approved
advertisement

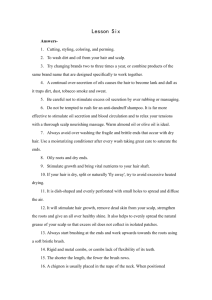
Ministry of Health of Ukraine BUKOVINIAN STATE MEDICAL UNIVERSITY “APPROVED” on methodical meeting of the Department of Anatomy, Topographical anatomy and Operative Surgery “………”…………………….2008 р. (Protocol №……….) The chief of department professor ……………………….……Yu.T.Achtemiichuk “………”…………………….2008 р. METHODICAL GUIDELINES for the 3d-year foreign students of English-spoken groups of the Medical Faculty (speciality “General medicine”) for independent work during the preparation to practical studies THE THEME OF STUDIES “Topographical anatomy and operative surgery of the cerebral part of the head” Module 1 “Topographical Anatomy and Operative Surgery of the Head, Neck, Thorax and Abdomen” Semantic module “Topographical Anatomy and Operative Surgery of the Head and Neck” Chernivtsi – 2008 1. Actuality of theme: The topographical anatomy and operative surgery of the head are very importance, because without the knowledge about peculiarities and variants of structure, form, location and mutual location of their anatomical structures, their agespecific it is impossible to diagnose in a proper time and correctly and to prescribe a necessary treatment to the patient. Surgeons usually pay much attention to the topographo-anatomic basis of surgical operations on the head. 2. Duration of studies: 2 working hours. 3. Objectives (concrete purposes): To know the definition of regions of the head. To know classification of surgical operations on the cerebral part of the head. To know the Topographical anatomy of mastoid region. The trepanation triangle (Shipot’s triangle). 4. Basic knowledges, abilities, skills, that necessary for the study themes (interdisciplinary integration): The names of previous disciplines 1. Normal anatomy 2. Physiology 3. Biophysics The got skills To describe the structure and function of the different organs of the human body, to determine projectors and landmarks of the anatomical structures. To understand the basic physical principles of using medical equipment and instruments. 5. Advices to the student. 5.1. Table of contents of the theme: The head is anatomically complex area of the body. The head is composed of a series of compartments, which are formed by bone and soft tissues. They are: the cranial cavity, two ears, two orbits, two nasal cavities, an oral cavity. The cranial cavity is the largest compartment and contains the brain and associated membranes (meninges). In addition to the major compartments of the head, two other anatomically defined regions of the head on each side are areas of transition from one compartment of the head to another. The infratemporal fossa is an area between the posterior aspect (ramus) of the mandible and a flat region of bone (lateral plate of the pterygoid process) just posterior to the upper jaw (maxilla). This fossa, bounded by bone and soft tissues, is a conduit for one of the major cranial nerves-the mandibular nerve (the mandibular division of the trigeminal nerve (V3)), which passes between the cranial and oral cavities. The pterygopalatine fossa on each side is just posterior to the upper jaw. This small fossa communicates with the cranial cavity, the infratemporal fossa, the orbit, the nasal cavity, and the oral cavity. A major structure passing through the pterygopalatine fossa is the (maxillary division of the trigeminal nerve) maxillary nerve (V2). The face is the anterior aspect of the head and contains a unique group of muscles that move the skin relative to underlying bone and control the anterior openings to the orbits and oral cavity. The scalp covers the superior, posterior, and lateral regions of the head. The border between the head and neck lies on such landmarks as: mental protuberance, lower part of base, angle and posterior border of ramus of mandible, lower semi-circle of external auditory meatus, superior nuchal line, external occipital protuberance (inion). The head is divided on cerebral and facial parts – by line, which begins from glabella, then goes above the superciliary arch, zygomatic arch to external acoustic meatus and go on to the lower part of mastoid process. The shape of the head is characterized by individual, sexual, racial, age-specific distinctions, besides the numerous congenital and acquired deformations of the scull and cerebrum occur. All these changes are very important for surgery. In the fetus and newborn, large membranous and unossified gaps (fontanelles) between the bones of the skull, particularly between the large flat bones that cover the top of the cranial cavity, allow: the head to deform during its passage through the birth canal; postnatal growth. Most of the fontanelles close during the first year of life. Full ossification of the thin connective tissue ligaments separating the bones at the suture lines begins in the late twenties, and is normally completed in the fifth decade of life. There are only three synovial joints in the head. The largest is the temporomandibular joint between the lower jaw (mandible) and the temporal bone. The other two synovial joints are between the three tiny bones in the middle ear, the malleus, incus, and stapes. CEREBRAL PART OF THE HEAD (THE SKULL) The cerebral part of the head is divided on fornix of skull (calvaria) and base of skull. The border between these areas begins from external occipital protuberance (inion), then goes by superior nuchal line, asterion (the convergence of three sutures – between temporal, parietal and occipital bones), sulcus between mastoid and squamous parts of temporal bone, upper semi-circle of external auditory meatus, lower edge of zygomatic process of temporal bone, forward edge of mandibular fossa, sphenoid crista, through the pterygomaxillary fissure to the sphenoidal rostrum (covered by vomer). Fornix of Skull (Calvaria) There are four regions consist of fornix of skull: 1) fronto-parieto-occipital (single), 2) temporal (couple), 3) mastoid (couple), 4) auricular (couple). Fronto-parieto-occipital region is limited by line goes from glabella, under superciliary arch, along superior temporal line, superior nuchal line to the external occipital protuberance (inion). There are superficial layers of soft tissues of this region is named a scalp. Although the scalp consists of five layers of soft tissue, the first three layers, called the scalp proper, are often clinically regarded as a single layer because they remain together when a scalp flap is made during a cran-iotomy (surgical opening of the calvaria) or when the scalp is torn off during accidents. It is difficult to separate the skin and the subcutaneous tissues of the scalp from the dense connective tissue of the epicranial apo-neurosis, or galea aponeurotica. Layers of the Scalp Each letter of the word S C A L P serves as a memory key for one of the layers of the scalp. Layer 1: Skin. Hair covers the scalp in most people. The skin of the scalp is thin, especially in elderly people, except in the occipital region. The skin contains many sweat and sebaceous glands and hair follicles. The skin of the scalp has an abundant arterial supply and good venous and lymphatic drainage systems. Scalp lacerations are the most common type of head injury requiring surgical care. These wounds bleed profusely because its communicating arteries enter around the periphery of the scalp, and they do not retract when lacerated because the scalp is tough. If these wounds are not treated appropriately, a scalp infection may develop and spread into the underlying bones of the calvaria, causing osteomyelitis. The infection can also spread to the cranial cavity, producing an extradu-ral (epidural) abscess, meningitis, or both. The ducts of the sebaceous glands that are associated with hair follicles in the scalp may become obstructed, resulting in the retention of secretions and the formation of sebaceous cysts (wens). Because they are in the skin of the scalp proper, sebaceous cysts move with the scalp. Layer 2: Connective tissue. This thick, subcutaneous layer of connective tissue is richly vascular-ized and well supplied with nerves. Its collagenous and elastic fibers criss-cross in all directions, attaching the skin to the third layer of the scalp (aponeurosis epicranialis). Fat is enclosed in lobules between the connective fibers. The amount of subcutaneous fat in the scalp is relatively constant, varying little in emaciation or obesity, but decreases with advancing age. As a result, the scalp is thinner in elderly. Layer 3: The Epicranial aponeurosis is a strong membranous sheet that covers the superior aspect of the calvaria. This aponeurosis is the membranous tendon of the fleshy bellies of the epicranius muscle (two occipital bellies (occipitalis) and two frontal bellies (frontalis) that are connected by the epic-ranial aponeurosis. The frontal bellies pull the scalp anteriorly and wrinkle the forehead transversely, whereas the occipital bellies pull the scalp posteriorly and wrinkle the skin on the posterior aspect of the neck. The epicra-nial aponeurosis is continuous laterally with the temporal fascia covering the temporalis muscle. This fascia is attached to the zygomatic arch. The epicranial aponeurosis is a clinically important layer of the scalp. Owing to its strength, a superficial laceration in the skin does not gape because its margins are held together by this aponeurosis. When suturing a superficial wound, deep sutures are not necessary because the epicranial aponeurosis docs not allow wide separation of the scalp proper. Deep scalp wounds gape widely when the epicranial aponeurosis is split or lacerated in the coronal plane, owing to the pull of the frontal and occipital parts of the epicranius muscle in different directions (anteriorly and posteriorly, respective). For this reason, deep coronal lacerations gape most widely. As mentioned, bleeding from scalp wounds is severe because the arteries cannot retract owing to the density of the connective tissue in the second layer of the scalp. Layer 4: Loose areolar tissue. This subapo-neurotic layer of areolar or loose connective tissue is somewhat like a sponge because it contains innumerable potential spaces that are capable of being distended with fluid. It is this loose connective tissue layer that allows free movement of the scalp proper, composed of layers 1–3. The loose areolar connective tissue layer is the dangerous area of the scalp because pus or blood in it can spread easily. Infection in this layer can also be transmitted to the cranial cavity through emissary veins that pass from this layer through apertures in the cranial bones, e.g. the parietal foramina. The emissary veins conned with the intracranial venous sinuses, e.g. the superior sagittal sinus. Infections in the loose connective tissue layer may produce inflammatory processes in the emissary veins, leading to thrombophlebitis of the intrac-ranial venous sinuses and the cortical veins. Awareness of the limits of the loose connective tissue layer (also known as the subaponeurotic space) is important so that the possible spread of an infection can be anticipated. An infection is unable to spread into the neck because the occipitalis muscle is attached posteriorly to the highest nuchal line of the occipital bone and posterolaterally to the mastoid parts of the temporal bones. An infection is unable to spread laterally beyond the zygomatic arches because the epicranial aponeurosis is continuous with the temporal fascia, where it is attached to these arches. An infection or fluid (e.g., blood or pus) can enter the eyelids and the root of the nose because the frontalis muscle is inserted into the skin and dense subcutaneous tissue and is not attached to the frontal bone. Because of the free movement permitted by the loose connective tissue layer, it is through it that the scalp proper separates during accidents (e.g., when the hair is caught in machinery). Layer 5: Pericranium. The pericranium is the deepest layer of the scalp and is the periosteum on the outer surface of the calvaria. The periosteum adheres to the suture-lines of the skull; collections of pus or blood beneath this layer, therefore, outline the affected bone. This is particularly well seen in birth injuries involving the skull (cephalohaematoma). Nerves of the Scalp The sensory innervation of the scalp anterior to the auricles (external ears) is through nerves that are branches of all three divisions of CN V, the trigeminal nerve. Posterior to the auricles, the nerve supply of the scalp is from the spinal cutaneous nerves (C2 and C3) of the neck from the cervical plexus. The areas of distribution of the branches of the trigeminal and cervical nerves are usually about equal. Arteries of the Scalp The blood supply of the scalp is from the external carotid arteries – through the occipital, posterior auricular, and superficial temporal arteries, and from the internal carotid arteries – through the supra-trochlear and supraorbital arteries. All these arteries anastomose freely with each other. The bones of calva-ria are supplied mainly by the middle meningeal arteries, branches of the maxillary arteries, but these bones receive some blood from pericranial vessels that enter the cranium through Volkmann’s canals (vascular canals in bones). Veins of the Scalp The vena comitantes accompany the arteries of the scalp and have the same names. The supraorbital and supratrochlear veins unite at the medial angle or canthus of the eye to form the facial vein. Here, it communicates with the superior ophthalmic vein, thereby making a link that may allow facial infections to reach the cavernous sinus. The superficial temporal vein joins the maxillary vein to form the retromandibular vein posterior to the neck of the mandible. The posterior auricular vein drains the scalp posterior to the auricle and often receives a mastoid emissary vein from the sigmoid sinus, an intracranial venous sinus. Lymphatic drainage of the Scalp Lymphatic drainage of the scalp generally follows the pattern of arterial distribution. The lymphatics in the occipital region initially drain to occipital nodes near the attachment of the trapezius muscle at the base of the skull. Further along the pathway occipital nodes drain into upper deep cervical nodes. There is also some direct drainage to upper deep cervical nodes from this part of the scalp. Lymphatics from the upper part of the scalp drain in two directions: - posterior to the vertex of the head they drain to mastoid nodes (retro-auricular/posterior auricular nodes) - posterior to the ear near the mastoid process of the temporal bone and efferent vessels from these nodes drain into upper deep cervical nodes; - anterior to the vertex of the head they drain to pre-auricular and parotid nodes anterior to the ear on the surface of the parotid gland. Finally, there may be some lymphatic drainage from the forehead to the submandibular nodes through efferent vessels that follow the facial artery. TEMPORAL REGION The boundaries of the left and right temporal regions are correspond to the attachment of temporal muscle (on the superior temporal line) above and the zygomatic arch below. The layers of soft tissue: - Skin is thin and mobile. - Subcutaneous connective tissue is advanced moderately. It contains of branches of the superficial temporal artery and vein, auriculotemporal nerve (from mandibular devision of trigeminal nerve). - The superficial fascia (continuation of the aponeurotic helmet). - Temporal aponeurosis (temporal fascia) which consist of two leafs attached to the superior edges of the zygomatic arch. Through the thickness of the temporal muscle pass profunda temporal vessels and nervs, temporal branches of the facial nerve. - Periosteum. - Temporal bone. MASTOID REGION The boundaries of the mastoid region is corresponding to the exterior form of mastoid process of the temporal bone. Layers: - Skin is thin, hairless, contains of sudoriferous glands. - Subcutaneous connective tissue is undeveloped. It contains of branches of the auricularis posterior muscle, occipital and posterior auricular vessels, posterior auricular and great auricular nerves (from facial nerve). - Aponeurosis is thin, continuation of the apo-neurotic helmet. - Periosteum is hardly connected with the bone except of triangular area (Shipot’s trepanation triangle). - Bone (mastoid process of temporal bone) contains of mastoid air cells and the largest from them – the mastoid (Valsalva’s) antrum which communicated with the cavity of the middle ear. Shipot’s trepanation triangle. It is very important landmark for harmless approach to the mastoid antrum (trepanation of mastoid process) in case of mastoiditis (potential complication of mesotympanitis) for evacuation of pus. The triangle is limited: anteriorly – suprameatal spine (Henle spine), posteriorly – crista mastoidea, and superiorly – horizontal line as continuation of the zygomatic arch. To the Shipo’s trepanation triangle adjoins: anteriorly – facial canal (Fallopian aqueduct), posteriorly – sigmoid sinus, and superiorly – middle ear (tympanic cavity). These anatomical structures may be mistakenly damaged by operating gouge during the trepanation of mastoid process (antrotomy). MENINGES OF THE BRAIN The brain, as well as the spinal cord, is surrounded by three layers of membranes (the meninges) – a tough, outer layer (the dura mater), a delicate, middle layer (the arachnoid mater), and an inner layer firmly attached to the surface of the brain (the pia mater). The cranial meninges are continuous with, and similar to, the spinal meninges through the foramen magnum, with one important distinction-the cranial dura mater consists of two layers, and only one of these is continuous through the foramen magnum. Cranial Dura Mater The cranial dura mater is a thick, tough, outer covering of the brain. It consists of an outer periosteal layer and an inner meningeal layer: - the outer periosteal layer is firmly attached to the skull, is the periosteum of the cranial cavity, and is continuous with the periosteum on the outer surface of the skull at the foramen magnum and other intracranial foramina; - the inner meningeal layer is in close contact with the arachnoid mater and is continuous with the spinal dura mater through the foramen magnum. The two layers of dura separate from each other at numerous locations to form two unique types of structures: (1) dural partitions, which project inward and incompletely separate parts of the brain; (2) intracranial venous structures. The arterial supply to the dura mater consists of: - anterior meningeal arteries (branches of the ethmoidal arteries) in the anterior cranial fossa; - the middle and accessory meningeal arteries (branch of the maxillary artery) in the middle cranial fossa; - the posterior meningeal artery and other me-ningeal branches in the posterior cranial fossa. The middle meningeal artery is a branch of the maxillary artery. It enters the middle cranial fossa through the foramen spinosum and divides into anterior and posterior branches: the anterior branch passes in an almost vertical direction to reach the vertex of the skull crossing the pterion during its course; the posterior branch passes in a posterosuperior direction, supplying this region of the middle cranial fossa. The posterior meningeal artery and other meningeal branches supplying the dura mater in the posterior cranial fossa come from several sources: - the posterior meningeal artery, the terminal branch of the ascending pharyngeal artery, enters the posterior cranial fossa through the jugular foramen; - a meningeal branch from the ascending pharyn-geal artery enters the posterior cranial fossa through the hypoglossal canal. - meningeal branches from the occipital artery enter the posterior cranial fossa through the jugular foramen and the mastoid foramen; - a meningeal branch from the vertebral artery arises as the vertebral artery enters the posterior cranial fossa through the foramen magnum. Innervation of the dura mater is by small meningeal branches of all three divisions of the trigeminal nerve (V1, V2, V3) and the first, second, and sometimes, third cervical nerves. Arachnoid Mater The arachnoid mater is a thin, avascular membrane, against, but not adherent to, the inner surface of the dura mater. From its inner surface thin processes or trabeculae extend downward, cross the subarach-noid space, and become continuous with the pia mater. The arachnoid lies against the dura mater, and does not enter the grooves or fissures of the brain, except for the longitudinal fissure between the two cerebral hemispheres. Pia Mater The pia mater is a thin, delicate membrane that closely invests the surface of the brain. It follows the contours of the brain, entering the grooves and fissures on its surface, and is closely applied to the roots of the cranial nerves at their origins. Arrangement of Meninges and Spaces There is a unique arrangement of meninges, coupled with real and potential spaces within the cranial cavity. A potential space is related to the dura mater, while a real space exists between the arachnoid mater and the pia mater. Extradural Space The potential space related to the dura mater is the extradural space – the outer or periosteal layer of dura mater is firmly attached to the bones surrounding the cranial cavity resulting in this potential space between these two structures; This potential space can become a fluid-filled actual space when a traumatic event results in a vascular hemorrhage. Bleeding into the extradural space due to rupture of a meningeal artery or a torn dural venous sinus results in an extradural hematoma. Bleeding due to the tearing of a vein as it enters a dural venous sinus results in a subdural hematoma. Subarachnoid Space Deep to the arachnoid mater is the only normally occurring fluid-filled space associated with the meninges. It occurs because the arachnoid mater clings to the inner surface of the dura mater and does not follow the contour of the brain, while the pia mater, being against the surface of the brain, closely follows the grooves and fissures on the surface of the brain. A narrow space (the subarachnoid space) is therefore created between these two membranes. The subarachnoid space surrounds the brain and spinal cord and in certain locations it enlarges into expanded areas (subarachnoid cisterns). It contains cerebrospinal fluid (CSF) and blood vessels. Cerebrospinal fluid is produced by the choroid plexus. 5.2. Theoretical questions to studies: 1. 2. 3. 4. 5. 6. 7. The regions of the head. The layer-by-layer structure of the scalp. The blood supply of the scalp. The nerve supply of the scalp. The brain. The meninges of the brain. The mastoid region. 5.3. Materials for self-control: DIRECTIONS: Each question below contains four or five suggested responses. Select the one best response to each question. 1. The carotid sheath and its contents may be safely retracted as a unit during surgical procedures on the neck. The contents of the carotid sheath include all the following structures EXCEPT the A common carotid artery B external carotid artery C internal jugular vein D sympathetic chain E vagus nerve 2. All the following statements correctly pertain to the sternomastoid muscle EXCEPT A It divides the neck into anterior and posterior triangles B It receives innervation from a nerve that passes through the foramen magnum C The head is extended when both left and right sternomastoid muscles contract simultaneously D Torticollis (wry neck) results from unilateral spasm of the sternomastoid muscle E Unilateral contraction brings the chin toward the contralateral shoulder Questions 3-6 A 28-year-old man is treated in an emergency room for a superficial gash on his forehead. The wound is bleeding profusely, but examination reveals no fracture. While the wound is being sutured, he relates that while he was using an electric razor, he remembers becoming dizzy and then “waking up on the floor with blood everywhere.” The physician suspects a hypersensitive cardiac reflex. 3. The afferent component of the cardiac reflex that slows the heart is carried by A cardiac nerves arising from the cervical sympathetic chain B a branch of the glossopharyngeal nerve C the inferior root of the ansa cervicalis D the superior root of the ansa cervicalis E the vagus nerve 4. The efferent component of the cardiac reflex that slows the heart is carried by A cardiac sympathetic nerves B a branch of the glossopharyngeal nerve C the inferior root of the ansa cervicalis D the superior root of the ansa cervicalis E the vagus nerve 5. The forehead and scalp bleed profusely. All the following statements correctly pertain to the blood supply to the scalp EXCEPT A bleeding deep to the epicranial aponeurosis may spread widely over the cranium B bleeding superficial to the epicranial aponeurosis may exacerbate a depressed cranial fracture C contralateral anastomotic connections are abundant D portions of the scalp are supplied by branches of the external carotid artery E portions of the scalp are supplied by branches of the internal carotid artery 6. The patient’s epicranial aponeurosis (galea aponeurotica) is penetrated, which results in severe gaping of the wound. The structure underlying the epicranial aponeurosis is A a layer containing blood vessels B bone C the dura mater D the periosteum (pericranium) E the tendon of the epicranial muscles (occipitofrontalis) Questions 7-12 A 53-year-old woman has a paralysis of the right side of her face that produces an expressionless and drooping appearance. She is unable to close her right eye, has difficulty chewing and drinking, perceives sounds as annoyingly intense in her right ear, and experiences some pain in her right external auditory meatus. Physical examination reveals loss of the blink reflex in the right eye upon stimulation of either cornea and loss of taste from the anterior two-thirds of the tongue on the right side. Lacrimation appears normal in the right eye, the jaw-jerk reflex is normal, and there appears to be no problem with balance. 7. The inability to close the right eye is the result of involvement of A the buccal branch of the facial nerve B the buccal branch of the trigeminal nerve C the levator palpebrae superioris muscle D the superior tarsal muscle (of Muller) E none of the above 8. The difficulty with mastication is the result of paralysis of A the right buccinator muscle B the right lateral pterygoid muscle C the right masseter muscle D the right zygomaticus major muscle E none of the above 9. The pain in the external auditory meatus is due to involvement of sensory neurons that have their cell bodies in the A facial nucleus B geniculate ganglion C pterygopalatine ganglion D spinal nucleus of cranial nerve V E trigeminal ganglion 10. The hyperacusia associated with the right ear results from involvement of A the auditory nerve B the chorda tympani nerve C the stapedius muscle D the tensor tympani muscle E the tympanic nerve of Jacobson 11. The branch of the facial nerve that conveys secretomotor neurons involved in lacrimation is the A chorda tympani B deep petrosal nerve C greater superficial petrosal nerve D lacrimal nerve E lesser superficial petrosal nerve 12. To produce the described signs and symptoms, a lesion involving the facial (CN VII) nerve would be: located A in the internal auditory meatus B at the geniculate ganglion C in the facial canal just distal to the geniculate ganglion D at the stylomastoid foramen E within the parenchyma of the parotid gland 13. Which of the following statements concerning the lacrimal apparatus is correct? A The lacrimal gland lies in the medial portion of the orbit B Lacrimal fluid is secreted at the puncta in the medial edges of both upper and lower lids C The nasolacrimal duct has a blind-ending lacrimal sac as its upper portion D the nasolacrimal duct ends in the middle meatus of the nose E None of the above 14. A small tumor of the orbit that involves the orbital foramen will produce which of the following signs and symptoms? A Blindness in one eye B Dilated pupil with loss of the pupillary reflex and accommodation C Paralysis of the superior rectus, inferior rectus, medial rectus, inferior oblique, and levator palpebrae superioris muscles D Venous engorgement of the retina E None of the above 15. A 24-year-old boxer, after stumbling repeatedly, sees an ophthalmologist. He is found to have 20/20 vision. Upon testing the extraocular muscles, the examiner finds that elevation is balanced, but in depression the right eyeball deviates slightly toward the midline and the patient reports seeing double. The examiner has determined that the problem lies in the right A abducens nerve B inferior division of the oculomotor nerve C optic nerve D superior division of the oculomotor nerve E trochlear nerve 16. All the following statements about the ciliary ganglion are correct EXCEPT A it contains the cell bodies of postganglionic parasympathetic neurons B preganglionic parasympathetic axons reach it via the oculomotor nerve C postganglionic neurons from this ganglion innervate the ciliary muscle D postganglionic neurons from this ganglion innervate the dilator pupillae muscle E sensory fibers passing through this ganglion participate in the blink reflex 17. Sympathetic fibers to the eye A are preganglionic from C1-C2 B have preganglionic cell bodies in the superior cervical ganglion C have preganglionic cell bodies in the T1-T2 cord levels D have postganglionic cell bodies in the ciliary ganglion E reach the eye via gray rami communicantes 18. Infection in the region drained by the angular vein may result in venous thrombosis of the cavernous sinus via the A anterior superior alveolar vein B infraorbital vein C internal maxillary vein D sphenopalatine vein E superior ophthalmic vein 19. All the following signs could result from infection within the right cavernous sinus EXCEPT A constricted pupil in response to light B engorgement of the retinal veins upon ophthalmoscopic examination C loss of corneal blink reflex upon touching right conjunctiva D ptosis (drooping) of the right eyelid E right ophthalmoplegia (loss of all voluntary movement of an eye) 20. Concerning the arterial supply to the brain, all the following statements correctly pertain to the cerebral arterial circle (of Willis) EXCEPT A it usually consists of the anterior communicating artery, anterior cerebral arteries, middle cerebral arteries, and posterior cerebral arteries B it should provide collateral circulation when a cerebral artery or internal carotid artery becomes occluded C it is complete in less than 50 percent of the population D it is particularly prone to aneurysms E it will adequately supply the lateral aspect of the left cerebral hemisphere in the event of occlusion of the left middle cerebral artery in the lateral fissure 21. The vertebral arteries are correctly described by which of the foj. lowing statements? A They arise from the common carotid artery on the left and the brachiocephalic artery on the right B They enter the cranium via the anterior condylar canals C They enter the cranium via the posterior condylar canals D They pass through the transverse processes of several cervical vertebra E They give rise to the posterior cerebral arteries 22. Reflexes that protect the inner ear from excessive noise involve the contraction of the tensor tympani and stapedius muscles. Correct statements about the tensor tympani muscle include all the following EXCEPT A it inserts onto the malleus B it is derived from the first branchial arch C it is innervated by the chorda tympani nerve D it lies parallel to the auditory tube 23. In addition to hearing loss and balance disturbances, a tumor in the internal acoustic meatus may be responsible for all the following signs and symptoms EXCEPT A dry eye from loss of secretion of the lacrimal gland B loss of secretion of the parotid gland on one side C loss of secretion of the submandibular and sublingual glands on one side D dry nasal mucosa from loss of secretion of the nasal glands on one side E facial paralysis 24. Tic douloureux (trigeminal neuralgia) is characterized by sharp pain over the distribution of the trigeminal nerve. This syndrome involves neurons that have their cell bodies in A the geniculate ganglion B the otic ganglion C the pterygopalatine ganglion D the submandibular ganglion E none of the above 25. A cranial fracture through the foramen rotundum that compresses the enclosed nerve results in A inability to clench the jaw firmly B paralysis of the inferior oblique muscle of the orbit C regurgitation of fluids into the nasopharynx during swallowing D uncontrolled drooling from the mouth E none of the above 26. Which of the following statements concerning opening the jaw is correct? A The axis of rotation passes through the mandibular foramen B The gliding movement is the result of contraction of the medial pterygoid muscle C The jaw openers are innervated by the maxillary division of the trigeminal nerve D There is gliding movement in the inframeniscal compartment of the temporomandibular joint E There is rotation in the suprameniscal compartment of the temporomandibular joint 27. In dislocation of the jaw, displacement of the articular disk beyond the articular tubercle of the temporomandibular joint results from spasm or excessive contraction of which of the following muscles? A Buccinator B Lateral pterygoid C Medial pterygoid D Masseter E Temporalis 28. Infection may spread from the nasal cavity to the meninges along the olfactory nerves. Olfactory fibers pass from the mucosa of the nasal cavity to the olfactory bulb via A the anterior and posterior ethmoidal foramina B the hiatus semilunaris C the sphenopalatine foramen D the nasociliary nerves E none of the above 29. The blood supply to the vestibular region of the nasal cavity is from branches of all the following vessels EXCEPT the A anterior ethmoidal branch of the ophthalmic artery B incisive branch of the descending palatine artery C posterior ethmoidal branch of the ophthalmic artery D sphenopalatine artery E superior labial branch of the facial artery 30. Although the ciliary action of the mucosa facilitates drainage of the paranasal sinuses, body position is paramount. Paranasal sinuses that drain by gravity with the body in the erect position include all the following EXCEPT the A frontal B inferior ethmoidal C middle ethmoidal D maxillary E superior ethmoidal Literature 1. Snell R.S. Clinical Anatomy for medical students. – Lippincott Williams & Wilkins, 2000. – 898 p. 2. Skandalakis J.E., Skandalakis P.N., Skandalakis L.J. Surgical Anatomy and Technique. – Springer, 1995. – 674 p. 3. Netter F.H. Atlas of human anatomy. – Ciba-Geigy Co., 1994. – 514 p. 4. Ellis H. Clinical Anatomy Arevision and applied anatomy for clinical students. – Blackwell publishing, 2006. – 439 p.