Maternal And Fetal Assessment Unit (MAFAU)
advertisement

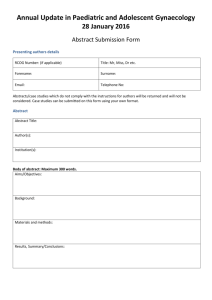
Women’s and Children’s Directorate Maternal and Fetal Assessment Unit: Improving the Patient Experience. Dear colleague, We are delighted to inform you about changes to the Maternal and Fetal Assessment Unit (MFAU) at PAH, which we hope will improve the experience of your patients. The MFAU team is now seeking your support for our efforts to deliver a fully-integrated care pathway. This will enable us to operate more efficiently, meet national guidelines, avoid unnecessary visits to hospital, and provide the right care more quickly. Last month, MFAU saw 600 women. We want to continue to improve services, even as demand increases. We are updating our guidelines, as well as promoting community-led care and choice. For example, we will shortly be starting outpatient induction of labour for low risk patients. This will reduce admissions and enhance patient experience. We recognise that the contribution of GPs is vital. Indeed, the Royal Colleges of GPs, Midwives, and Obstetricians and Gynaecologists have issued a joint statement on this role (attached), as part of a UK-wide bid to improve the care of pregnant women and new mothers. Based on this consensus, we are inviting GPs and community midwives to work with us as a team. We have included our new evidence-based guidelines (below), and are asking for your co-operation in adopting them to implement important operational changes: Ante-natal MFAU will accept women from 22 weeks only. GPs and midwives should ring the unit on 01279 827102 before sending patients directly to us. This will help to ensure patients do not face long waits. For the same reason, we are encouraging women to telephone before coming in. Patient safety remains paramount. Where gestation is below 22 weeks and there are concerns about fetal heartbeat, please listen to the heart to confirm viability and then ring MFAU to arrange a scan within 24 hours. Post-natal Where babies require additional support in the community, GPs are asked to review cases and then refer to the neonatal community team, unless clinically unwell then they should go to A&E It is most appropriate for postnatal women to be reviewed in the community in the first instance. However, please bleep the on-call registrar at PAH if urgent advice is needed with regards to management or admission. Women who need urgent attention more than 28 days after delivery should be referred to A&E. We look forward to working with you to improve services for our patients. Please read the guidelines and accompanying materials when you receive them. Feedback is very welcome. Kind regards Miss Rahat.Khan, Lead Consultant November 2011 Jasodra Moolchan, Lead midwife Consensus statement by RCGP, RCM, RCOG The role of the General Practitioner in Maternity Care - 6th November 2011 Representatives of the RCGP, RCM and RCOG have met to develop a consensus statement for the UK about the role of the GP in maternity care. The consensus statement acknowledges that GPs have an important role in maternity care and sets out a minimum of seven criteria that they should achieve to demonstrate their competence in this area, including: Pre-conception care, especially for those with complex care needs Health promotion in early pregnancy, including managing conditions such as bleeding Recognising and signposting emergency conditions directly to hospital Follow-up care for medical conditions such as diabetes and hypertension Provision of postnatal and contraception advice Professor Amanda Howe, RCGP Honorary Secretary said: “Many GPs would like to have an enhanced role in maternity care and this makes sense because of the strong bond between the woman and her family doctor. “We are reassured that our colleagues at the RCM and RCOG stand with us and share this view, as demonstrated by the publication of our joint statement. Cathy Warwick, RCM General Secretary, said: “High-quality, safe maternity services are dependent on all of the health professionals involved working together as a team and communicating well. I am delighted that the RCGP, RCOG and the RCM have come together to produce this important statement, which promotes collaborative working.” Dr Tony Falconer, RCOG President said, “We acknowledge the important role of family doctors in the provision of maternity services as they are the first point of contact for some women. “With their knowledge of a woman’s medical history, they are in a good position to advise on care, as described in the statement. “We believe good care can be provided through better joint working between healthcare professionals and this approach dovetails the recommendations laid out in our High Quality Women’s Health Care report.” The Role of the General Practitioner in Maternity Care: A Consensus Statement can be found on the RCGP website here. High Quality Women’s Health Care: A proposal for change can be found on the RCOG website here. Maternal and Fetal Assessment Unit (MFAU) Hamstel Road, Harlow, Essex, CM20 1QX Tel: 01279 444455 ext 2945 Gestation from 23 weeks Name : ______________________________ Team ____________________________ Address : ____________________________ EDD _____________________________ ____________________________________ Parity ____________________________ ____________________________________ Gestation _________________________ DOB ________________________________ Date referred to MFAU _______________ Hospital Number ______________________ Date attending MFAU ________________ Referred by: □GP □MW □Obstetrician □Self □Follow up MFAU referral criteria □ Reduced fetal movements □ Raised BP >150/100 symptomatic or asymptomatic, no proteinurea □ Raised BP >140/90 with 1+ or more protienurea, symptomatic or asymptomatic □ Mild abdominal pain □ Mild bleeding per vagina □ Itching in pregnancy □ Obstetric cholestasis monitoring/ □ Ruptured membranes at 37 weeks with no regular contractions □ Preterm rupture of membranes monitoring ( initially to be seen on labour ward) □ Surveillance of oligohydramnoius □ Confirmation of small or large for gestational age and ongoing assessment of intrauterine growth restriction □ Surveillance of pregnancy over 42 weeks when the woman declines induction of labour □To confirm presentation of fetus from 36 weeks □ Administration of prophylactic Anti D at 28 weeks □ Administer Betamethasone/Dexamethosone □ MRSA screening □Outpatient induction of labour for low risk women _____________________________________________________________________________ _____________________________________________________________________________ ________________________________________________________________________ Please see reverse History: Treatment / Assessment Requested:


![Letter to MPs re: maternal mental health report Dear [Name of MP] I](http://s3.studylib.net/store/data/006839335_1-7d7b3127aade7ad6d126565942ce75c1-300x300.png)