Acute Cardiac Unfolding Case Study - NC-NET

Acute Cardiac Unfolding Case Study
Concept: Perfusion
You are working as a nurse in the ED when a 42 year old female comes in complaining of chest discomfort. Although she states that she has been experiencing this discomfort “on & off” for a couple of weeks, today it is much worse. She says that today she has also been anxious, fatigued and nauseated.
Other than that she is vague about her symptoms and hesitant to get into a hospital gown. When you question her about her pain, she is very timid and appears afraid to answer your questions. When she finally agrees to change into a gown, you notice that she has bruises, in various stages of healing across her anterior chest wall. You ask her how she got the bruises…she states “she is clumsy and always running into the shelf in her pantry”. Her husband is in the room, appears frustrated and tells you that he thinks that she is just complaining of pain to get attention.
What do you think could be the cause of her chest discomfort?
As the nurse, what are your priorities with this patient? What do you want to make sure happens and is documented?
Explain what diagnostic testing you think the MD will order, as well as the rationale behind when & why it should be done.
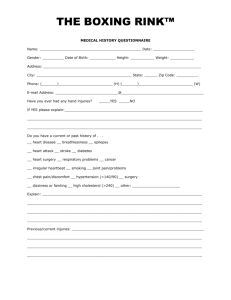
Patient’s vital signs are:
BP = 104/62
HR = 88
RR = 20
T = 100.4
O2 sat = 98% on room air
Pain = States pain 2/10 when husband in room but when he steps into hall, she confesses that it is closer to 7/10
Test results:
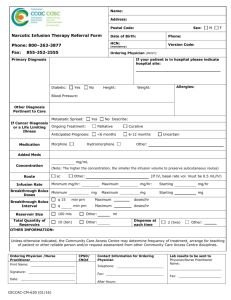
Her EKG shows ST elevation in leads II, III, AVF Hct/HgB = 39.3/13.1
CK = 292
CK/MB = 6%
Troponin I = 4.2
Sodium = 142
Potassium = 3.1
Glucose = 186
BUN/CR = 8/.8
What is significant about this information/these results? Why?
You are working at a small community hospital that does not have a cardiac catheterization lab. Therefore, the physician can only treat this patient medically. If this hospital had a cardiac cath lab, what are some of the interventions that may be done to treat this patient?
The physician has just handed you the chart with orders. The following are the orders he has written:
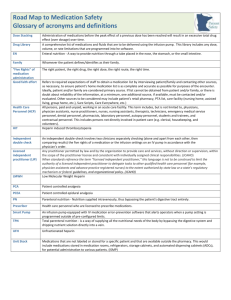
ASA 81 mg po now
Metoprolol 50 mg IV rapid push, times 3 doses (30 minutes apart)
tPA infusion per hospital policy for MI
Heparin infusion at 1200units/hour
D5 ½ NS infusion at 100ml/hour
Oxycodone 1-2 tablets po every 4 hours as needed for chest pain
Nitroglycerin infusion to start at 5mcg/min then titrate for pain but keep
SBP > 100/
What do you think? Are these orders appropriate for this situation/ patient? Is there anything you would change? Anything you that you think was forgotten?
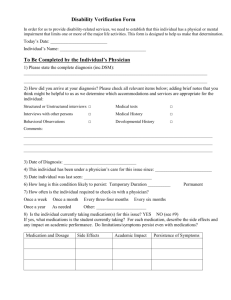
What information (e.g. history, labs, etc.) do you need to know before carrying out any of these orders (or the ones that you determined are more appropriate for this situation)?
You agree that the patient should receive the Heparin infusion. The order states to infuse Heparin at 1200 units/hour via pump. The medication is supplied from pharmacy in a pre-mixed bag…500ml of D5W with 25,000 units of Heparin. What would you need to set the pump at to deliver 1200 units per hour?
While you understand the importance of giving a beta blocker as soon as possible to someone suffering from Acute Coronary Syndrome or Myocardial Infarction, you were right to question the dosage of Metoprolol…50mg IV push is WAY TOO much medication. After clarifying with the physician, he re-orders the medication. The order now reads ‘give 5mg Metoprolol IV push’. The medication is supplied in a vial…upon reading the label you find that there is 10mg of Metoprolol per 5ml. How many ml of the medication will you need to give to deliver the ordered dosage?
You also questioned the order for the IV fluid as her labs did not indicate dehydration and you did not want to increase preload which would increase the workload of the heart muscle. The physician still wants the patient to receive the fluid but agrees to decrease the rate to 50 ml per hour. The IV tubing at your facility has a drop factor of 15.
Please determine how many drops per minute the IV fluid would run at to deliver the fluid at 50
Your patient is currently stable on her NTG and Heparin infusions…so you decide to go on break…
Just when you are getting ready to leave the unit…
The patient’s husband comes out to get you because his wife doesn’t look to good and is writhing in pain. He appears very concerned. How do you respond? What are you thinking/anticipating is the problem? Why?
You were right; the patient was extending her MI and was immediately transferred to the ICU. Due to the severity of her MI, she had complications causing her to spend several days in ICU.
You have just enjoyed a couple days off and come back to work and are assigned to the medical/telemetry unit…Guess what?? You get to take care of your patient from ER that had the MI.
She has been doing fairly well since admission to the medical unit but in report you hear that she has developed heart failure due to her myocardial infarction.
Her ejection fraction has been determined to be 45%.
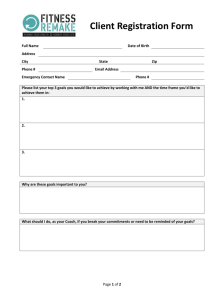
What would you anticipate finding on her assessment?
What medications do you anticipate seeing on her MAR? Why? (Remember to think Contractility, HR, Preload, Afterload
What data would you need to look up in the chart to determine if her treatment is effective?
In reviewing her care plan, what nursing care/interventions do you anticipate finding?
The doctor comes in and tells the patient that she will be going home in the next day or two. She needs discharge education to help ensure that she can prevent exacerbation of her disease process. If you were to develop a teaching plan for her, what would you include on it?