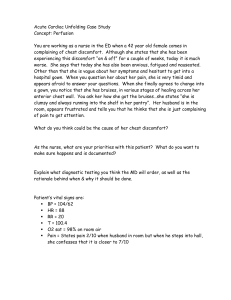
Ramipril

STUDIES ON FORMULATION DEVELOPMENT,
OPTIMIZATION AND IN VITRO RELEASE KINETICS OF
NOVEL BILAYER TABLETS OF RAMIPRIL IMMEDIATE
RELEASE AND METOPROLOL SUCCINATE SUSTAINED
RELEASE
S.Ashutosh Kumar* 1 , S.Manidipa
1 , Dr. Y. Indira Muzib 2 , Dr. J.V.L.N.Seshagiri
Rao 3 , Dr.V. Raghu Murthy 4
1. A.K.R.G College of Pharmacy, Nallajerla, West Godavari, 534112
2. Institute of Pharmaceutical Technology, Sri Padmavati Mahila
Visvavidyalayam, Tirupati, A.P
3. AU College of Pharmaceutical Sciences, Andhra University, Visakhapatnam,
A.P
4. S.V Government Polytechnic, Tirupati, A.P
Author for Correspondance:ashu_mpharm2007@rediffmail.com
INTRODUCTION
Hypertension is one of the most important preventable causes of premature death worldwide and the benefits of antihypertensive drugs have been confirmed by the largest evidence base from clinical trials in medicine. Many classes of drugs are available for treatment, and debate has raged about whether the benefits of treatment are purely a function of the quality of blood pressure control or whether the type of drug used might also be a powerful determinant of outcome.
This is a key question because the difference in cost between "older" drugs
(thiazide or blockers) and "newer" drugs (such as angiotensin converting enzyme
(ACE) inhibitors or calcium channel blockers) is substantial. A meta-analysis of
1
trials of treatment for hypertension with the newer drugs found that ACE inhibitors and calcium channel blockers were likely to reduce cardiovascular morbidity and mortality by the same order of magnitude as blockers or thiazide, but such analyses have insufficient statistical power to detect cause specific outcomes with regard to specific drugs.
There are several forms used interchanged viz controlled release, programmed release, sustained release, prolonged release, timed release, slow release, extended release and other such dosages forms. The goal of any drug delivery system is to provide a therapeutic amount of drug to the proper site in the body to achieve promptly and then maintain the desired drug core. It is for this reason that the science and technology responsible for development of sustained release pharmaceuticals has been, and continues to be, the focus of a great deal of attention in both industrial and academic laboratories.
The history of Sustain Release technology can be divided roughly into 3 time periods. From 1950 to 1970 in the period of sustained drug release a number of systems containing hydrophobic polymers and very wire fabricated with drugs into dosage forms with the aim of sustaining drug levels and hence drug action for an extended period of time. The period of 1990 to 1990 was involved in the determination of the needs in controlled drug delivery and to understand the barriers of various routes of administrations. Post 1999 in the modern era of sustained release dosages forms (Sustained Release drug delivery technology).
Now currently there are numerous products as market formulated for both oral and parentral routes of administration.
2
DEFINITION
Sustain Release systems include any drug delivery system the achieve slow release of drug over an extended period of time. Sustained drug action of a predetermines rate by maintaining a relatively constant, effective drug level in the body with concomitant minimization of undesirable effects.
DRUG PROFILE
METOPROLOL
Metoprolol succinate is a beta 1-selective (cardio selective) adrenoceptor blocking agent its chemical name is (I) - (isopropyl amino) -3-(p-(2methoxy ethyl) phenoxyl)-2-propanol succinate.
Its structural formula is
OH
CH
2
– CHCH
2
NH CH (CH
3
)
2
COOH
CH
2
CH
2
COOH
CH
2
CH
2
OCH
3
DESCRIPTION
Metoprolol succinate is a white crystalline powder with a molecular weight of 652.8.
It’s freely soluble in water, soluble in methanol, sparingly soluble in ethanol,
3
slightly soluble in dichloromethane and 2 propanol, practically insoluble in ethylacetate, acetone, diethyl ether and heptane.
Metoprolol is inactive with ingredients such as silicon dioxide, cellulose compounds, sodium stearyl fumerate, polyethylene glycol, titanium dioxide, paraffin.
CLINICAL PHARMACOLOGY
Metoprolol is a beta1-selective (cardio selective) adrenergic receptor blocking agent. This preferential effect is not absolute, however and at higher plasma concentrations, metoprolol has no intrinsic sympathomimetic activity, and membrane stabilizing activity is detectable only at plasma concentrations much greater than required for beta blockade.
Clinical pharmacology studies have confirmed the Beta-blocking activity of metoprolol in man, as shown by, a. Reduction in heart rate and cardiac out put at rest and upon exercise. b. Reduction of systolic blood pressure upon exercise. c. Inhibition of isoproterenol-induced tachy cardia. d. Reduction of reflex orthostatic tachy cardia.
PHARMACOKINETICS
ABSORPTION :
The absorption of metoprolol of rapid and complete .plasma levels following oral administration of conventional metoprolol tablets however approximate 50 % of levels following intravenous administration, indicating about
50% first pass metabolism.
4
Metoprolol doses the blood brain barrier and has been reported in the CSF in a concentration 78% of the simultaneous plasma concentration.
Plasma levels achieved are highly variable after oral administration. Only a small fraction of the drug (about12%) is bound to human serum albumin.
Metoprolol is a racemic mixture of R- and S- enantiomers, and is primarily metabolised by CYP2D6. When administration orally, it exhibits stereo selective metabolism that is dependent on oxidation phenotype.
The systemic availability and half life of metoprolol if patients with renal failure do not differ, to a clinically significant degree from those in normal subjects.
Consequently, no reduction in dosage is usually needed in patients with chronic renal failure.
METABOLISM
Metoprolol is metabolised predominantly by CYP2D6, an enzyme that is absent in about 8% of Caucasians (poor metabolizes) and about 2% of other populations.
ELIMINATION
Elimination is mainly by biotransformation in the liver, and the plasma half life ranges from approximately 3 to 7 hours. Less than 5% of an oral dose of metoprolol is recovered unchanged in the urine; the rest is excreted by the kidney as metabolites that appear to have no beta blocking activity. Intravenous administration of metoprolol, the urinary recovery of unchanged drug is approximately 10%.
INDICATION AND USAGE
Hypertension:-
5
Metoprolol is indicated for the treatment of hypertension. It may be used alone (or) in combination with other antihypertensive agents.
Angina pectoris
Heat failure:-
Metoprolol is indicated for the treatment of symptomatic (NYHA class II nd or III nd
) heat failure of ischemic, hypertensive (or) cardiomyopathic organ. It was studied in a patients already receiving ACE Inhibitors, Diuretics, and found that metoprolol in combination with above category drugs decreases the rate of mortality plus hospitalization.
CONTRA INDICATION
Metoprolol is contraindicated in severe Brady cardia, heat block greater than first degree, cardiac failure, sick sinus syndrome and in patients who ace hypersensitivity to any component of this product.
WARNING: - ISCHEMIC HEAT DISEASE
Metoprolol particularly in patients with ischemic heat disease, the dosage should be gradually reduced over a period of 1-2 weeks and the patients should be monitored carefully. If angina marked by worsens (or) acute coronary insufficiency develops, metoprolol administration should be reinstalled promptly, at least temporarily, and other measures for the management of unstable angina should be taken.
BRONCHOSPASTIC DISEASES
Patients with bronchospastic diseases should, in general not Receive Beta-
Blockers, because of its relative beta- relativity.
DIABETES AND HYPOGLYCEMIA
6
Metoprolol should be used with caution in diabetic patients if a beta - blocking agents is required. Beta blockers may mask tachycardia occurring with hypoglycemia, but other manifestation such as dizziness and sweating may not be significantly affected.
MAGOR SURGERY
The necessity of with drawing Beta blocking therapy prior to major surgery in controversial; the impaired ability of the heat to respond to reflex adrenergic and surgical procedures.
THYROTOXICOSIS
Beta-adrenergic blockade may mask certain clinical signs
(tachycardia) of hyperthyroidism, patients respected of developing thyrotoxicosis should be managed carefully to avoid abrupt with drawl of beta blockade, which must precipitate a thyroid storm.
Peripheral vascular disease
Calcium channel blockers.
PRECAUTION
Metoprolol should be used with caution in patients with impaired hepatic function. In patients with pheochromocycroma, an alpha blocking agents should be indicated to the case of any beta- blocking agent.
DRUG INTERACTION:
Catecholamine depleting drugs (eg. reserpine, mono amino oxidase
(MAO) may have an addictive effect when given with B-Blocking agents. Patients treated with Metoprolol surplus a catecholamine depletor should therefore be closing observed for evidence of hypotension or marked Brady cardia, which may
7
produce vertigo, syncope, or postural hypotension.
Drugs that inhibit CYP2D6 such as quinidine, fluoxetine, parotexetine and propafenone are likely to increase metoprolol concentration.
Beta- blockers may exacerbate the rebound hypertension which can follow the withdrawal of clonidine.
Caution should be taken while administration of metoprolol to pregnant women as well as nursing women’s.
ADVERSE REACTIONS
CENTRAL NERVOUS SYSTEM : - Tiredness and dizziness have occurred in about 10 of 100 patients. Depression in about 5 of 100, mental confusion, short term memory loss, headache, somnolence, night mares, and insomnia, have also been reported.
CARDIO VASCULAR
Shortness of breath and Brady cardia, cold extremities, arterial insufficiency, usually of the Reynaud type: palpitations, congestive heart failure, peripheral edema, chest pain, and hypotension have also been reported.
RESPIRATORY
Wheezing and dyspnea
GASTRO INTESTINAL
Diarrhea- 5 of 100 patients
Nausea
Dry mouth
Gastric pain
Constipation
8
Flatulence
Heart burn etc.
HYPERTENSIVE REACTIONS
Purities (or) rash in about 5 of 100 patients.
Psoriasis
DOSAGE AND ADMINISTRATION:-
Metoprolol SR tablet intended for once daily administration.
The usual initial dose is 25 to 100 mg daily in case of hypertension.
Dosages above 400 mg per day have not been studied.
In case of angina pectoris the dose of metoprolol SR tablet is 100 mg daily, given in a single dose. The dosage may be gradually increased at weakly until optimum clinical response has been obtained.
25 mg bid, (or) 50 mg bid in case of immediate release tablet.
RAMIPRIL
DESCRIPTION
:
Ramipril is a 2-aza-bicyclo [3.3.01-octanc-3-carboxylic acid derivative. It is a white, crystalline substance soluble in polar organic solvents and buffered aqueous solutions. Ramipril melts between 105°C and 112°C.Ramipril chemical name is (2S, 3aS, 6aS)-l [(S)-N-[(S)-l-Carboxy-3-phenylpropyl] alanyl] octahydrocyclopenta [b]pyrrole-2-carboxylic acid, 1-ethyl ester; its structural formula is:
O
C
H
5
C
2
O
CH
C
2
CH
2
H H
3
C
NH
H
C
H
C
N
O
COOH
9 H
H
Ramiprilat, the diacid metabolite of ramiprilate, is a non-sulfahydryl angiotensin converting enzyme inhibitor. Ramipril is converted to ramipril at by hepatic cleavage of the ester group.
C
LINICAL
P
HARMACOLOGY
:
Mechanism of Action
Ramipril and Ramiprilat inhibit angiotensin-converting enzyme (ACE) human subjects and animals. ACE is a peptidyl dipeptidase that catalyzes the conversion of angiotensin I to the vascoconstrictor substance, angiotensin II. Angiotensin II also stimulates aldosterone secretion by the adrenal cortex. Inhibition of ACE results in decreased plasma angiotensin II, which leads to decreased vasopressor activity and to decrease aldosterone secretion.
The mechanism through which Ramipril lowers blood pressure is believed to be primarily suppression of the rennin-angiotensin-aldosterone system;
Ramipril has an antihypertensive effect even in patients with low-rennin hypertension. Although Ramipril was antihypertensive in all races studied, black hypertensive patients (usually a low-rennin hypertensive population) had a smaller average response to monotherapy than non-black patients.
Pharmacokinetics and Metabolism
The oral administration of Ramipril, peak plasma concentrations of
10
Ramipril are reached within one hour. The extent of absorption is at least 50-
60% and is not significantly influenced by the presence of food in the GI tract, although the rate of absorption is reduced.
Cleavage of the ester group (primarily in the liver) converts ramipril to its active diacid metabolite, Ramiprilat. Peak plasma concentrations of Ramiprilat are reached 2-4 hours after drug intake
Distribution
The serum protein binding of ramipril is about 73% and that of
Ramiprilat about 56%; in vitro, these percentages are independent of concentration over the range of 0.01 to 1
g/ml.
METABOLISM:
Ramipril is almost completely metabolized to Ramiprilat, which has about 6 times the ACE inhibitory activity of ramipril, and to the 3iketopiperazine ester, the diketopiperazine acid, and the glucuronides of ramipril and Ramiprilat, all of which are inactive.
Elimination
After oral administration of ramipril, about 60% of the parent drug and its metabolites is eliminated in the urine, and about 40% is found in the feces. Drug recovered in the feces may represent both biliary excretions of metabolites and/or unabsorbed drug; however the proportion of a dose eliminated by the bile has not been determined. Less than 2% of the administered dose is recovered in urine as unchanged Ramipril.
11
Bioavailability
Blood concentrations of ramipril and Ramiprilat increase with increased dose, but are not strictly dose-proportional. The 24-hour AUC for Ramiprilat, however, is dose-proportional over the 2.5-20 mg dose range. The absolute bioavailability of ramipril and Ramiprilat were 28% and 44%, respectively, when
5 mg of oral ramipril was compared with the same dose of ramipril given intravenously. Plasma concentrations of Ramiprilat decline in a triphasic manner
(initial rapid decline, apparent elimination phase, terminal elimination phase. The initial rapid decline, which represents distribution of the drug into a. large peripheral compartment and subsequent binding to both plasma and tissue ACE, has a half -life of 2-4 hours. Because of its potent binding to ACE and slow dissociation from the enzyme, Ramiprilat shows two elimination phases. The apparent elimination phase corresponds to the clearance of free Ramiprilat and has a half-life of 9.7-18 hours. The terminal elimination phase has a prolonged halflife (>50 hours) and probably represents the binding/dissociation kinetics of the
Ramiprilat/ACE complex. It does not contribute to the accumulation of the drug.
After multiple daily doses of ramipril 5-10 mg, the half-life of Ramiprilat concentrations within the therapeutic range was 13-17 hours.
After once-daily dosing, steady-state plasma concentrations of Ramiprilat are some what higher than those seen after the first dose.
The urinary excretion of ramipril, Ramiprilat, and their metabolites is reduced in patients with impaired renal function. Compared to normal subjects, patients with creaitinine clearance less than 40 ml/min/1,73m
2
had higher peak and trough Ramiprilat levels and slightly longer times to peak concentrations.
12
In patients with impaired liver function, the metabolism of ramipril to
Ramiprilat appears to be slowed, possibly because of diminished activity of hepatic esterase’s, and plasma ramipril levels in these patients are increased about
3-fold. Peak concentrations of Ramiprilat in these patients, however, are not different from those seen in subjects with normal hepatic function, and the effect of a given dose on plasma ACE activity does not vary with hepatic function.
Pharmacodynamics
Single doses of ramipril of 2.5-20 mg produce approximately 60-80% inhibition of ACE activity 4 hours after dosing with approximately 40-60% inhibition after 24 Hours. Multiple oral doses of ramipril of 2.0 mg or more cause' plasrna ACE activity To fall by more than 90% 4 hours after dosing, with over
80% inhibition of ACE activity remaining 24 hours after dosing.
INDICATIONS AND USAGE
Reduction in Risk of Myocardial Infarction, Stroke, and Death from
Cardiovascular Causes
Ramipril is indicated in patients 55 years or older at high risk of developing a major cardiovascular event because of a history of coronary artery disease, stroke, peripheral vascular disease, or diabetes that is accompanied by at least one other cardiovascular risk factor
(hypertension, elevated total cholesterol levels, low HDL levels, cigarette smoking, or documented microalbuminuria), to reduce the risk of myocardial infarction, stroke, or death from cardiovascular causes. Ramipril can be used in addition to other needed treatment (such as
- blockers (such as
13
antihypertensive, antiplatelet or lipid-lowering therapy).
Heart Failure Post Myocardial Infarction
Ramipril is indicated in stable patients who have demonstrated clinical signs of congestive heart failure within the first few days after sustaining acute myocardial infarction. Administration of ramipril to such patients has been shown to decrease the risk of death (principally cardiovascular death) and to decrease the risks of failure-related hospitalization and progression to severe/resistant heart failure.
CONTRAINDICATIONS
Ramipril is contraindicated in patients who are hypersensitive to this product or any other angiotensin converting enzyme inhibitor (e.g., a patient who has experienced angioedema during therapy with any other ACE inhibitor
WARNINGS
Anaphylactoid and Possibly Related Reactions
Presumably because angiotensin-converting enzyme inhibitors affect the metabolism of eicosanoids and polypeptides, including endogenous bradykinin, patients receiving ACE inhibitors may be subject to a variety of adverse reactions, some of them serious.
Head and Neck Angioedema
Patients with a history of angioedema unrelated to ACE inhibitor therapy may be at increased risk of angioedema while receiving an ACE
Inhibitor. Angioedema of the face, extremities, lips, tongue, glottis, and larynx has
14
been reported in patients treated with angiotensin converting enzyme inhibitors.
Angioedema associated with laryngeal edema can be fatal. If laryngeal strider or angioedema of the face, tongue, or glottis occurs, treatment with Ramipril should be discontinued and appropriate therapy instituted immediately. Where there is involvement of the tongue, glottis, Iarynx, likely to cause airway obstruction appropriate therapy, eg, subcutaneous epinephrine solution 1:1,000 (03 ml to 0.5 ml) should be promptly administered.
Intestinal Angioedema
Intestinal angioedema has been reported in patients treated with ACE inhibitors. These patients presented with abdominal pain (with or without nausea or vomiting); in some cases there was no prior history of facial angioedema and
C-l esterase levels were normal. The angioedema was diagnosed by procedures including abdominal CT scan or ultrasound, or at surgery, and symptoms resolved after stopping the ACE inhibitor.
Hypotension
Ramilpril can cause symptomatic hypotension, after either the initial dose or a later dose when the dosage has been increased. Like other ACE inhibitors, ramipril has been only rarely associated with hypotension in uncomplicated hypertensive patients. Symptomatic hypotension is most likely to occur in patients who have been volume- and/or salt-depleted as a result of prolonged diuretic therapy, dietary salt restriction, dialysis, diarrhea, or vomiting. Volume and/or salt depletion should be .corrected before initiating therapy with Ramipril.
15
Hepatic Failure
Rarely, ACE inhibitors, including Ramipril, have been associated with a syndrome that starts with cholestatic jaundice and progresses to fulminant hepatic necrosis and (sometimes) death.
Neutropenia/Agranulocytosis
ACE inhibitors, rarely, a mild - in isolated cases severe - reduction in the red blood cell count and hemoglobin content, white blood cell or platelet count may develop. In isolated cases, Agranulocytosis, pancytopenia, and bone marrow depression may occur.
Fetal/Neonatal Morbidity and Mortality
ACE inhibitors can cause fetal and neonatal morbidity and death when administered to pregnant women. Several dozen cases have been reported in the world literature. When pregnancy is detected, ACE inhibitors should be discontinued as soon as possible.
The use of ACE inhibitors during the second and third trimesters of pregnancy has been associated with fetal and neonatal injury, including hypotension, neonatal skull hypoplasia, anuria, reversible or irreversible renal failure, and death.
Impaired Renal Function:
As a consequence of inhibiting the rennin-angiotensin-aldosterone system, changes in renal function may be anticipated in susceptible individuals. In patients with
16
severe congestive heart failure whose renal function may depend on the activity of the rennin-angiotensin-aldosterone system, treatment with angiotensin converting enzyme inhibitors, including Ramipril may be associated with oliguria and/or progressive azotemia and (rarely) with acute renal failure and/or death.
DRUG INTERACTIONS
With nonsteroidal anti-inflammatory agents: Rarely, concomitant treatments with ACE inhibitors and nonsteroidal anti- inflammatory agents have been associated with worsening of renal failure and an increase in serum potassium.
With diuretics
Patients on diuretics, especially those in whom diuretic therapy was recently instituted, may occasionally experience an excessive reduction of blood pressure after initiation of therapy with Ramipril.
With Potassium supplements and potassium - sparing diuretics
Ramipril can attenuate potassium loss caused by thiazide diuretics.
Potassium - sparing diuretics (Spironolactone Amiloride, triameterene, and other) or potassium supplements can increase the risk of hyperkalemia. Therefore, if concomitant use of such agents is indicated, they should be given with caution.
Pregnancy
Pregnancy Catefories C (first trimester) and D (second and third
17
trimesters). Fetal Neonatal morbidity and Mortality.
Nursing Mothers
Ingestion of single 10 mg oral does Ramipril resulted in undetectable amounts of Ramipril and its metabolites in breast milk. However, because multiple does may produce low milk concentration that is not predictable from single doses, women receiving Ramipril should not breast feed.
ADVERSE REACTION
Cardiovascular:
Symptomatic hypotension reported in 0.5% of patients in US trials) syncope and palpitations.
Hematologic:
Pancytopenia, hemolytic anemia and thrombocytopenia.
Renal:
Some hypertensive patients with no apparent pre-existing renal disease have developed minor, usually transient, increases in blood urea nitrogen and serum creaitinine when taking Ramipril, particularly when Ramipril was given concomitantly with a diuretic.
Acute renal failure.
Angioneurotic Edema:
Angioneurotic edema has been reported in 0.3% of patients in US clinical trials )
Gastrointestinal:
Hepatic failure, hepatitis, jaundice, pancreatitis, abdominal pain
18
(sometimes with enzyme changes suggesting pancreatitis), anorexia, constipation, diarrhea, dry mouth, dyspepsia, dysphasia, gastroenteritis, increased salivation and taste disturbance.
Dermatologic:
Apparent hypersensitivity reactions (manifested by urticaria, pruritus, or rash, with or without fever), photosensitivity, purpura, onycholysis, pemphigus, pemphigoid, erythema multiforme, toxic epidermal necrolysis, and Stevens- Johnson syndrome.
Neurologic and Psychiatric:
Anxiety, amnesia, convulsions, depression, hearing loss, insomnia, nervousness, neuralgia, neuropathy, paresthesia, somnolence, tinnitus, tremor, vertigo, and vision disturbances.
Miscellaneous:
As with other ACE inhibitors, a symptom complex has been reported which may include a positive ANA, an elevated erythrocyte sedimentation rate, arthralgia/arthritis, myalgia, fever, vasculitis, eosinophilia, photosensitivity, rash and other dermatologic manifestations.
DOSAGE AND ADMINISTRATION
Reduction in Risk of Myocardial Infarction, Stroke, and Death from
Cardiovascular Causes
Ramipril should be given at an initial dose of 2.5 mg, once a day for
1 week, 5 mg, once a day for the next 3 weeks, and then increased as tolerated, to a maintenance dose of 10 mg, once a day. If the patient is hypertensive or recently post myocardial infarction, it can also be given as a divided dose.
19
Heart Failure Post Myocardial Infarction
For the treatment of post-infarction patients who have shown signs of congestive failure, the recommended starting dose of Ramipril is 2.5 mg twice daily (5 mg per day). A patient who becomes hypertensive at this dose may be switched to 1.25 mg twice daily, and after one week at the starting dose, patients should then be titrated (if tolerated) toward a target dose of 5 mg twice daily, with dosage increases being about 3 weeks apart.
MATERIALS USED FOR THE FORMULATION OF METOPROLOL
WITH RAMIPRIL DUAL LAYER TABLETS
1. HPMC K-100 (DOW)
2. HPMC K4M (DOW)
3. Micro crystalline cellulose PH 101
4. Ponceau 4 R
5. IPA
6. Povidone k 30
7. Magnesium stearate
8. Talc
9. Sodium stearyl fumerate
10. Starch -1500
11. Eudragit L100
12. Micro cristalline cellulose ph102.
PLAN OF STUDY
20
8.
1.
2.
6.
Formulation of Ramipril immediate release and Metoprolol succinate sustained release dual release tablet dosage form F1.
Formulation and Ramipril IR and Metoprolol succinate SR dual release tablet dosage form F2.
3. Formulation of Ramipril IR and Metoprolol succinate SR dual release tablet dosage form F3.
Formulation of Ramipril IR and Metoprolol succinate SR dual release 4. tablet dosage form F4.
5. Formulation of Ramipril IR and Metoprolol succinate SR dual release tablet dosage form F5.
Formulation of Ramipril IR and Metoprolol succinate SR dual release tablet dosage form F6.
7. Physical characteristics of fabricated tablet F1 to F6 like Hardness, diameter, thickness, friability, weight variations, disintegration time, assay
(content uniformity).
In vitro dissolution tests for fabricates tablet F1 to F6.
21
11.
12
7.
8.
9.
Formulation of Metoprolol
BATCH SIZE: 1000 Tablets
AVERAGE WT. OF METAPROLOL PART: 280 mg
PUNCH SIZE: 14/32
S.No. Ingredients F
1
F
2
F
3
1.
F
4
F
5
F
6
47.5g 47.5g 47.5g 47.5g 47.5g 47.5g
2.
METOPROLOL
SUCCINATE
HPMC K-100 98 g 112 g 126g 140 g 77 g 79.5 g
3.
4.
HPMC K
4
M
MCC pH 101
28 g
92.5g
28 g
75.7g
28 g 28 g 15 g
48.9 g 43.5 g 26.1g
15 g
20.3 g
5.
6.
10.
Povidone K 30
Isopropyl Alcohol
5.6 g 79 g 8.4 g 9.8 g 9.8 g 9.8 g
150 ml
150 ml
150ml 150ml 150ml 150ml
HPMC K -100
HPML K
4
M
LUBRICATION
- - -
- - -
2.8 g 4.2 g 5.6 g -
-
-
77g
15 g
79.5g
15 g
Magnesium
Stearate
- -
Sodium
Fumarate
Talc
Stearyl 5.6 g 7g 7g
2.8 g 2.8 g 2.8 g 2.8 g 2.8 g 2.8 g
COLOURING AGENT
Ponceau 4 R 2.8 g 2.8 g 2.8 g 2.8 g 2.8 g 2.8 g
22
FORMULATION OF RAMIPRIL IMMEDIATE RELEASE PART
Formulation of Ramipril
BATCH SIZE: 1000 Tablets
AVERAGE WT. OF RAMIPRIL PART: 130 mg
PUNCH SIZE: 14/32
S. No.
1.
Ingredients
RAMIPRIPL
F
1
5 g
F
2
5 g
F
3
5 g
2.
3.
4.
5.
STARCH -1500
Eudragit L - 100 , 55
SSF
MCC PH 102
98.7 g
25 g
1.3 g
-
83.7 g
20 g
1.3 g
20 g
78.7 g
15 g
1.3 g
30 g
F
3 formulation is continued for the other 3 formulations
PERCENTAGE OF POLYMER USED METOPROLOL SUCCINATE
PART
Formulation HPMC K
4
KPMC K 100
F
F
1
2
10%
10%
35%
40%
Total polymer con. in %
45%
50%
F
3
F
4
10%
10%
45%
50%
55%
60%
F
5
F
6
10%
10.7%
55%
56.7
65%
67.4
23
MATERIALS AND METHODS
Materials used
The following materials were obtained from commercial sources and used as received.
S. No. Materials Sources
1. Metoprolol succinate
2. Ramipril
Wockard
Wockard
3. Microcrystalline cellulose plain Ranq Remedies, Mumbai
5. Microcrystalline cellulose pH 102 Maize Product, Mumbai
7. Croscarmellose sodium
8. PVP-K-30
9. Isopropyl alcohol
Fisher Ltd., Chennai
Fisher Ltd., Chennai
Fisher Ltd., Chennai
10. Talc
12. Magnesium Stearate
13 HPMC K
100
14.
15.
HPMC K
Ponce 4R
4
18. Acetonitrile
Equipments Used
Kanpha Labs, Chennai
Jain Enterprises, Chennai
Samsung Fine Chemicals,
Mumbai.
Samsung Fine Chemicals,
Mumbai.
Kanpha Labs, Chennai
Nice Chemical Ltd., Chennai.
S. No.
1.
Equipments / Instruments
28 station double hopper bilayer press
Manufacturer
Cadmach, Ahmadabad
24
2.
3.
4.
5.
Rapid mixture granulator
Fluidized bed dryer
Double cone blender
Hardness tester
Remi, Mumbai
Cadmach, Ahmadabad
Cadmach, Ahmadabad
Monsanto
6.
7.
Friability tester
Disintegration tester
8. Dissolution
9. 205-A SGS weighing balance
10. HPLC / SPD-10AVP
Electrolab, Chennai
Electrolab, Chennai
Electrolab TDT 08L
Precisa, Mumbai
Shimadzu Japan.
11. pH Meter STL
METOPROLOL
Manufacturing Process
FORMULATION METHOD
Step - I- Receiving
Weigh all the ingredients mentioned below accordingly to the formula.
Sr.No.
1.
2.
3.
4.
Ingredients
Metoprolol succinate
HPMC - K00 (DOW)
Mico crystalline cellulose PH 101
HPMC K
4
M (DOW)
Receive
30#
30 #
30 #
30 #
25
Step - 2
Preparation of Binder
S.No.
1
2.
Ingredients Name
Povidone K - 30
Isopropyl alcohol
Procedure for Binder Separation
Dissolve providone K-30 is Isopropyl alcohol by slow addition. A void lump formation during addition of providone K-30 stirs to dissolve from various solutions.
Step: 3
Granulation
A. Drug mixing
Mix the step I ingredients in Rotating mixture granulator (RMG) for 25 minutes.
B. Wet Mixing
Granulate the step 3 A ingredients with step 2 ingredients. Addition of binder should be slow to effect granulation, and then approximate of addition is to be recoded on the facing page. Add extra amount of Binder, if required and record the volume / by eight. Use chopper such that not lumps are formed during granulation.
26
Binder Addition time
(Min)
Total granulation time
(min)
Impelled
Chopper
Impeller
Speed
Time (in mins)
Speed
Time (in mins)
Speed
Time (in mins)
Slow
10
Slow
08
High
10
Amount of Binder added
Chopper
Speed
Time (in mins)
.
Step:-4
Initial Drying
Air dries the wet mass in fluidized bed dryer for 15 minutes.
High
08
Step- 5
Receive the drug granule through the sifter fitted with 20#.
Mill the retained granules through a mill fitted with 2 mm screen.
Step - 6
Final Drying
Dry the semidried granules in Fluidized Bed drugs at temperature of 50°C of the outlet temperature gauge to suitably achieve on LOD of 1%. Record the temperature (periodically).
Check for the loss on drying (LOD at 80°C.
Stop drying when the LOD reaches..... NMT 1.0 ..........%
27
Sieving of Lubricants
Sieve the following lubricants already weighed and kept ready as per the formula.
S.No. Ingredients
HPMC K - 100 ( Dow)
Sieve
30 # 1.
2.
3.
HPMC K - 4 m (Dow
Purified tale
30 #
30 #
4.
5.
Magnesium Stearate
Sodium stearyl Fumarate
30 #
30 #
Step - 8
Blending
Pre- blended the received and milled granular is double concentrate blender, along with sifted excipients of Step 7. Except purified Talc and sodium stearyl formulate). This step applied only to V and VI formulation.
Time taken for pre blending - 15 min
Add the sifted lubricant purified the Talc magnesium stearate and sodium stearyl fumerate into the previously prepared granules and mix uniformity. Add
Ponceau 4 R in the in the final stage and mix well.
Time taken for blending 10 minutes
Compression details
Load the granules in the hopper of the Rotary tablet machine and adjust the machine for allowable load on punch tips.
Adjust the machine for it tablet weight, hardness and thickness, start the compression.
28
1.
Mean while the thickness and weight variation should be mentioned usually.
Machine Used
Machine Name : Cad Mach
Punch Tooling
RPM
No of stations :
:
: 25
28
Finally physical parameters such as
Average weight :
2.
3.
Weight variation
Limits (%)
:
Dimension (mm) :
4.
5.
Thickness (mm) :
Hardness (kg/cm
2
) :
6. Friability (%)
Are checked for compressed tablets.
Perform the assay of the collected tablets.
The % of the drug content should fall with in the limit as mentioned in standard.
CORE TABLET SPECIFICATION (STANDARDS)
S.No. Compression Parameters
1. Weight of one tablet
2
3.
Weight of 20 tablets
Thickness
Units mg g mm
Valve
4`0
4.2
0.2
29
4.
5.
6.
7.
8.
Hardness
Friability
Disintegration time
Dissolution
Assay kg / cm
2
% w/w min
%
%
NLT 3.5
NMT 1
NMT 8
As per standard procedure
As per standard procedure
FORMULATION OF RAMIPRIL PART (DIRECT COMPRESSION)
S.No.
1.
2.
3.
4.
5.
Ingredients
Ramipril
Starch 1500
MCCPH 102
Eudragit L 100
CCS
Sieve
30 #
30 #
30 #
30 #
30 #
Step -1
Sieving
Step - 2
Geometrical Mixing
Divide the excipients into 4 equal parts and mix the sieved first part of the ingredient to the drug for 5 minutes, then add the second part, continue mixing for another 10 minutes, finally add the 4th and mix it for 20 minutes.
30
Compression
Load the granules of metoprolol part in the right hand side hopper of the bilayer press.
Adjust the machine for its weight.
Load the direct compression part in the left hand side of the bilayer press
Adjust the tablet wt, thickness and hardness
Start compression
1. Thickness
EVALUATION OF
UNCOATED DUAL RELEASE TABLETS
Control of physical dimension of the tablets such as size and thickness is essential for consumer acceptance and to maintain tablet-to-tablet uniformity. The dimensional specifications were measured using digital micrometer calipers. The thickness of the tablet is mostly related to the tablet hardness it can be used as initial control parameter.
2. Hardness test
The hardness of the tablet was carried out by using Monsanto hardness tester. The hardness of the tablet kg/cm
2
was measured. The results are given in table.
3. Weight variation test:
Twenty tablets were randomly selected an weighed to determine the average weight and was compared with individual tablet weight. The percentage weight variation was calculated. As per pharmacopoeia specification
31
Average weight of tablets (mg)
130 (or) less
130-324
More than 324
Maximum % difference allowed
± 10%
± 7.5%
± 5%
The results are given in table.
Friability test
Weighed amount of 20 dedusted tablets were subjected to rotating chamber of “Roche type friability”. The chamber that revolves at 25rpm. This is then operated for 100 revolutions. The tablets are then dusted and reweighed.
F
W o
W o
W x 100
Where W o
= Initial weight
W = Final weight
Limit for compressed tablets that lose less than 0.5 to 1.0% of their weight.
The results are given in table
Disintegration test
The disintegration test was carried out as per pharmacopoeia procedure.
One tablet was placed in each of the six tubes of the basket and the disc was added to each tube. The test was carried out by using D.M. water as medium. The temperature was maintained at 37
0 C ± 2 0
C. The apparatus was operated and DT was noted. The results are given in table.
ASSAY OF METOPROLOL AND RAMIPRIL
Chromatographic Condition
Column
Detector Wavelength :
: Kromasil C
223 nm
18
32
Flow Rate
Injection volume
:
:
1 ml/ ml
20
l
Mobile Phase Preparation
2 g of sodium perchlorate in 1000 ml of water. To this add 0.5 ml. of triethyl amine.
Adjust pH to 3.6 with orthophosphoric acid
Replace 200ml with acetonitrile. Filter and degas before use.
Buffer: ACN
80: 20
Standard Preparation
Weigh accurately about 25 mg of Ramipril dissolve and dilute it to 25 ml with mobile phase. Take 5 ml from the above solution into 100ml Volumetric flask add 50 mg of metoprolol succinate working standard dissolve with mobile phase and make up the volume to 100 ml.
Sample Preparation
Crush 5 tablets and weigh accurately the average wt. of one tablet and dissolve it by using 20 ml of methanol, 20 ml of 0.1 N HCl, shake well until the drug gets dissolved. Then add the mobile phase and make up the volume to 100 ml.
Filter the supernatant liquid with 0.45
membrane filter.
Calculate the quantity in mg of metoprolol Hydrochloride and Ramipril in each tablet by formula.
Sample Area
S tan dard area
X
Std .
Wt .
X
100
5
100
X
100
Sample .
Wt .
X
AverageWt .
X % purity
Label Claim
= Ans x Conversion factor
33
=
684 .
81
Ans x
652 .
81
1 .
05
METHOD OF ANALYSIS FOR DISSOLUTION
For Metoprolol Succinate (SR part)
Medium : 500 ml pH 6.8 Phosphate Buffer
Apparatus : Basket
Speed
Sampling Points
Temperature
:
:
:
50 RPM
1, 4, 8, 20 Hour
37° C
0.5 °C
No. of Units
Time
1 Hour :
:
:
IV Hour
VIII Hour
:
:
XX Hour :
Chromatographic Conditions
Column :
Detector wavelength :
Flow rate :
6
Limits %
NMT 25%
20 - 40%
40 - 60%
NLT 80%
Kromasil C8
223 nm
1.0 ml / minute
20
l Injection volume :
Mobile phase
Buffer:
: Buffer: Acetonitrile pH 3.0 Phosphate Buffer : 50 ml of 1 M monobasic sodium phosphate and 8.0 ml. of 1 M phosphoric acid and dilute with water to 1000ml adjust with 1 M phosphoric acid to pH 3.0.
34
Diluents : Mobile phase
Standard Preparation:
Weigh accurately about 50 mg of Metoprolol succinate working standard in a 100ml volumetric flask dissolve in a dissolution medium makeup the volume with same. Dilute 5 ml from the above solution to 10 ml with dissolution medium.
Procedure
Set dissolution parameters and place 1 tablet in to each vessel taking care to exclude air bubbles from the surface of the tablet and immediate start the apparatus. After 60 minutes withdraw the sample medium 10 ml and replace the pH 6.8 buffer solution and filter through 0.45
nylon filter and withdraw the sample medium 4th, 8th and 20th hour.
System Suitability
Inject separately 20
l of standard preparation in to the liquid chromatograph and record the chromatograms. Measure the response of the major peaks.
Procedure
Take 5ml from the sample and dilute to 10 ml and inject 20
l sample preparation (one injection) in to the liquid chromatograph and record the chromatogram. Measure the responses for the major peaks. Calculate the dissolved quantity of Metoprolol succinate in percentage form the peak areas of standard and sample preparation and percentage of potency of working standards used.
Calculation for Metoprolol succinate
35
Sample area
S tan dardArea
X
50
500
X
5
10
X
500
47 .
5 x
10
5
X 100
DISSOLUTION FOR RAMIPRIL (Immediate Release Part)
Medium : 900 ml. of purified water
Apparatus : Paddle
Speed
Sampling points
Temperature
:
:
:
75 RPM
45 minutes
37°
0.5°C
No. of Units
Mobile Phase
Buffer Preparation procedure:
: 6
2 gm of sodiumperchlorate in 1000 ml of water. Add 0.5 mg of triethyamine. PH is adjusted to 6.8 with ortho phosphoric acid.
Buffer
50
:
:
ACN
50
Procedure
Set dissolution parameters and place 1 tablet into each vessel taking care to exclude air bubbles from the surface of the tablet and immediately start the apparatus. After 45 minutes replace 10 ml of sample filter through 0.5
nylon filter.
36
Standard Preparation:
Weigh accurately 50 mg of Ramipril working standard in 100ml volumetric flask dissolve in dissolution medium make up the volume with the same. Dilute 5ml to 50 ml and then 5 to 50 ml with dissolution medium.
System Suitability
Inject separately 20
l of standard preparation into liquid chromatograph and record the chromatograms. Measure the response of the major peaks at 215 nm.
Sample Procedure
Inject 20
l of sample into the liquid chromatograph and record the chromatogram. Measure the responses at 215 nm.
Calculation
S
Samplearea tan dard Area x
Std .
Wt
100
5 x
50
5 x
50 x
900
5 x 100
RESULTS AND DISCUSSION
The present investigation was undertaken to formulate and evaluate the bilayer tablet containing Metoprolol succinate as sustained release and Ramipril as an immediate release layer.
The sustained release part was formulated by using hydrophilic polymer
HPMC K - 100 and HPMC K
4
M. HPMC K
4
M was kept constant in a concentration of 10% for 5 formulations. 0.7% was increased in case of the
6th formulation.
37
The concentration of HPMC K
100
was increased 5% is each formulation(
F
1 -
F
5
). In final formulation 56.7% concentration of HPMC K
100
is used to control the release of Metoprolol.
As Metoprolol is a highly water soluble drug the concentration of polymer used to control the release was more.
The theoretical sustained release profile needed for Metoprolol succinate was worked on its pharmacokinetic parameter suggested by Wagner.
The limit of release profile was worked out for all formulations.
Time Limit
Ist hour
4 th hour
8th hour
NMT 25%
25-40%
40 - 60%
20th hour NLT - 80%
The immediate release part was formulated by using different excipients.
Here Eudragit L
100
is used because to stabilize the Ramipril part..
Ramipril is unstable and can be easily degraded into A, B, C, D impurities.
So in order to make Ramipril stable Eudragit was added.
Initially Eudragit L100 delayed the Disintegration time, so we reduced the concentration and finally reached with a stable formulation without any disintegration problems.
Starch 1500 and MCCPH 102 are used because the Ramipril is formulated by Direct compression method.
38
Drug content uniformity (Assay)
For any dosage form the drug content should be uniform for all batches of the tablets as the proportions of excipients used in the formulation is more than
50% of total tabled weight so the drug content uniformity was determined .
Assay for the Final Formulation F
6
Standard area of Metoprolol
Standard area of Ramipril
: 6164158
: 1524881
Calculation
For Metoprolol
Average Sample area of Metoprolol = 5756852
Sample Area
S tan dard area
X
Std .
dilution .
Sample dilution
X
AverageWt .
X
Label Claim converion factor X % purity
5856852
6164158 x
50 .
1 x
100
100
446 .
9 x
439 .
6
50 x 1 .
05 x 100
= 98.13%
Calculation for Ramipril
Ramipril Part
Sample area = 1487200
Sample Area
S tan dard area
X
26 .
4
X
25
5
100
X
100
446 .
9
X
439 .
6 x 100
5
= 101.3%
39
PHYSICAL PARAMETERS REPORT
For all formulation from F1 to F6 the physical parameters like dimension, thickness, hardness, weight variation, friability and disintegration test was performed and reported in table.
Description of the oval layer tablet
Shape
Thickness
: Circular biconvex
: 4.2 ± 0.2mm
Average weight : 410 mg
EVALUATION OF BILAYER TABLET (WT. VARIATION TEST)
415
418
420
422
430
429
422
422
428
415
F
1
412
420
428
8
9
10
11
12
13
6
7
4
5
S. No.
1.
2.
3
F
2
412
412
413
415
410.3
415.2
428..4
415
421.6
421
418
411
409
F
3
417.2
415.8
410.4
410.6
408.4
412.4
418.3
410.8
421.4
420.3
416
414.8
410.8
403.8
405.4
408.6
413
415.6
412.4
F
4
415
412
420.5
420.5
416.2
418.5
420.2
418
420
412
410.4
418.2
410.8
F
5
412.5
412.3
414
410.3
418.6
415.2
410.7
410.8
418.1
412
416
420
418.1
F
6
413
410.6
412.2
410.3
414.2
415
412.6
40
14
15.
16
421
420
418
421.2
418.6
420
17
18
418
415
408.3
410
19 470 410.6
20 420 413.2
Formula x
x
X 100 x x = Actual wt of a tablet
412.6
420.3
420
430
408
408
410.8
410.5
410.7
421
420.3
412.4
421.9
415.8
412.4
412.8
412.4
410.9
414
412.8
414.2
X = Average Wt.
Limit
5%
Result
The weight variation test is performed in all trials (F1 - F6) and these comply with that of the IP standard.
Friability Test
Limit = 1%
Formula F
1
F
2
F
3
F
4
F
5
F
6
8.3286 8.4342 8.5102 8.4832 8.4130 8.4030 Initial Weight
Final Wt 7.8434 7.9182 8.0123 8.4601 8.3924 8.3835
Calculation
IW
FW
IW
X 100
5.82% 6.11% 5.86% 0.27% 0.24% 0.23%
412.3
410.4
412.8
416.2
414
416
412.8
41
Result
Trial F
4
, F
5 and F
6
passed the test for friability
. Hardness test F
1
F
2
F
3
F
4
Limit NLT 5kg
3
2.6
2.4
2.8
3.2
3.4
3.5
3.2
3.6
5.8
4.7
5.4
F
5
5
4.5
5.8
2.8
3
3.5
3.2
2.8
3.4
5.6
4
5.5
4.8
5.8
4.9
Average
2.77 kg/ cm
2
3.22 kg/ cm
2
3.3 kg/ cm
2
5.1 kg/ cm
2
5.12 kg/ cm
2
Result
Trial F
4
, F
5
and F6 has sufficient hardness. Hence passes the test for
4.52 kg/ cm
2 hardness.
Thickness of the Bilayer tablet.
Thickness test F
1
F
2
3.9
F
3
4.1
F
4
4.3
F
5
4.2
F
6
4.2 4.4
4.4 4.2 4.4 4.4 4.1 4.2
Limit NMT
0.2mm 4.3
4.4
4.3
4
4.2
4.0
4.1
4.2
4.2
4.3
4.3
4.2
4.1 4.4 4..4 4 4.3 4.2
Average (mm)
4.32 4.16 4.22 4.2 4.22 4.22
F
6
6
5.4
5.5
42
Result
All trials are with in the limit. Hence passes the test for thickness.
DISINTEGRATION TEST FOR IMMEDIATE RELEASE RAMIPRIL
PART
Disintegration F
1
F
2
F
3
14.20
15.22
9.20
8.23
4.53
4.9
Tablet taken = 6 16.15
14.10
9.26
9.58
5.21
5.13
15.10 10.30 5.08
Average ( in mints)
14.9 9.31
Note: F
4
, F
5
and F
6 batches are continued with the F
3
trial.
Result
The disintegration time of F
3
is 4.9 mints .
DISSOLUTION DATA FOR METOPROLOL SR PART
Release Profile
Ist Hour
IV th Hour
8th Hour
:
:
:
NMT 25%
25 to 40%
40 - 60 %
20th hour : NLT 80%
4.9
S. No. Standard Area
1.
2.
1546785
1542321
3.
4.
1544543
1545238
43
5.
6.
Average
Calculation for Metoprolol succinate
1545238
1545933
1544176
Sample area
S tan dardArea
X
50
500
X
5
10
X
500
47 .
5 x
10
5
X 100
Sl. No.
1
Dissolution Data for F
1
Formulation
Area (1st Hr) Results in %
617670 42.05
Average %
2.
3.
607863
615452
41.43
41.95
599803
601357
40.8
40.99
41.26
4
5
6 589362 40.17
In F
1 formulation 41.26% of Metoprolol was released at the end of Ist hour. This release does not for within the limit of release profile.
Dissolution Data for F
2
Formulation
Sl. No. Area (1st Hr) Results in % Area(4th hour)
1
2.
503252
498651
34.30
33.9
926505
915322
3.
4
5
526432
499821
513423
35.8
34
349
954582
938412
908033
6 503117
Average Results in %
34.29
34.5
946617
Results in %
63.1
62.3
63.7
63.96
61.89
63.27
63.27
44
In F
2 formulation 41.26% of Metoprolol was released was not with the limit. In first hour 34.5% of the drug is released and in second hour the release is
63.27.
So the dissolution was discontinued by 4th hour.
The polymer concentration was further increased to 5%
Sl. No.
1
2.
3.
4
5
Dissolution Data for F
3
Formulation
Area (1st Hr) Results in % Area 4th hour Results in
%
401485 27.3 813921 55.48
398426
391309
361392
411324
27.1
26.9
28.6
28
808993
799361
801630
820367
55.14
55.4
54.6
56.10
6 404312 27.1 796153 54.3
Results in average 26.9 54.9
In F
3
formulation polymer concentration was increased from 40-45%
The release of metoprolol in first hour is 26.9% which is more than the specified limit.
The release of 4th hour is 54.9% which is also over the limit. So further polymer concentration was increased to another 5%.
Sl.
No.
1
2.
3.
4
Area (1st
Hr)
355160
358420
365132
348320
Dissolution Data for F
4
Formulation
Results in
%
Area (4th hour)
Results in %
Area
(8th hour)
24.21
24.4
710320
724636
48.42
49.21
1019156
1123033
Results in %
69.4
76.5
24.8
23.9
754532
744821
51.43 1012315 69
50.77 10123.15 69.2
45
5 357915 24.36 703610 47.9 1048541 69.08
6 368150
Average
25.09
24.4
699845 47.6 1152643 76.3
49.28
In F
4 the release of Metoprolol was within the limit.
In 4th hour the release of Metoprolol exceed s the limit
In 8th hour the release was 72.68% which also exceeds the limit.
So further polymer concentration was increased to 5%.
72.68
Sl.
No.
Area
(1st
Hr)
Dissolution Data for F
5
Formulation
Results in %
Area
(4th hour)
Results in %
Area
(8th hour)
Results in %
Area
(20th hour)
Results in %
1 262509 17.8 571345 38.9 802971 54.7 1412532 96.28
2. 278210 18.9 582320 39.6 796432 54.2 143670 97.94
3. 270513 18.4 581340 39.6 789164 53.74 1339726 91.34
4 260150 17.7 596520 40.6 801326 55.5 1448218 98.72
5 250320 17 603492 41.13 814301 55.6 1467206 100
6 262516 17.8 613117 41.7 804136 55.3 1491027 101.6
Average 18 40.3 54.6
In F
5
the release of Metoprolol was within the limit.
97.6
Therefore for the reproducibility of F
5
formulation, F
6
formulation was developed with 0.7% change in HPMC K
100
polymer concentration.
46
Sl.
No.
1
2.
3.
4
5
Area
(1st Hr)
231626
228413
229124
232138
225163
Results in
%
15.7
15.5
15.6
15.8
15.3
Area
(4th hour)
520416
508347
513721
520132
499841
Dissolution Data for F
6
Formulation
Results in
%
Area
(8th hour)
Results in
%
35.4
34.7
802971
798993
54.7
54.4
35.01
35.4
34
789361
801630
790367
53.80
54.6
53.9
Area
(16th hour)
1204457
1204118
1198432
1199265
1210503
Results in %
Area
(20th hour)
Results in %
82.10 1431683 97.59
82.08 1390651 94.79
81.69 1418523 96.69
81.75 1380694 94.11
82.5 1422541 96.97
1370392 93.41
95.5
6 227913
Average
15.5
15.6
510346 35.02
34.9
786415 53.60
54.19
120581
In F
6
formulation first hour, 2nd hour, 4th hour, 8th hour and 20th hour released was within limit.
82.3
80.25
So we standardize F
6
formula for sustained release of metoprolol.
47
Dissolution data for Immediate release Ramipril Part (F
3
)
Calculation
S
Samplearea tan dard Area x
Std .
Wt
100
5 x
50
5 x
50 x
900
5 x 100
Standard area = 54416
Sl. No.
1
2
3
4
5
6
Area in ( 45 min)
57844
58496
55077
58935
54956
52628
Average Release in %
93.46%
In F
4
, F
5
and F
6
in same working formula (F
3
) were continued.
48
Problems
Faced
Metoprolol
SR Part
PROBLEMS FACED WHILE FORMULATING METAPROLOL WITH RAMIPRIL BILAYER TABLET
F
1
F
2
F
3
F
4
F
5
Ramipril part
hardness
Sticking problem
Release problem
Insufficient
Insufficient hardness
Disintegration problem
Insufficient hardness
Sticking problem
Release problem
Sticking problem
Release problem
Disintegration problem
Disintegration problem OK
F
6
Sticking problem
Release was nearer profile to the
Hardness OK
No Sticking problem
The Release is also with in the limit
This batch was formulated for the reproducibility of F
5
formulation
Release, hardness and other physical parameters are within the limit
49
SUMMARY & CONCLUSION
In the present investigation, studies were undertaken on the design of oral dual release tablet. In that immediate release of ACE inhibition drug, Ramipril and sustained release of Metoprolol succinate as an antihypertensive by using HPMC-
K 100 and HPMC K4 as an Rate controlling polymers.
Metoprolol succinate is used as an antihypertensive. The potential benefits with oral controlled release drug delivery system are reduced side effects, decreased dosing frequency enhanced compliance and convenience.
Introduction regarding bilayer tablet, control release vs sustained. Release formulation, additives, polymers, and pharmacology of Ramipril and metoprolol succinate were discussed.
Literature review regarding the use, and pharmacological, biopharmaceutical, beneficial effect of this combination, information of two drugs and past work done is bilayer tablets was presented in Literature review, section.
Formula regarding the 6 formulations for immediate release .Ramipril, and sustain release Metoprolol succinate was presented in the plan of study.
List of excipients used in two parts of bilayer tablet, reagents, equipments, and instruments procedure for formulation of dual release tablet, drug content assay, Invitro release procedures and evaluation of tablets were given in materials and methods section.
Totally 6 formulations were made by using different ratios of HPMC K
100 and HPMC K
4
M. Here HPMC K
4
is kept constant as 10% for F
1
to F
5
in F
6
10.7%.
50
F
1
sustained release tablets. HPMC K
100 conc. = 35%
F
2
sustained release tablets. HPMC K
100 conc. = 40%
F
3
sustained release tablets. HPMC K
100 conc. = 45%
F
4
sustained release tablets. HPMC K
100 conc. = 50%
F
5 sustained release tablets. HPMC K
100 conc. = 55%
F
6
sustained release tablets. HPMC K
100 conc. = 56.7%
Invitro studies of F
1
- F
6
formulations are carried out and formulation F
5 shows the release with in the limit profile. So finally for the Reproducibility F
6 formulation was formulated. In the SR formulation F
6
, using HPMC K
100
56.7% and HPMC K
4
M 10.7% gives the drug release of 15.6%, 34.9%, 54.19%, 80.25
%, 95.5% at Ist , IVth, VIIIth and XXth hour respectively. As the polymer ratio increases the release rate of the drug decreases from the matrix tablet formulation is various physiological pH conditions.
All the tablet formulations were evaluated for their characteristics such as hardness, thickness, diameter, friability, weight variation and content uniformity
(assay). From the investigation it was noted that the drug content were found to fall within the limits. From this study it can concluded that Ramipril and
Metoprolol can be formulated with Metoprolol as sustained release layer by using
HPMC K -100. The release can be so well controlled that it almost coincides the theoretical release pattern for the drug by proper adjustment of polymer ratio.
Ramipril is formulated as one layer as immediate release. Hence this dual release formulation designed was found to be quite useful in combination therapy.
51
Reference:
1.
Preparation and characterization of Metoprolol sustained release solid dispersion, Department of pharmaceutical science, school of pharmacy and pharmaceutical sciences, 2006 Jul-Aug; 13(4): 295-302.
2.
Validated kinetic spectrophotometric method for the determination of metoprolol in pharmaceutical formulations, Rahman N, Rahman H, Azmi SN,
Department of chemistry, Aligarh Muslim University, Aligarh.
3.
Evaluation of in vitro release rate and in vivo absorption characteristics of four Metoprolol sustained-release tablet formulations, Rekhi Gs, Eddington
ND, Fossler, MJ, Schwartz P, Lesko LJ, Augsburger LL, Dept. of pharmaceutical sciences, School of pharmacy, University of Maryland at
Baltimore.
4.
Notari, Robert E., Biopharmaceutics and Clinical Pharmacokinetics, An introduction, 4 th
Edition, Marcel Dekker, Inc, New York, 1987.
5.
Foye, William O., Lemke, Thomas L., Williams, David A., Principles of
Medicinal Chemistry, 4 th
Edition, Wililams & Wilkins, Baltimore, 1995.
6.
Pharmacokinetics and Biopharmaceuticals A definition of terms, J.
Pharmacokinetic, Biopharm. 1:3 (1973).
7.
A. G. Fishburn, An Introduction of pharmaceutical formulation, pergamon press, New York, 1965.
52
8.
Goodman & Gilman (9 th
Ed)
9.
Katzung 6 th ed.
53