Presentation - Dr - Dartmouth
advertisement

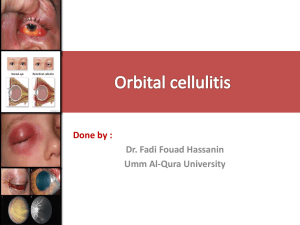
December 2004 Presentation - Dr. Bethany Ames, Pediatric Resident This patient is a 14-year-old male with a complaint of left eye pain. He reported that the previous day he had been hunting, when he developed a sudden headache over his forehead. He vomited several times and continued to experience a throbbing headache. He experienced chills with rigors and woke a few times during the night due to pain. When he awoke in the a.m., his left eye was swollen shut and the pain had localized to behind this eye. He had double vision and blurriness. He presented to his PCP where exam revealed fever with periorbital edema and erythema. Labs were significant for WBC of 12,200, 80% granulocytes. He was treated with IM ceftriaxone and acetaminophen with codeine. Past medical history remarkable for recurrent staphylococcal skin infections and history of obesity. He had had two molars extracted six months previously and was scheduled to have further dental work. Recent medications were only those used for pain over the last two days. Immunizations up to date. Family history most significant for recent death of his father at age 47 with diabetes and cardiovascular disease. Social history: Moved to this area two years ago from Florida. He is in 9 th grade and gets A’s and C’s. Review of systems negative for preceding sinus pain, sinusitis and negative for seasonal allergies. Denied any trauma. He does not wear contacts or glasses. Denies recent dental pain. Physical Examination Vitals T 38.3, HR 97, RR 16, BP 139/80 Weight 124 Kg Gen Pt was in obvious discomfort HEENT Left eye with marked edema and erythema of both lids. Exophthalmos and downward displacement of globe. Injected and edematous conjunctiva. Limited ocular ROM. Comments: Remainder of exam normal except for dental decay, obesity and acanthosis nigricans. Sinus and orbital CT scan was done on admission. Findings were consistent with significant left pan sinusitis, orbital cellulitis that included free air in the globe and a communicating tract between the oral cavity and sinus cavity. Course: Started on ampicillin-sulbactam (Unasyn) for gram positive and anaerobic bacteria most likely to cause sinusitis. He was also given a 48 hr course of dexamethasone and monitored closely for hyperglycemia. After the CT he was taken to the OR for surgical debridement and decompression, ethmoidectomy and orbital exploration. The orbitectomy revealed green foul smelling purulent discharge. Drains were placed in the orbit and sinus. Post operatively patient reported immediate resolution of pain. Two days following the initial surgery, patient returned to the OR to have two maxillary molars extracted. At that time a large infected maxillary cyst was noted and excised. In the immediate post op period, he remained afebrile. Diagnosis: Dental abscess with oral antral fistula leading to sinusitis. Sinusitis extended to orbital cavity resulting in orbital cellulitis. Cultures of orbit and sinus grew Streptococcus milleri group and coagulase negative Staph species. Discussion - Dr. John F. Modlin “Orbital cellulitis is a serious acute bacterial infection of the ocular orbit which contains the extraocular muscles and fat. Although the interior structures of the eye are spared of infection, sight may be threatened from increased ocular pressure resulting from infection within the closed bony orbit. It invariably results from direct extension of infection from the adjacent ethmoid sinus that is separated from the orbit by a very thin layer of skeletal bone (the lamina papyracea). Many cases occur in older children and adolescents who often have acute pansinusitis like this patient. Thus the etiologic bacteria are the same as those associated with acute sinusitis, which include S. pneumoniae, H. influenzae, Moraxella catarrhalis, Staphylococcus aureus, and oral aerobic and anaerobic streptococci (including S. milleri). This case has an added twist: the sinus infection probably began in the ipsilateral maxillary sinus as a complication of a periapical dental abscess. Orbital cellulitis is both a medical and a surgical emergency. Treatment includes administration of a broad spectrum antibiotic expected to cover the organisms listed above, and rapid surgical drainage of the sinuses. Orbital drainage is also carried out in cases where the CT scan demonstrates an abscess cavity within the orbit. Otherwise, infection of the orbit generally clears on appropriate antibiotic therapy as long as the sinuses are drained.” References: Starkey CR, Steele RW. Medical management of orbital cellulitis. Ped Infect Dis J 2001; 20:1002-1005. Goldberg F, Berne AS, Oski FA. Differentiation of orbital cellulitis from preseptal cellulitis by computerized tomography. Pediatrics 1978; 62:1000-1005. Page 1 of 2 December 2004 New Provider Profile: Marcus S. Shaker, MD Welcome to Dr. Marcus S. Shaker, who has recently joined CHaD as an Assistant Professor of Allergy. Dr. Shaker graduated from James Madison University and earned his medical degree at University of Virginia School of Medicine. He completed his residency in Pediatrics and his fellowship in allergy/asthma at the University of Virginia Health System. Dr. Shaker's research interests include characterized activated (CD-69 positive) lymphocyte cytokine responses in wheezing children with community-acquired human rhinovirus infection, and he has published several articles in the Journal of Allergy and Clinical Immunology. "My philosophy of care involves a patient centered, evidence-based approach to allergy in a child-friendly clinic environment,” says Dr. Shaker. “I always try to treat others the way I would want them to treat me if the roles were reversed.” Conferences and Announcements: For more information, call 603-650-3436 December 3, 2004: CHaD Currents – Hot Topics in Children’s Health – Newborn Hearing Screening (Christine Rosenwasser, MD), Common Endocrine Diseases (Kyle Landt, MD), Slipped Capital Femoral Epiphysis (Brian Carney, MD), and Evaluation of Sports Injuries in Children (Kenneth Weintraub, MD); at D-H Manchester. March 3-6, 2005: The 15th Dartmouth Pediatric Conference: Contemporary Issues in Office Pediatrics will focus on Adolescent Confidentiality, Childhood Obesity, and Childhood Depression, among many other topics. We will return to the Woodstock Inn and Resort in Woodstock, Vermont. Pediatric Grand Rounds - Wednesdays at 8AM, Auditorium E at DHMC December 1: “Core Binding Factors in Hematopoiesis & Leukemia” - Nancy A. Speck, Ph.D., DHMC December 8: “The Red Scaly Baby” - James Dinulos, M.D., DHMC December 15: “Fostering Health: Caring for Children in Foster Care” - Maryellen Gusic, M.D., Hershey Medical Center December 22: No Grand Rounds--Happy Holidays! December 29: No Grand Rounds--Happy Holidays! Respiratory Viral Activity - from the DHMC Virology Lab Respiratory virus activity at DHMC by culture and antigen detection Number of Positives 10 9 8 7 6 5 4 3 2 1 0 RSV Parainfluenza 3 Adenovirus Influenza A 12/18/04 12/4/04 11/20/04 11/6/04 10/23/04 10/9/04 9/25/04 9/11/04 8/28/04 8/14/04 7/31/04 7/17/04 7/3/04 6/19/04 6/5/04 5/22/04 5/8/04 4/24/04 4/10/04 3/27/04 3/13/04 2/28/04 2/14/04 1/31/04 1/17/04 1/3/04 Influenza B Subscription Information Editor: Dr. Rebecca L. Rich, Pediatric Chief Resident Managing Editor: Margaret Rose Minnock, MBA Editorial Board: Drs. Norm Berman, Sam Casella, Sara Chaffee, Leslie Fall, Dan Levin, George Little, John Modlin, Richard Nordgren, Dennis Stokes, Jodi Wenger CHaD Morning Report is intended to provide the reader with interesting and helpful clinical information on a recent case selected from one of CHaD's pediatric inpatient units. Physicians may claim Category 2 credit for this activity. If you would like to receive this report on a monthly basis, or to unsubscribe, please go to www.dhmc.org/goto/CHaDMorningReport, where current and back issues will be maintained, or call the Connection Line at 1-866-DHMC DOC (346-2362). Page 2 of 2