted in urine is proportional to skeletal muscle mass 3. as muscles atrophy, excretion decreases 4. protein intake, menstrual cycle can affect 2. Cholesterol and lipoproteins 3. Hemoglobin/hematocrit - iron, hydration status IV. Physical exam - physical signs are last to appear in the progression of malnutrition A. Steps of malnutrition 1. Lack in diet (historical information) 2. Stores decline (anthropometric and biochem) 3. Body functions abnormally (biochemical) 4. Physical signs appear Note: Some physical signs have low specificity, eg, dry, scaly skin B. Some physical signs associated with malnutrition Sign Dull, thin, dry hair that is easy to pluck Possible nutrient deficiency Scaly skin around nostrils, cheilosis riboflavin Swollen face Kwashiorkor Pallor Iron Dullness, dryness of cornea Bitot's spots Vitamin A Fissuring of eye corners Riboflavin, B-6 Magenta tongue Atrophy or hypertrophy of taste buds Riboflavin Mottled tooth enamel Protein Folic acid, niacin Fluoride excess Spongy, bleeding receeding gums Vitamin C Thyroid enlarged Iodine V. Estimation of nutrient needs A. energy maintenance needs- Harris-Benedict equation (BEE) times activity and stress factors most commonly used 1. BEE a. (women) = 665 + (9.6 X wt (kg)) + (1.7 X ht(cm)) - (4.7 X age (years)) b. (men) = 66 + (13.7 X wt (kg)) + (5 X ht (cm)) - (6.8 X age (years)) Note: use adjusted BW if person is >125% IBW 2. multiply by each factor that applies a. Activity 1. very light/sedentary 1.2 -1.3 2. Light (no plnned activity, mostly officework) 1.5-1.6 3. Moderate (walking, stairclimbing during day) 1.6-1.7 4. Heavy (planned vigorous activities) 1.9-2.1 b. Stress 1. uncomplicated surgery 1.1 - 1.5 2. complicated surgery or fractures 1.2 - 1.4 3. Major burn 1.5 - 2.0 c. Fever 1.3 for each degree C above nrml f. Anabolism 1. 0.5 if pt experienced moderate weight loss 2. 1.1 - 1.5 if pt experienced severe weight loss 3. example 4. Alternative to Harris Benedict times factors: kcal X kg body wt Overweight Normal Underweight Sedentary Moderate Active 20-25 30 30 30 25 40 35 40 45-50 Athlete (90 min/d): 45-50 kcal/kg Hospitalized patients in stress: 40 - 45 kcal/kg Most other hospitalized patients: 30-35 kcal/kg 5. Equations provide a place to start - adjustment may be made for individual variation B. Protein 1. Nitrogen balance - Nitrogen in - Nitrogen out 2. Equations Person Protein needs per kg body wt Healthy .8 - 1 Fever, fracture, infection 1.5 - 2.0 Protein depleted 1.5 - 2.0 Extensive burns 1.5 - 3.0 Endurance athlete 1.2 – 1.4 Strength 1.6-1.7 VI. Special Considerations A. Pregnancy 1. blood volume expands, hemodilution (H/H low) 2. cholesterol increases B. Amputations - subtract according to % of body missing C. Deformed - may be impossible to measure accurately D. Elderly 1. naturally lose lean body mass and increase in proportion of fat as age, then very old tend to lose fat stores 2. Probably good to have some reserves 3. H/H tend to be low - may be a normal process of aging - less lean tissue, don't need as much hemoglobin (less tissue to oxygenate) 4. More prone to malnutrition a. lack of appetite b. presence of chronic diseases c. GI function declines d. many drugs e. mental problems Overall Macronutrient: Carbs General 60-65% kcal Endurance 65-70% kcal or 7-10 g/kg Protein General .8g/kg or 12-15% kcal Endurance 1.2-1.4 g/kg Strength 1.6-1.7 Fat Max of 30%