Chapter 1 Introducing Health Psychology
advertisement

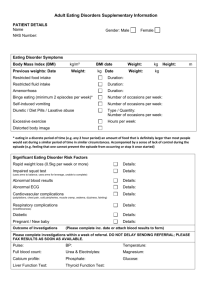
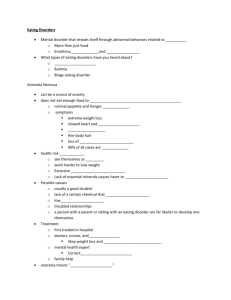
Chapter 15 Eating and Weight eating disorder - Any serious and habitual disturbance in eating behavior that produces unhealthy consequences. This definition excludes rare disorders such as "pica" (the eating of non-nutritive substances such as chalk or wood) and "rumination disorder of infancy" which involves an apparently healthy infant or young child vomiting up his or her food for no apparent reason). the four major problems of eating - are the focus of our text: (1) overeating and dieting, (2) anorexia nervosa, (3) bulimia nervosa, and (4) binge eating. anorexia nervosa - An eating disorder characterized by intentional starvation, distorted body image, excessive amounts of energy expended, and an intense fear of gaining weight. Mary Kate Olsen has this disorder. ducted glands - produce substances needed for digestion (such as saliva). These substances enter the digestive system via the ducts. salivary glands - Glands that furnish moisture (saliva) which allows the taste buds of the tongue to function (no saliva, no taste). digestive tract (system) - includes (in order) the mouth, pharynx, esophagus, stomach, small intestine, large intestine (colon), rectum, and anus. The digestive system is plagued by more diseases and disorders than any other body system. pharynx - The part of the digestive tract between the mouth and the esophagus. esophagus - The tube leading from the pharynx to the stomach. peristalsis - rhythmic contractions of the "circular muscles" that propel food through the digestive tract. gastric juices - are secreted by the stomach AND the glands that empty into the stomach secretions that aid in digestion. stomach - Has as its "primary" purpose, mixing of food particles with gastric juices, preparing for absorption of nutrients by the small intestine. Very little nutrient absorption occurs in the stomach. Digestion of "protein" with the aid of the enzyme "pepsin" is a "secondary" function of the stomach. pepsin - An enzyme responsible for digestion of protein in the stomach. pancreatic juices - Are released via ducts into the small intestine and serve two functions: (1) digestion of carbohydrates and fats and (2) to lower the level of acidity of the mixture of food and gastric juices coming from the stomach. small intestine - Absorbs nutrients from: (1) proteins, (2) carbohydrates, and (3) fats. Protein and carbohydrate nutrients are absorbed in the upper third of the small intestine. Fats nutrients are absorbed in the middle third of the small intestine. bile salts - are produced in the liver and stored in the gall bladder. They are released into the small intestine where they break down fat molecules to a form that can be processed pancreatic enzymes. liver - The largest gland in the body. Its functions include: (1) aiding digestion by producing bile, (2) regulating organic components of the blood, and (3) acting as a detoxifier of the blood. gall bladder - A ducted sac attached to the liver in which bile (produced by the liver) is stored. large intestine (colon) - The only absorption that takes place in the large intestine is of: (1) water, (2) some minerals, and (3) vitamins produced by bacteria that normally live in the colon. feces - Any materials left over after digestion. rectum - The end of the digestive tract leading to the anus. anus - Opening through which feces are eliminated. factors that influence weight - include: (1) caloric content, a given volume such as one square inch of fats contains more calories than the same volume of carbohydrates or sugars, (2) rate at which food moves through the body, (3) metabolic rate, which varies widely from person to person, and (4) activity level. leptin - A protein hormone produced by fat cells involved in "long term" regulation of weight. Depletion of fat reserves results in lowered leptin levels. This signals the central nervous system to initiate eating behavior. hypothalamus - A small structure located in the brain beneath the thalamus. It is the main brain area involved in the control of eating and drinking behaviors. It responds to changing leptin levels. ghrelin - A peptide hormone produced primarily in the stomach and involved in the "short term" regulation of eating and weight. Levels rise when we get hungry and this signals the hypothalamus to release "neuropeptide Y and other chemicals that trigger eating. After we have eaten, ghrelin levels fall. cholecystokinin (CCK) - A peptide hormone released by the intestines that also acts on the hypothalamus and produces feelings of "satiation" after eating. Like grehlin, CCK is involved in "short term" eating and weight regulation. satiation (satiety) - The technical term for feeling "full" after eating. The opposite of hunger. The hypothalamus contains both a hunger and a satiety center. experimental starvation - Ancel Keys conducted a study in which men dieted down to 75% of their weight. At first, weight loss was quick but got slower as the bodies adapted to lower caloric intake. The men irritable, aggressive, and inactive. When allowed to eat normally, they regained the weight easily but their normal "mood" was slow to return. experimental weight gain - Allen Simms provided a group of men in a prison with as much tasty food as they wanted (of many types). Weight gain was quick at first but then (as above) slowed as the body adapted. Some were unable to attain their goal of a weight gain of 20-30 pounds. Food eventually became repulsive. When a normal diet was reinstated, those with a "family history of obesity" had more trouble getting back to their original weights. These two studies taken together show that (1) both gaining and losing weight can be difficult because the body wants to remain at its "setpoint" and adapts to changing diets, (2) people have individual tendencies with regard to body makeup, and (3) changes in diet can bring about significant psychological changes. obese people - (1) eat more food, (2) seem to have a preference for foods rich in fat, which is more calorie dense than carbohydrates or sugars, and (3) tend to be inactive. Muscle and bone weigh more than fat so some people (like athletes) can be heavier (for a given size) and weigh more than obese people. weight charts - for desirable weights (based on height and frame size) are published by the Metropolitan Life insurance Company, based on data from the Society of Actuaries. An "actuary" is an expert (often employed by insurance companies) who can examine large databases and evaluate the likelihood of events and quantify the outcomes in order to minimize losses (e.g., what is the probability of heart attack for a non-smoking, overweight, 50 year old European American female?). A look at Table 15.1 shows that between 1959 and 1983 "desirable weight" the "chart based" desirable weight values increased significantly (by about 10 pounds overall). Percent body fat – is a better measure of obesity than weight. It can be assessed by (1) measuring a “fold” of skin or (2) by measuring bioelectrical impedance (the body’s resistance to a small electric current). This is the more accurate measure. body mass index (BMI) - Is an estimate of obesity determined by body weight and height (weight in kilograms / height in meters2). Despite the fact than BMI does NOT tell us a person’s ratio of fat to muscle, it is currently a popular measure. Overweight is defined as BMI of 25 to 30 and obesity as BMI of 30 or more (which corresponds roughly to “20%” over the 1983 Metropolitan Life insurance Company chart’s “desirable weight.” cultural changes - Prior to 1920 being heavy was a sign of prosperity and being thin was associated with disease and poverty whereas being plump or fat was associated with prosperity and wealth. Now, about 100 years later, things have reversed. demographics - From the 1980s through the 1990s, obesity increased by 50%. This trend is MOST problematic in the U. S. with “35%” of the population obese (BMI of 30 or greater) and another 30% overweight (BMI of 25 - 30). setpoint model - The body has a preferred level of fat that it fights to maintain. If fat (and leptin) levels fall, the body (1) slows its metabolic rate, and (2) increases hunger, in response to messages from the hypothalamus. The model does NOT tell us why some people’s setpoints are just too high. genetics - Evolution has given us a “thrifty metabolism” that wants to store fat when food is plentiful. This is no longer adaptive though. While this is generally true, people differ greatly in tendency to gain weight. Obesity runs in families. Adoption and twin studies support a strong role of genetics in obesity AND in how fat is distributed around the body. the positive incentive model - acknowledges three important factors: (1) taste, (2) learning, and (3) social context, which the setpoint model does not. People eat more if the food tastes good. Variety is important. Sclafani & Springer found that a “supermarket” diet (high fat, high sugar, and lots of variety) produced weight gains of “269%” in laboratory rats. People eat more in the presence of others. a U shaped function - With weight plotted on the X axis and mortality plotted on the Y axis, a U shaped function results. Those who are very underweight and those very overweight have higher mortality rates than those of normal weight, however, obesity is the bigger risk factor. Interestingly, being moderately overweight may not pose much more risk than being in the normal weight range. a big butt is healthier than a fat gut - Some people carry their excess weight mainly around the abdomen (the “beer belly”) whereas others put fat on around the hips and thighs and these differences have a genetic component. Those whose fat is concentrated in the abdomen (high waist to hip ratio) are at increased risk for (1) metabolic syndrome, (2) cardiovascular disease, and (3) Type 2 diabetes, even if they are not obese. amenorrhea - Cessation of the menses (woman's monthly cycle). diets don't work - In 2002, a Federal Trade Commission report stated that (1) "miracle diets," supported by testimonials and extensive advertising were highly misleading and (2) that according to U. S. Surgeon General, Richard Carmona, "The surest and safest way to weight loss and healthier living is by a combination of healthier eating and exercising." Weight Watchers - is one example of a program that stresses "portion control" which our text cites as a sensible approach to weight loss. low carbohydrate diets - such as Atkins, Sugarbusters, and South Beach allow virtually unlimited fat and protein (meat). There was concern that these diets would lead to cholesterol increases. At least one study did NOT support this concern. People do begin to crave carbs after a time and don't stay with such programs. high carbohydrate diets - such as the Ornish vegetarian diet previously discussed are healthy and allow people to eat their fill of vegetables, but are even harder to stay with. behavior modification programs - focus on changing lifestyle, and in particular: (1) setting eating plans and goals, (2) setting exercise goals, and (3) having the goal of gradual weight loss and maintenance. amphetamines (stimulants) - were prescribed for weight loss in the 1950s and 60s. However, as tolerance built up, dosage had to be increased and dependence could become more problematic than obesity. the fen-phen diet - (fenfluramine and phenylpropylalanine) was found to cause damage to heart valves and points out how dangerous such approaches can be. Increased knowledge about hormones and hunger may least to safer more effective medications. surgery - Gastric binding (placing a band around the stomach) and gastric bypass (routing food around most of the stomach) are considered for people (1) with BMIs over 35 or (2) who must lose weight because of related health risks. Patients will need to take nutritional supplements for the rest of their lives and as with any surgery, there are risks. Liposuction is a "cosmetic" surgery only and the removal of fat tissue carries NO health benefits. the Consumer Reports 2002 Survey - Of the 32,000 people responding, those who lost weight on their own were generally more successful than those who participated in weight loss "programs." The most successful people were those who changed their eating and exercise habits. age and dieting - the younger the dieter, the better their chances are of keeping off the weight they lose. Obese children are more likely to maintain loss than are obese adults. eating disorders - include (1) anorexia nervosa, (2) bulimia nervosa, and (3) binge eating disorder. Binge eating disorder is, at present, not an official "DSMIV" diagnosis, it is in the "provisional" category, awaiting further research. eating disorders in general - are more common among certain groups such as: (1) models, (2) dancers, and (3) athletes. Core components of all the disorders are: (1) body dissatisfaction, (2) preoccupation with food, and (3) preoccupation with weight and body shape. Females outnumber males by about "10 to 1." anorexia nervosa - Is defined by the DSM-IV as including: (1) weight 85% less than normal or BMI below 17.5, (2) fear of being fat, (3) distorted body image, (4) cessation of at least three menstrual cycles "amenorrhea." There are two subtypes: (1) food restricting, and (2) binge-purging. Anorexics are typically from upper SES, European American, high achieving families. Some researchers, such as Hilde Bruch, think the disorder may be an attempt to gain "control" over their lives. Anorexia has the "highest mortality rate" of any psychiatric disorder. Treatment (typically cognitive behavior therapy) has a low success rate. The most common cause of death is from cardiac failure. Prozac may be helpful in preventing relapse. bulimia - Primary features, according to the DSM-IV, include: (1) episodes of binging, (2) sense of loss of control, and (3) inappropriate measure to compensate (i.e., binging). Bulimia differs from anorexia in that: (1) "impulsivity" appears to be a key factor, (2) prevalence does NOT differ by SES or ethnicity, (3) bulimics are of normal weight, and (4) the disorder only exists in the "Western" cultures or those influenced by Western cultures. binge eating disorder - The primary DSM criterion for this disorder is binging at least twice a week for at least six months. Characteristics include: (1) higher BMIs than the other disorders, (2) prevalence does NOT differ by SES or ethnicity, (3) personality disorder diagnoses are common, and (4) unlike Bulimia, it is not limited to Western cultures. hypoglycemia - A consequence of eating disorders. High sugar intake releases insulin which lowers blood sugar. This leads to cravings for more sugar and possibly another binge. damage to the teeth - repeated vomiting brings hydrochloric acid into the mouth where it wears away the enamel of the teeth. anemia - A consequence of eating disorders. A low level of red blood cells, leading to generalized weakness and lack of vitality. electrolyte imbalance - A condition caused by loss of essential minerals such as sodium,. potassium, and calcium. A consequence of purging. alkalosis - An abnormally high level of alkaline in the body caused by loss of hydrochloric acid during vomiting. Also a consequence of purging. treatment - for the eating disorders in general consists most often of cognitive behavioral therapy. Treatment of these disorders is usually only modestly successful.