Drug Recalls - Pharmacy Guild of Australia
advertisement

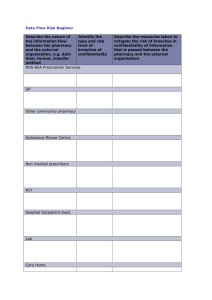
Community Pharmacy Roadmap Program Development Template Program/Service Quadrant Medicine Recalls A – Prescribed Medicines – Services and Programs 1. Program/Service Description a) Background A medicine is recalled from supply from the Australian market when there is an 'established deficiency in quality, efficacy or safety'. A recall might be initiated as a result of reports referred from a variety of sources, including: manufacturers wholesalers retail and hospital pharmacists research facilities medical practitioners and dentists. The Therapeutic Goods Administration (TGA) may also request a recall as a result of: analysis and testing of samples of therapeutic goods advice from an expert advisory committee information received from international regulatory authorities. 1 The current process followed is largely defined by the Uniform Recall Procedure for Therapeutic Goods (URPTG), established by the TGA. This procedure describes the stages of recall, including notification, crisis management, information requirements, an assessment of strategy, class and level of recall, communications, responsibilities of sponsors and recall coordinators and follow-up actions. A review of the role of community pharmacy in drug recalls was undertaken as part of the 4th Community Pharmacy Agreement. (4CPA) This review’s report, released in February 2010, found the URPTG made little mention of community pharmacy and that there was a lack of any standardised national recall procedures for the sector. This means that, beyond the initiation of the recall, performance of medicine recall tasks at the pharmacy level is reliant upon pharmacist’ professional responsibilities, rather than explicitly defined procedures.2 b) Brief Description Pharmacies play a key role in the quarantine and return of recalled medicines to the manufacturer, as well as the counselling of patients. A real-time internet based alert system for medicine recalls would assist pharmacies in this important role. This is consistent with the findings of the 4CPA report which suggests: “..the development of a system that sends an immediate electronic multi-modal message to all pharmacies” The report notes such a system “…could be included in dispensing systems, added to other existing data base systems such as Project STOP or be an entirely new product.” 3 c) Alignment with An effective and efficient medicine recall process aligns with the National Medicine Policy4, Government Policy with medicines needing to meet appropriate standards of quality, safety and efficacy. TGA Product Recalls: http://www.tga.gov.au/recalls/index.htm Nova Public Policy Pty Ltd: Review of the role of community pharmacy in drug recalls- Final report, 2 February 2010 http://www.health.gov.au/internet/main/publishing.nsf/content/3AFDB28CDC5C43A5CA25751400032D03/$File/Drug%20Recalls%20Revi ew%20Final%20Report%2020100202.pdf 1 2 3 Ibid. p7 4 http://www.health.gov.au/internet/main/publishing.nsf/Content/National+Medicines+Policy-1 1 d) Expected Outcomes for Government and Community Pharmacy From the government perspective, a real-time, standardised electronic alert system for recalls would mean the timely removal of recalled medicines across all pharmacies, meaning superior outcomes for public health. From the community pharmacy perspective, a uniform process to be followed for medicine recalls would maximise efficiency/simplicity, and ensure recall-related tasks were commensurate with any remuneration provided. e) Consumer Benefits An effective and efficient medicine recall process, supported by an internet-based real time monitoring and alert system, would minimise the risk to consumers. f) Who Performs the Service Pharmacists Pharmacy assistants The pharmacist will be involved with any professional aspects associated with the service, while pharmacy assistants will be involved with administrative functions. g) Collaboration with Other Health Care Professionals Will service delivery require any formal collaboration with other health care professionals? The pharmacist may need to collaborate with the prescriber after a medicine has been recalled to discuss alternative therapies for patients. 2. Implementation and Enablers a) Stakeholder Consultation Representative bodies from the following areas will need to be consulted in order to fully develop and implement a program: Consumer organisations Funders Government and regulatory bodies GP organisations and other prescriber groups Pharmacy organisations Pharmacy software vendors Product sponsor groups Professional insurers b) IT Requirements Is pharmacy software required to deliver this program? Yes. The current medicine recall processes rely substantially on facsimile as the mode of communication between pharmacies and others in the medicine recall chain. A real time monitoring and alert system that sends an immediate electronic message to all pharmacies would reduce the delays reportedly experienced with the current system. It could be included in dispensing systems or added to other existing data base systems such as for Project STOP5. c) Infrastructure and Staffing Is a private consultation area required to deliver this program? No. Is the program within the pharmacist’s/pharmacy assistant’s normal scope of practice? Yes. Is an additional pharmacist likely to be needed? No. 5 d) Training What additional formal training is likely? Initial instruction on any systems that are developed will be required. e) Supporting Will a QCPP standard be required? http://www.projectstop.com.au/ 2 Standards, Procedures and Templates / Checklists Yes. An update to existing Quality Care Pharmacy Program (QCPP) standards may be required to accommodate aspects of this service. Will professional guidelines and/or standards for pharmacists be required? Yes. Are there any national guidelines which need to be taken into account in developing the program to ensure consistency with best practice? Yes. The URPTG should be expanded to include the role of community pharmacy. f) Legislation / Regulation Implications The management of safety and quality in the medicine supply (and recall) system in Australia is largely provided via agreements, protocols and procedures between sponsors and the TGA including the URPTG. It is unlikely that either Commonwealth or State/Territory legislation should need to be changed. 3. Funding Funding options Possible funding options include: Commonwealth funding – through an incentive scheme (e.g. via QCPP) User-pays – sponsors remain responsible for costs associated with recalls, and pharmacies are reimbursed for direct and indirect costs incurred, such as customer counselling Has any funding for this program been secured? No. 4. Timelines Timelines □ Established community pharmacy practice √ Immediate to short-term implementation (< 30 June 2015) □ Medium-term implementation (1 July 2015 to 30 June 2020) □ Longer-term implementation (> 1 July 2020 ) 3