Paediatric Clinical Guidelines
advertisement

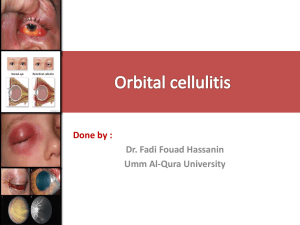
Paediatric Clinical Guidelines Infectious 8.1 February 2002 GUIDELINES FOR THE MANAGEMENT OF PERIORBITAL CELLULITIS/ABCESS Indications for Admission - The majority of patients with periobital swelling Diplopia CNS signs or symptoms Reduced visual acuity Reduced light reflexes or swinging light test Patients who are toxic or systemically unwell Proptosis Ophthalmoplegia Patients in whom it is not possible to examine the eye The only patient suitable for discharge is: someone with minimal upper lid oedema, normal eye examination and with none of the above. Augmentin has a suitable spectrum of activity for these patients. Treatment Plan 1. 2. 3. 4. Arrange an ophthalmological opinion Arrange an ENT opinion IV access – blood cultures Intravenous Cefuroxime (100 mgs/kg/day in 3 doses) and Metronidazole (7.5 mgs/kg tds, max 400 mgs) with nasal Ephedrine 0.5% nose drops three times a day in the head back, nostril up position 5. Don’t forget to give adequate analgesia to allow a proper assessment 6. The following should be done twice daily following ophthalmology advice: a. Assess colour vision and acuity. This must be done with the eye open and on the eye in question on its own. If the patient has glasses and these are not available then test acuity through a pinhole. b. Test for eye movement to see if there is any ophthalmoplegia c. Test the pupil reflexes If there is gross proptosis, ophthalmoplegia or concern these observations should be done on an hourly basis. Indications for CT 1. Central symptoms or signs, eg drowsy, had a fit, cranial nerve lesion, headache and vomiting 2. Gross proptosis 3. Ophthalmoplegia Page 1 of 4 4. 5. 6. 7. Deteriorating acuity or colour vision or unable to evaluate vision Bilateral periorbital oedema (? Cavernous sinus thrombosis) No improvement or deterioration at 24-36 hours Swinging pyrexia not resolving within 36 hours N.B. If vision is deteriorating rapidly the orbit must be decompressed. This should be done within an hour and if imaging cannot be done within this time then do not wait for it. References 1. Wald E R, Pang D, Milmore G J, Schramm V L, (1981) Sinusitis and its Complications in a Paediatric Patient. Paediatric Clinics of North America. 28 (4) 777-796 2. Brook I, Friedman E M, Rodriquez W J, Controni G, (1980) Complications of Sinusitis in Children. Paediatrics. 66, 568-572 3. Wagenmann M, Naclerio R, (1992) Complications of Sinusitis. J Allergy Clin Immunol. 90, 552-4 4. Uzcategui N, Warman R, Simth A, Howard C W, (1998) Clinical Practice Guidelines for the Management of Orbital Cellulitis. L Pediatr Ophthlamol Strabismus. 35, 73-79 5. Rubin S E, Rubin L G, Zito J, Goldstein M N, Eng C, (1989) Medical Management of Subperiosteal Abscess in Children, J Pediatr Ophthalmol Strabismus. 26, 21-26 6. Schramm Jr V L, Curtin H D, (1982) Evaluation of Orbital Cellulitis and Results of Treatment. Laryngoscope. 92, 732-738 7. Davis J P, Stearns M P, (1994) Orbital Complications of Sinusitis: Avoid Delays in Diagnosis. Postgraduate Med J. 70, 108-110 8. Chandler J R, Langenbrunner D J, Stevens E R, (1970) The Pathogenesis of Orbital Complications in Acute Sinusitis. Laryngoscope. 80, 1414-1428 Page 2 of 4 Parent Information Sheet Your child has been diagnosed as having peri – orbital cellulitis (an infection in front of the eye). Most of these infections can be safely treated at home with antibiotics given by mouth. If antibiotics by mouth do not start to improve the swelling within 24 hours, your child will need to come into hospital so that antibiotics can be given directly into a vein. It is important that he / she completes the course of antibiotics provided by the doctor. If he / she becomes more unwell with headache, vomiting, increased drowsiness then he / she will need to be seen quickly to make sure more serious infection isn’t present. Arrangements need to be made for your GP to review your child in the next 24 hours to ensure that the infection is getting better. You may be the best judge that the eye swelling has reduced. Page 3 of 4 PAEDIATRIC CLINICAL GUIDELINES ISSUE: VERSION: FINAL Title: Management of Periorbital Cellulitis/Abscess Author: Job Title: Professor N S Jones Professor in Otorhinolaryngology First Issued: Date Revised: Review Date: Document Derivation: i.e. References: Consultation Process: Dr Maria Atkinson – Paediatric Specialist Registrar Dr Stephanie Smith – Consultant Emergency Paediatrician Clive Newman – Paediatric Pharmacist Included in document February 2002 February 2005 Ratified By: Paediatric Clinical Guidelines Committee Chaired By: Consultant with Responsibility: Dr Stephanie Smith Distribution: All wards QMC and CHN Training issues: Included in Induction Programme Audit: This guideline has been registered with Nottingham City Hospital NHS Trust and QMC Clinical Guidelines Committee. However, clinical guidelines are ’guidelines’ only. The interpretation and application of clinical guidelines will remain the responsibility of the individual clinician. If in doubt contact a senior colleague or expert. Caution is advised when using guidelines after the review date. MANUAL AMENDMENTS RECORD (please complete when making any hand-written changes/ amendments to guideline and not processed through guideline committee) Date Page 4 of 4 Author Description