P-15 Drugs & Medicines - Administration v06
advertisement

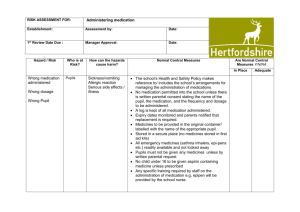
Cornford House POLICY NO: P-15 Date Reviewed Issue No: January 2016 7 Page 1 of 4 HANDLING & CONTROL OF DRUGS: (2) ADMINISTRATION This Policy defines the arrangements for ensuring that residents receive only their own medication (exception: Household Remedies) which are safely stored, recorded and properly administered by trained staff: Medicines Administration Procedure All staff must comply with the following procedure for the administration of medicines. 1. Before you begin you must wash your hands thoroughly. Then assemble all the equipment required: medicines trolley, the MARs folder, a sufficient supply of medicines pots, medicines spoons, oral syringes, tablet cutters, gloves, water, glasses, paper towels and container for collection of used equipment. Medicines should be administered to each resident in turn. 2. Using the MARs read the list of medicines presented and note which medicines are indicated to be given at this time. 3. Select the first medicine due to be given and mark the record. This will confirm the correct medicine by presenting the number of tablets / capsules to administer. 4. Check this number against the label on the medicine container; if there is a discrepancy a check should be made with the Pharmacy or person-in-charge before giving the medicine to the resident. Having checked that the medicine is correct and checked its expiry date, remove it from its pack directly into a medicines pot (tablets and capsules). If the tablet or capsule is in a bottle then it can be gently tipped into the lid before transferring to the medicines pot. Tablets and capsules should never be dispensed into your hand. Bottles of liquid preparations should always be shaken well before measuring a dose. Oral liquid medicines should be measured using a medicines measure for doses of 5mL or more. For smaller doses, an oral syringe should be used because the medicines measure is not accurate enough. If the medicine dose requires the tablet to be cut in half, use the tablet cutter to half the tablet appropriately. Please note that the Pharmacy will not supply pre-cut tablets. 5. Select the next medicine that is due for administration and repeat the step in 5. 6. Find any other items to be administered such as creams or eye drops. Offer any “when required” or “prn” medicines that the resident has been prescribed according to their care plan. 7. Once all items for the first resident have been potted, they should be taken directly to the resident and administered via the prescribed route immediately. Medicines should not be left with the resident to “take later”. Cornford House POLICY NO: P-15 Date Reviewed Issue No: January 2016 7 Page 2 of 4 HANDLING & CONTROL OF DRUGS: (2) ADMINISTRATION 8. Account for all of the medicines immediately after administration 9. Please note that medicines refused or not taken should be accounted for by selecting the appropriate code. Medicines that have been “spat out” or “spilled” can be placed in the “refused medicines” pots supplied by the Pharmacy . 10. Repeat procedure from step 2 with all other residents. Medication must not be altered in any way i.e. crushing, unless there is an authorisation letter from the GP. Administration of Controlled Drugs Administrations of controlled drugs must follow the same procedure as above. However the following additional procedure must be complied with: The person administering the medicines must take the CD from the CD cupboard and check against the medicine’s record on the MARs Return remaining stock to CD cupboard and lock it Administer the medicine according to procedures above. A witness will be required to confirm the administration on the MARs. Please note that this person does not need to be accredited for administering medicines, but must be approved for witnessing medicines administration. Complete CD register in full ensuring the stock balance is correct. A witness will be required to check and sign the CD register. Records of Medicines Administered It is a requirement to keep records of medicines administered. The historical records of medicines administered over the previous three years will be made available to the care home through the on-line service. These records must be printed at the end of each month and kept as a back up and to show CQC or PCT inspectors. The records will contain the following information: Name and date of birth of the resident, and their room number if appropriate. Details of any allergies that the resident may have. Name, strength and route of all medicines. Frequency and times of administration. Any special instructions such as “before food” Codes to explain reasons for omission. As required medication should have information on maximum dosage and frequency. Medication Errors Medication errors are almost never the result of a single, isolated human error. Instead, they result from multiple small breakdowns in the systems for handling drugs. For this reason this Cornford House POLICY NO: P-15 Date Reviewed Issue No: January 2016 7 Page 3 of 4 HANDLING & CONTROL OF DRUGS: (2) ADMINISTRATION policy makes a requirement for all medication errors to be investigated by the care home manager. The learning from these errors must be communicated to all members of staff. If an error occurs the following steps must be carried out: The incident must be reported to the care home manager. The medication error should be documented on the medication incident form, a copy should be stored with the resident’s care plan. The care home manager should seek the advice of a pharmacist or GP as to the seriousness of the medication error and the affect on the resident. The resident’s GP should then be informed and the actions recommended must be implemented and documented. The need to report the error to CQC should be discussed with the owner and where necessary it should be reported via the notification form. If the medication error is suspected to be a result of a dispensing error or a failure in service delivery, the Pharmacy will carry out an internal investigation and respond to the care home manager by email within 7 days of receiving news of the incident. Attempting to conceal any error may result in a disciplinary action The following are strategies that care home managers should implement to reduce the risk of occurrence of medication errors: Ensure that staff administer medicines use the MARs Lighting in medication dispensing areas must be adequate Members of staff who administer medicines must be shielded from interruptions and distractions Ensure room temperature in medication storage areas and the refrigerator are kept within safe guidelines Ensure medicines are arranged in a manner that fosters efficient workflow Ensure all handwritten prescriptions are legible Ensure all changes to medication therapy are communicated to the Pharmacy Ensure wherever possible that residents are aware of all medicines they are prescribed, and the rationale for their prescription Ensure that every medication error is individually analysed by the Home Manager to determine the root cause of the error, regardless of the outcome. Drug and Safety alerts All care homes must be registered for receiving drug and device safety alerts from the MHRA. The care home manger is required to keep records of the receipt of all safety alerts and actions taken as a result of the alerts. Upon receipt of the safety alert the care home manager or a designated person must take responsibility and decide if further action is required. The following procedure must be Cornford House POLICY NO: P-15 Date Reviewed Issue No: January 2016 7 Page 4 of 4 HANDLING & CONTROL OF DRUGS: (2) ADMINISTRATION carried out: • • • • • • • • • The safety alert must be brought to attention of all relevant staff. Recommended remedial action must be implemented within the time scale specified. In some cases no action will be necessary or the safety alert will not apply. In these cases the safety alert must be signed to indicate that it is not applicable and recorded. If the bulletin does apply then action must be taken. The action taken must be recorded and attached to the Alert and signed by the designated person/s. In all cases the care home manager must report the action taken to the Quality Assurance Manager (or equivalent). Further information can be obtained through the Department of Health, MHRA Document “Reporting Adverse Incidents and Disseminating Medical Device Alerts”. (January 2005). Management of errors in administering drugs In the event of an error being identified in administering drugs it must immediately be reported to the Manager. The resident must be examined to assess to what extent the error has been detrimental to them. The resident’s GP must be informed immediately. Details should be recorded in the Drug Error Book kept in the Clinic Room in each Unit and in electronic daily report A full investigation will be carried out and details recorded. An action plan will be put in place detailing the necessary procedures and training required to avoid a recurrence. The employee concerned will be interviewed and disciplinary action will be taken if it is deemed necessary. Reference should be made to the Nursing Midwifery Council Guidelines and the Care Quality Commission Inspection office. Covert Administration IT IS NOT common practise to administer medication covertly. We need to define when medications can be administered covertly in the residents ‘best interest’ Medication may only be administered covertly in line with the principles of MCA as follows: Residents must have been reviewed by their Consultant / GP. It must have been agreed with them as to which medication maybe administered covertly There must be an authorisation letter from the GP Medication administered covertly should be for the shortest period possible Care plan must include all the details.