3. Plasma Membrane
advertisement

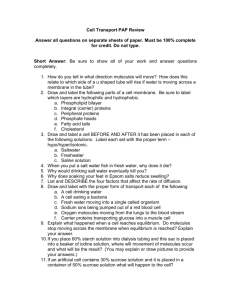
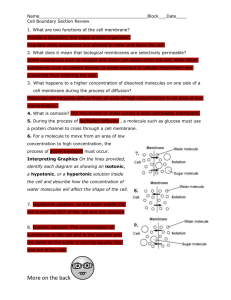
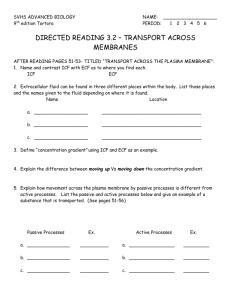
Plasma Membrane Dynamics and Cell Transport Mechanisms Plasma Membranes are mostly Lipids and Proteins arranged in a Fluid Mosaic Model A typical cell membrane has a composition of: Lipids: 40-60% - arranged in a double lipid bilayer. Protein: 30-50% - proteins which are inserted either partly or completely through bilayer. Carbohydrate: 5-10% - carbohydrates which attach to extracellular fluid (ECF) side. These percentages can vary significantly depending on the specific type of cell in the body. Plasma membrane ECF ICF Nucleus Cytoplasm with organelles Figure 1. This is the typical diagrammatic representation of a eukaryotic cell. The extracellular fluid (ECF) is kept separate from the intracellular fluid (ICF) by the plasma membrane. General Function of Plasma Membranes 1. Physical Barrier: The plasma membrane (PM) acts as a barrier; it separates the inside of the cell, containing ICF, from the outside of the cell, containing ECF. It creates the boundary of the cell and isolates it from other cells and structures. 2. Regulation of Exchange: Anything that goes into or out of a cell must do so by crossing the plasma membrane. Exchange with the environment occurs across this membrane, either by slipping through the membrane or by being transported across by protein channels or protein carriers. 3. Structural Support: Structural proteins are tethered to the internal or intracellular aspect of the plasma membrane in order to create the internal structural support for the cell. This internal framework is referred to as the cytoskeleton of the cell. For example, this helps create the shape of cells, like the distinctive biconcave disc shape of the red blood cell. 4. Communication and Cell ID: Signals from the external environment of the cell are transferred into the internal compartment across the plasma membrane. This often involves receptors that sit on the external aspect of the plasma membrane to receive the signal. Signal molecules are called ‘ligands’ and they bind to receptors, much like substrates bind to enzymes. There are also molecules (glycoproteins and glycolipids) which attach to the external surface of the plasma membrane to help identify the cell as self. For example, these flags or markers are what make up the blood typing of a red blood cell (A, B, AB or O). Membrane Lipids 1. Phospholipids - usually about 75% of lipid content. The polar glycerol-phosphate head of a phospholipid is the hydrophilic end and a nonpolar fatty acid tail is the hydrophobic end. The entire molecule is amphiphilic, meaning it can mix with both water and lipid environments. The phospholipids are arranged in two rows, called the lipid bilayer and this functions as a barrier that only lipid-soluble molecules can penetrate. They also provide a framework for membrane 2 proteins. Some lipids are involved in cellular communication. Some common phospholipids found in plasma membranes include phosphatidyl choline and sphingomyelin. 2. Cholesterol - usually about 20 - 30% of lipid content. This 4 ringed lipid structure inserts into the hydrophobic center with the nonpolar fatty acid tails. The more cholesterol in the plasma membrane the more insulative the membrane will be. For example, the myelin sheath membrane (which insulates axons of nerve cells) is about 30% cholesterol, while other mammalian cell membranes may be about 20% cholesterol. Cholesterol helps to stabilize the plasma membrane. It functions to keep membranes impermeable and yet flexible. Membranes with higher cholesterol concentrations are less permeable to ions, water, and other small molecules. Presumably cholesterol blocks the openings between phospholipid tails through which these small molecules could otherwise pass. Mammals maintain a relatively constant Tb, so the "plasticizing" effect of cholesterol is not as important as it is in poikilothermic animals and plants that cannot maintain a constant body temperature. 3. Glycolipids – usually about 5% of the lipid content. The prefix glyco means ‘glucose’ or ‘sugar’, so a glycolipid is a small amount of a sugar attached to a large amount of lipid. Glycolipids are found on the external surface of the plasma membrane and act as a cell markers. This helps identify the cell as self to defense cells of the body. Other Phospholipid Arrangements 1. Micelles are small droplets with hydrophobic tails forming the interior; the hydrophilic heads form the exposed boundary. Important in digestion and absorption of fats in digestive tract. 2. Liposomes are larger hollow spheres with phospholipid bilayer walls. Their hollow core can be loaded with water-soluble molecules. Can be used as a drug delivery system. Membrane Carbohydrates Plasma membrane carbohydrates attach to both lipids and proteins. The Glycocalyx is a protective layer on cell surface formed by Glycoproteins - when glucose attached to membrane proteins and Glycolipids - when glucose attached to membrane lipids. The carbohydrates of the glycocalyx play a critical role in identifying cells; for example, the carbohydrates of the glycocalyx in human blood cells differentiate the main ABO blood groups from one another. Membrane Proteins 1. Associated Proteins Also termed peripheral or extrinsic proteins. They are attached loosely to membrane-spanning proteins or to polar regions of phospholipids. They do not span the plasma membrane! 2. Integral Proteins and Membrane-Spanning Proteins Also termed intrinsic proteins. These are tightly bound into the phospholipid bilayer. Some integral proteins only extend partway into the membrane, others are membrane-spanning. Membrane-spanning proteins have segments that cross the membrane multiple times. Loops extend into extracellular and intracellular regions. Carbohydrates attach to extracellular loops and phosphates attach to intracellular loops. When amino acids are linked to each other, they can form an -helix that has an exterior layer of nonpolar side groups and a central core composed of the polar amino and carboxyl groups. This ties the protein so firmly to the membrane that it can only be freed by disrupting the phospholipid bilayer with detergents. 3 Membrane receptors, transporters, and enzymes are grouped into families according to how many membrane-spanning regions they possess. Below are some examples: 1) The voltage-gated K+ channel has six transmembrane segments. 2) The voltage-gated Na+ and Ca2+ channels have four associated segments (domains), each with six membrane-spanning regions. 3) The ATPase transporters of eukaryotic cells have 8-10 membrane-spanning regions. 4) The G-protein-linked membrane receptors all have seven transmembrane segments, as do the 2adrenergic and rhodopsin receptors. Originally it was thought that membrane proteins all floated freely within the lipid layer of the membrane. However, it has been shown that some proteins are immobile, held in place by cytoskeleton proteins. Restriction of protein movement allows membrane polarity, which can be seen in transporting epithelia. Other proteins are mobile and move under the direction of cytoskeleton. For example, rhodopsin, the protein pigment that absorbs light in the retina, rotates in place, somersaulting at a rate of 60° every 10 seconds. 3. Glycoproteins As mentioned above, the prefix glyco means ‘glucose’, so a glycoprotein is a small amount of a carbohydrate (sugar) attached to a large amount of protein. If the molecule is called a proteoglycan, then there is more sugar (glyco) than protein. Glycoproteins are also found on the external surface of the plasma membrane and act as a cell markers. Function of Plasma Membrane Proteins The proteins that are associated with the plasma membrane have an expansive range of roles. 1. Structural Elements 2. Cell Adhesion Molecules 3. Enzymes 4. Receptors 5. Transporters 1. Structural Proteins – Theses link cytoskeleton and membrane to maintain cell shape, e.g., microvilli, red blood cells. The characteristic shape of the red blood cell is due to an extensive cytoskeleton that pulls the cell membrane into a biconcave disc shape. In diseases such as hereditary spherocytosis, defects in cytoskeletal proteins produce abnormally shaped red blood cells that are unable to move normally through the circulatory system. 2. Cell Adhesion Molecules - Form part of the cell-to-cell connections holding tissues together. Membrane-spanning proteins link the cytoskeleton to the extracellular matrix. The most common fibrous protein that attaches a cell to adjacent cells is collagen! 3. Enzymes – Membrane associated enzymes act as any other enzymes do but are fixed to the plasma membrane. Chemical reactions can take place on either membrane face, i.e. on the extracellular or intracellular surface. For example, enzymes on luminal surface in small intestine cells (extracellular) digest peptides and carbohydrates. Enzymes on the intracellular surface, such as adenylyl cyclase, play an important role in signal transduction. 4. Receptors – These act as receivers for the body's chemical signaling system, with each receptor being specific for a certain type or family of signal molecule. A ligand is any molecule binding to a receptor. Ligand binding usually triggers another membrane event, this can be signal transduction (e.g., hormone binding) or directly lead to an ion channel opening or closing (ionotropic effect). 4 5. Transporters - Many molecules require the use of transporters to cross cell membranes. Most lipophobic (can also be termed hydrophilic) molecules, such as smaller carbohydrates, amino acids, peptides, proteins, and charged particles such as ions, must have assistance from membrane proteins in order to get into or out of cells. All of the above listed functions of plasma membrane proteins are very important. In the next stage that follows, however, we are going concentrate on the role of plasma membrane proteins as transporters in the body and the various mechanisms by which they move molecules from one side of the plasma membrane to the other. There are 2 Categories of Protein Transporters: Protein Channels and Protein Carriers Protein Channels Protein channels are well named; they are much like little water-filled channels, forming a passageway that directly links the ECF to ICF. The narrow diameter of protein channels restricts passage through them to small sized molecules, mostly water (H2O) and ions (K+, Na+, Cl- and Ca2+). Electrical charges lining the inner channel may restrict the movement of some molecules; therefore they can be very specific as to what they allow to travel through them. This mode of transport is very fast, much faster than protein carriers because there is no need for the binding of the substrate as in protein carriers. ECF ICF Will this get through? Yes, it is small enough. protein channel Will this get through? No, it is too big. plasma membrane Open channels spend most time in the open configuration and are also called pores. Other channels are gated and spend most time in a closed state. Three Types of Gated Ion Channels: The protein channels that have gates that can open or close are called gated ion channels. There are three types of gated channels that we will explore, and they differ in the ‘trigger’ that opens or closes the gate, they are: 1. Chemically Gated Channels: triggered by specific ligands (chemicals) to open or close channel. 2. Voltage-Gated Channels: triggered by electrical changes across cell to open or close channel. 3. Mechanically Gated Channels: triggered by distention or physical force to open or close channel. Some gated channels remain open and the molecules leak across the channel, these are often called "leaky channels". The normal permeability of cells to Na+ and K+ is due to such leak channels. 5 Protein Carriers The second type of protein transporters are called protein carriers. These never form a direct or continuous passage between the ECF and the ICF. They have a binding site (like enzymes) and will only transport specific molecules that match this site. Once the molecule binds to the site, the protein carrier undergoes a conformation (shape) change. It can rotate, or close one end while it opens the opposite, thus carrying the molecule across membrane. This mode of transportation is slower than protein channels, as they need to bind the substrate and change shape while moving substrates. ECF ICF Will this get through? Protein carrier Yes, it has the right shape for binding site. Typically, carriers are used for transporting larger, polar molecules. A perfect example is glucose. Glucose has a MW of 180, so it is a larger molecule, but not massive like starch or albumin. It is also a polar molecule, meaning it is soluble (mixes) in water. Amino acids are another good example of molecules moved by carriers. Properties of Protein Carrier Mediated Transport Because of the way that protein carriers work, their transport exhibits saturation, specificity, and competition. Specificity Protein carriers move only one type or family of closely related molecules. For example, GLUT transporters move glucose, mannose, galactose, and fructose across membranes. They are specific for naturally occurring 6-carbon monosaccharides. Other carriers will transport amino acids, and there can be up to 20 different types of carriers, each specific for the 20 different amino acids the human body uses. Competition Carriers have preference (or affinity) for certain molecule(s). This can result in competition for the binding site between various molecules. For example, maltose is a disaccharide made of 2 glucose molecules, so one end of the maltose could try to occupy the binding site for a glucose transporter. Although it can bind, typically it will not be transported in the process, it is not the right shape overall. Thus in this case, maltose would be a competitive inhibitor for glucose transport. Saturation Saturation occurs when a group of protein carriers are transporting the substrate at its maximum rate, with all carriers occupied. Saturation will depend on the number of available carriers and substrate concentration. Cells can sometimes increase or decrease the number of available carriers to control substrate movement. As the substrate concentration increases, transport rate increases until the carriers become saturated. At this stage they are at their maximum transport capacity and cannot move things across the membrane any faster. An interesting consequence of saturation can be seen in the transport of glucose in the kidney. Normally, you should not find any glucose in your urine. If you do, it can be a sign of diabetes mellitus. However, if you were to consume large quantities of glucose, say by eating too many chocolates from your valentine gift, you may have glucose in your urine that is not due to a disease state (not yet anyway!). The glucose carriers in your kidney tubules can become saturated due to the abnormally high amounts of glucose being filtered by your renal system. If the carriers reach their maximum and more glucose is still in the filtrate, it will end up in the urine due to protein carrier saturation. 6 MOVEMENT ACROSS MEMBRANES You may have heard plasma membranes described as selectively or semi-permeable membranes. This means that some molecules can get across and some molecules cannot. The membrane composition determines which molecules move across. Permeable molecules can cross membrane by any method. Impermeable molecules cannot cross cell membrane. General Factors Influencing Molecule Permeability Although the components of a plasma membrane can vary, the properties of a given molecule will have a large effect on whether is passes through the plasma membrane easily, or if it needs assistance or if it cannot pass at all. 1. Size of molecule – smaller molecules can more easily pass through than larger. 2. Polarity or lipid solubility of molecule – lipid soluble molecules pass through more easily than polar. 3. Charge of molecule – uncharged molecules pass through more easily than charged. The permeability of a molecule can be influenced by all three of these factors, not just one. For example, water (H2O) is a polar molecule, that is, it is insoluble (does not mix) in lipids. This would tend to make it less permeable, since the phospholipid bilayer creates a significant barrier to polar substances crossing the membrane. However, the molecular weight (MW) of H2O is only 18, thus it is very small and for this reason can easily pass through most cell membranes in the human body. Ions are commonly very small, but they are charged particles and cannot pass directly through membrane by simple diffusion, they would require a protein channel, they would require a protein channel. At the other end of the spectrum, just because a molecule is fairly large does not mean it cannot pass directly through membrane by simple diffusion; relatively larger lipophilic substances can cross directly through membrane by simple diffusion, as the lipid bilayer is not a barrier. Very large molecules or a large amount of substance will typically require membrane transportation in a vesicle (see below). There are 2 ways a molecule can transported across a cell membrane: Passive & Active 1. Passive Transport: does not require energy (ATP). Movement down a gradient. 1) Diffusion 2) Facilitated diffusion 3) Filtration 1) Diffusion Diffusion is the net movement of molecules from an area of higher concentration to an area of lower concentration. In other words, the molecule is moving down its concentration gradient. This is a passive transport mechanism. Getting in a kayak and going down stream with the river is an example of passive transport. No energy expenditure is required; you can just sit there and be moved down stream. In the body, the net movement of molecules continues down its gradient until equilibrium is reached. Diffusion can occur in open regions or across a partition such as a membrane. Factors that Effect the Rate of Diffusion Diffusion is a very common and important mode of transport in the human body. The oxygen (O2) that enters our blood stream from our lungs does so by simple diffusion. A very important issue in human physiology is what factors affect the rate of diffusion of a molecule from one side of a plasma membrane to the other. Listed below are some of the important factors that affect the rate (how quickly) diffusion takes place. 7 Some factors that effect the rate of diffusion: a. Size of the molecule (as indicated by its MW) – smaller = faster b. Distance – shorter = faster c. Temperature – warmer = faster d. Surface area of membrane – greater = faster e. Thickness of barrier – thinner = faster f. Steepness of concentration gradient – greater = faster As we continue in physiology, all of these factors will be revisited in the various organ systems. 2) Facilitated Diffusion Some molecules that are polar or too big to use simple diffusion to get across a membrane can use protein carriers to move down their concentration gradient. This requires no energy. The molecules must bind to the membrane carrier (as discussed above), so in this way in needs the ‘help’ of a carrier to move down its gradient across the membrane. As long as it is going down its concentration gradient, it is still diffusion. The term ‘facilitated’ indicates that the molecule is getting some assistance. As we have seen, this process is also prone to specificity, competition and saturation. 3) Filtration Filtration is the net movement of water and solutes across a membrane due to the force of hydrostatic pressure. Hydrostatic pressure can be defined as the force of a fluid on the walls of its container. It can also be described as the force of gravity on a fluid. For example, if you place ground coffee on a paper filter and pour water over the top of it, the filter allows water and small solutes to pass through, but not the bigger coffee grinds. What you get on the other side is a filtrate of what was above, that is, anything small enough to pass through the holes of the filter, thus the term ‘filtration’. In the human body, the hydrostatic pressure of blood in a blood vessel pushes water and solutes across the blood vessel wall and into the interstitium. This is a normal function of certain blood vessels, as we shall see later! 2. Active Transport: requires energy input (ATP) 1) Primary (direct) active 2) Secondary (indirect) active 3) Vesicular transport Active transport requires the input of energy from ATP. This ATP id required because molecules are being moved up or against their concentration gradients. It is proteins that move these molecules against their concentration gradients. It is important to realize that creating and maintaining disequilibrium across a membrane in the body is very important and useful. Again, this requires the input of energy from ATP. The movement can be of one or more substances across a membrane: 1. Uniport: When a protein moves only one (uni) kind of molecule. 2. Co-transport: When a protein moves more than one molecule at a time. a. Symport: Moves molecules in the same direction. b. Antiport: Moves molecules in the opposite directions. 1) Primary Active Transport (direct) In primary active transport, energy from ATP is directly used to transport molecules against their concentration gradient. For example, the Na+/K+-ATPase is a membrane spanning protein carrier. Please note the –ase ending, so it is also an enzyme that hydrolyzes (breaks bonds with water) ATP to get its energy. It is also referred to as the 'Na+/K+ pump'. This is because it acts much like a pump that is bailing 8 + out a leaky ship. It works non-stop to continuously expel 3 Na ions out of the cell and at the same time import 2 K+ ions into the cell per cycle. Each cycle of the pump requires 1 ATP molecule. Both Na+ and K+ are being moved against their concentration gradients, therefore we know that ATP must be required because this is active transport. The ATP is hydrolyzed to ADP + Pi + Energy! This is an antiport mechanism, as both molecules are being transported in opposite directions. The Na+/K+ pump helps to maintain the resting membrane potential (RMP) across the plasma membrane of all living cells. Draw a diagram of the Na+/K+ pump. 2) Secondary active transport (indirect) In secondary active transport, the ATP is used indirectly to move molecules across membranes. Essentially what this means is the potential energy that is stored in a concentration gradient is used to help move molecules across a membrane. An excellent illustration of how this is done is seen in the Na+/glucose transporter. The relative concentration of Na+ is low on the inside, high on the outside of the cell. When Na+ moves down its concentration gradient (into the cell) this force is harnessed to move glucose against its concentration gradient (also into the cell). While the Na+ goes down its gradient, the glucose can be dragged along with it, up hill, so to speak. The original source of ATP that allows this to occur is the one used in the Na+/K+ pump described above, as it maintains a low Na+ concentration inside the cell. This is a symport mechanism, as both molecules are being transported in the same direction. Draw a diagram of the Na+/glucose transporter. 3) Vesicular Transport Vesicular transport is used to move large macromolecules or large quantities of a molecule across the plasma membrane. Vesicles are like mini lipid bilayer bubbles that bud off from plasma membrane and encapsulate large molecules. This is an active form of transport that directly requires energy in the form of ATP for the maneuvering of the cytoskeleton. There are two main forms of Vesicular transport 1. Endocytosis - bringing material into the cell, inward vesicular transport. 2. Exocytosis - releasing material from the cell, outward vesicular transport. 1. Endocytosis: There are three general kinds of endocytosis. 1) Pinocytosis (cell drinking): relatively unselective whereby ECF is transported into the cell. 2) Phagocytosis is a process by which cells engulf a particle or another cell into a much larger vesicle, e.g., certain types of WBC (called Macrophages) engulf bacteria this way. 3) Receptor-Mediated Endocytosis: This is a very selective process. Receptors on the external surface of the plasma membrane bind specific ligands. This ligand-receptor complex then creates a clathrin-coated pit, a type of invagination of the membrane. The membrane then pinches this off as cytoplasmic vesicle, thereby ingesting the ligand-receptor complexes. The vesicle membrane and the receptors are recycled to the surface membrane to be used again. 2. Exocytosis: This is used by many cells to secrete or release large molecules or large amounts of a molecule. Intracellular vesicles fuse with the plasma membrane, then releases its contents into ECF. This process requires energy and Ca2+ and involves other proteins. An excellent example of how this is commonly used in the body is the release of neurotransmitters from neurons into the synaptic cleft. This process is also used to secrete large lipophobic molecules, such as hormones, protein fibers and mucus across cell membranes. Exocytosis is also used to insert proteins, such as receptors, into membrane. 9 Lysosomes can remove waste in this manner and is often regulated from outside of the cell (e.g., hormone-induced hormone release). Transcytosis and Vesicular Transport Transcytosis means movement across (trans) a cell (cytosis); it can involve endocytosis, then vesicular transport across cell, then exocytosis out of the cell at the other end. So the substance has moved completely across the cell. This provides for movement of large proteins intact, e.g., the absorption of maternal antibodies through breast milk, or the movement of proteins across capillary endothelium. Transport Across Epithelial Linings An excellent summary of the various types of transport discussed so far is the transport of molecules across epithelial linings, called transepithelial movement. Epithelial membranes are polarized with an apical (lumen or top side) and basolateral (ECF side) membranes have different proteins. The Na+-glucose symport on apical membrane and the Na+-K+-ATPase is only on basolateral (bottom side) membrane. Transporting epithelial cells can alter their permeability by inserting or withdrawing membrane proteins. Although glucose is a large polar molecule (and thus has 2 strikes against it for having an easy passage across a membrane), there are two different transport systems to move glucose across epithelial cells: 1. Secondary active transport. The Na+/glucose symport from the lumen of the gut into the cell through the apical membrane. This is made possible by the continuous active transport of Na+, constantly being ejected across the basolateral membrane of the cell via Na+-K+-ATPase. 2. Glucose can also move across a membrane down its concentration gradient by facilitated diffusion, as seen in across basolateral membrane of the cell. As an interesting note, the substance ouabain, a known powerful toxin to cells, specifically inhibits the Na+/K+-ATPase. These Na+/K+ pumps are found only on the basolateral membrane of transporting epithelial cells. Ouabain placed on one side of the epithelium affects only that side, so only when ouabain is applied to the basolateral side will cause glucose transport to decrease slowly, as the Na+ gradient is abolished, because Na+ enters the apical side with glucose but is not pumped out, so over time the Na+ gradient that powers the symporter disappears. BODY FLUID COMPARTMENTS Fluid in the body can be described as being in one of three different compartments: 1) Intracellular; 2) Interstitial; and 3) Plasma. 1. Intracellular fluid (ICF): the fluid inside cells (within the plasma membrane). 2. Interstitial fluid: the fluid directly bathing cells (tissue fluid); lacks plasma proteins. 3. Plasma: the fluid portion of blood, it can also be referred to as vascular volume. Extracellular Fluid (ECF) The term extracellular fluid (ECF) simply means the fluid outside of a cell. So you can see that both interstitial fluid and plasma are considered to be ECF. In a healthy human body, all of these fluids must have an osmolarity within the range of 295 to 310 mOsM. However, they differ dramatically in the relative concentrations of important ions and molecules. 10 Table 1. A comparison of the relative concentrations in the three tissue compartment volumes. Ion/Molecule K+ Na+ ClCa2+ Proteins Plasma Interstitial fluid ↓ ↑ ↑ ↑ ↑↑ ↓ ↑ ↑ ↑ ↓↓ Intracellular ↑ ↓ ↓ ↓* ↑ * In muscle cells, calcium ions (Ca2+) are stored intracellularly in the sarcoplasmic reticulum (SR). Distribution of Water and Solutes in the Body Living cells use energy to maintain a state of chemical and electrical disequilibrium across the cell membrane. Cell membranes and capillary endothelium act as selective barriers establishing a solute disequilibrium. What this means is that there are very different concentrations of certain ions on the outside of the cell compared to the inside, as seen in Table 1 above. These differences are maintained by active transporters which move solutes against their concentration gradients constantly, leading to chemical and electrical disequilibrium (un-evenness). Because things are being moved up or against their gradients, maintaining this disequilibrium requires energy input in the form of ATP. The Distribution Water in the Body Intracellular fluids = 2/3 of body's water Extracellular fluids = 1/3 of body's water Plasma = 8% ECF Interstitial fluid = 25% ECF Osmosis Osmosis is the net movement of water across a semipermeable membrane from a higher water concentration to a lower water concentration. Typically, water moves freely until osmotic equilibrium is reached. Quite simply, osmosis is a special case of diffusion for water. Osmolarity Osmolarity describes the number of particles per liter of a solution, Osmoles per liter = Osmol/L or OsM or milliosmoles (mOsM). Osmolarity takes into account dissociation of molecules in solution and converts molarity to osmolarity. Osmolarity (osmol/L) = molarity x (number of particles in solution). Osmolarity depends solely on the number of particles per liter of solution. In the human body, all fluid compartment volumes have an osmolarity that falls within the narrow range of 295 to 310 mOsMs. We already know that the fluid in these three compartments is different, but in a health body, their osmolarities must be within this range. Tonicity The tonicity of a solution is a measure of its strength, like the strength of a muscle can be referred to as its ‘tone’ or tension. A solution is made up of two components; the solvent (water in physiology); and the solute (whatever is dissolved in the water). By definition, the solvent is more abundant than the solute and the relative concentration of the solute will determine the tonicity of a fluid. The tonicity of a fluid determines how the volume of a cell will change if placed in that solution. Tonicity has no units, it is always comparative. 11 In human physiology, tonicity is matched with osmolarity in such a way that the optimal value range for human cells (295 to 310 mOsM) is termed isotonic. The prefix iso- means “same”. If we have three beakers, each with the following solutions in them, we need to ask ourselves how a normal cell would respond to each environment. The way we can answer this is to decide which direction water would move (into or out of the cell) 1. Isotonic solution: The cell’s intracellular fluid has the same osmolarity as the fluid surrounding it in the beaker, so there is no net movement of H2O into or out of the cell and its volume doesn't change. This is what cells like and how they function best. Solvent – water. Solute – particle in solution. Cell in solution. 2. Hypertonic solution: This solution is too strong (hyper = above), having more solutes in solution than the intracellular fluid of the cell. Water is in higher concentration inside the cell and will move down its concentration gradient (via osmosis) into the beaker, where water is less. The cell’s volume decreases or shrinks, this is called crenation. When cells crenate, they loose function, which is not good for the body. 3. Hypotonic solution: This solution is too weak (hypo = below), having fewer solutes in solution than the intracellular fluid of the cell. Water is in higher concentration inside the beaker and will move down its concentration gradient (via osmosis) into the cell, where water is less. The cell’s volume increases and may even burst (cell lysis). When cells expand, they loose function, which is not good for the body. In a more complex analysis, tonicity depends on the nature of the solutes, not on osmolarity. Penetrating solutes can enter a cell (e.g., glucose and urea) and non-penetrating solutes cannot enter a cell (e.g., sucrose, NaCl). NaCl is considered to be functionally non-penetrating, as it gets pumped out of the cell as soon as it enters. We will discuss the issues of tonicity and osmolarity more fully in lab. The Body is in a State of Electrical and Chemical Disequilibrium This is the result of the chemical disequilibrium. The major intracellular ions are K+, phosphate (and to some degree proteins). The extracellular ions are Na+, Cl-. The differences between the two sides of the plasma membrane create the electrical disequilibrium and the Resting Membrane Potential (RMP). Electricity and Electrical Signals Atoms are electrically neutral. Ions are created as electrons are added/removed and for each cation in the body, there is a matching anion somewhere. There are important principles to remember for electricity in physiological systems. The Law of Conservation of Electric Charges means that the net amount of electric charge produced in any process is zero. Opposite charges attract, like charges repel and energy is required to separate opposite charges or bring together like charges. Conductors of electrical charge allow free 12 movement of positive and negative charges whereas insulators prevent movement of charged particles as it turns out, cell membranes are insulators. The Plasma Membrane is an Insulator Separation of electrical charges in body occurs across the cell membranes. Ions have electrical and chemical concentration gradients across the plasma membrane. The Na+, Cl- and Ca2+ concentrations are higher in the extracellular fluid and the K+ concentration is higher inside the cell. These electrical and chemical gradients, combined is referred to as the Electrochemical Gradient, are created by active transport mechanisms and selective membrane permeability to certain ions. The inside of cell is negative relative to the outside at rest and a voltmeter is used to measure the membrane potential difference. The next section of physiology, neurophysiology, will further examine this dynamic relationship across the plasma membrane in neurons.