surface basal
advertisement

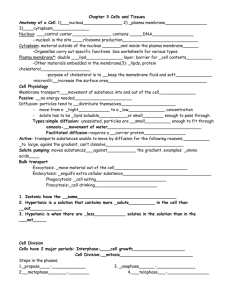
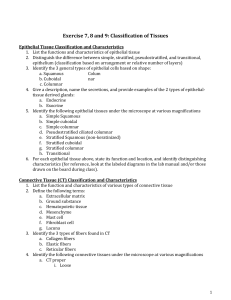
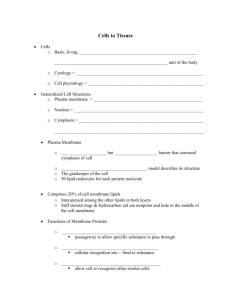
Histology 1 Histology is the study of tissues. The organs of the body consist of four primary tissues: epithelial, connective, muscle, and nervous. Tissues perform specialized functions that enable the organs of the body to carry out specific tasks. A tissue is made up of cells similar to one another in both form and function and the intercellular material in which the cells reside. The intercellular material (ICM) or matrix contains intercellular fluid or ground substance of various consistency and fibers. Tissue = Cells + Intercellular Material (Matrix) consists of ground substance + fibers To understand the tissues' functions the organization, shape and locations of the tissues must be recognized. Procedures A. General Guidelines for Studying Tissues 1. Be familiar with how tissues within an organ are organized. 2. Know the orientation of the tissue slice on the slide. In preparing specimens, three-dimensional organs are sectioned very thin (6 m in thickness) they appear two-dimensional. Cross section (c.s.) and longitudinal section (l.s.) is included on the slide label to explain how the tissue was prepared. 3. Under the microscope, a tissue is made up of cells, fibers and ground substance. Not every feature of a tissue is unmistakable. Elongated cells are often confused with fibers. Nuclei may be interpreted as whole cells, when the cytoplasm or the cell membrane is ill-defined. 4. Examine the slide first under low power, then with high power. Under low power a panoramic view of the specimen is seen. When you have recognized the anatomical relationships among the different tissues in the organ, choose a particular region and examine under high power. 5. You must know the function(s) and at least 1 or 2 locations of each tissue. When you understand tissue structure and location, you appreciate its function. The function of tissues is related to their shape, arrangement and location. 6. Label diagrams, fill out function and location tables (refer to textbook). I. Epithelial Tissue A. General Characteristics, Locations and Functions 1. General characteristics a. Epithelial tissue is always on a free surface, next to a space rather than next to other structures. Apical surface of a cell – exposed to the free surface. Basal surface of a cell – adheres to adjacent underlying surface of connective tissue. Lateral surfaces of a cell – are intercellular membrane junctions that adheres cells to each other. b.The cells of epithelial tissue are closely packed with very little intercellular material between the cells. The cells are held together at cell junctions by tight junctions, anchoring or adhering junctions desmosomes and hemidesmosomes or communicating junctions - gap junctions. 2 Specialized Intercellular Membrane Junctions that occur between Cells 1. Tight Junctions - The lateral cell membranes of adjacent cells towards the free (outer) surfaces fuse, eliminating any extracellular space between the cells. The tight junction prevents passage of substances into the body, except across the apical cell membrane. 2. Adherens Junctions – made of plaque, a dense layer of protein on the inside of the cell membrane. Microfilaments extend from the plaque into the cell’s cytoplasm. Transmembrane glycoproteins anchored in the plaque of one cell crosses the space between the membranes and connects with the transmembrane glycoproteins of the adjacent cell to attach the cells. The adherens junctions extend as a band that encircles the cell, as the adhesion belt. The adherens junctions are observed in epithelial tissue to help epithelial surfaces to resist separation. 3. Desmosomes - maintain a tight cell to cell adhesion between cells so cells do not pull apart from one another. Desmosomes are spot adhesions, which help attach cells to each other. They are composed of plaque and intermediate filaments and linked by tramsmembrane glycoproteins to the adjacent cell. Hemidesmosomes are half a desmosome. They connect cells to the extracellular material, so they anchor one kind of tissue to another kind of tissue in the body. 4. Gap Junction - the cell membranes of adjacent cells are separated by a small extracellular space. Small tubular channels (connexons) extend across the space and link the cytoplasm of adjacent cells. At the gap junctions small molecules and ions can rapidly pass from cell to cell. The gap junctions also play a role in transmission of electrical activity between cells as chemical and electrical signals travel via the gap junctions. The gap junctions are observed in the cells of the nervous system and in cardiac muscle. c. Avascular - no blood vessels. d. Basement Membrane – All epithelial tissue rests on a basement membrane, a nonliving supporting layer that attaches and separates the epithelium from the underlying connective tissue. The basement membrane consists of 2 layers: 1. basal lamina closer to the epithelial cells is mainly made of collagen fibers secreted by the epithelial cells. The basal lamina attaches the epithelial cells to the basement membrane. The basal lamina functions as a filter to selective determine which molecules can diffuse from the underlying connective tissue to enter the epithelium. 2. reticular lamina is closer to the connective tissue is mainly made of reticular fibers secreted by the fibroblasts of the connective tissue. Attachment between the fibers of the two layers of the basement membrane holds the two layers together. Hemidesomosomes attach the epithelial cells to the entire basement membrane. e. Some epithelial cells have the ability to undergo cell division to keep renewing the layer. 2. Locations Epithelial tissue covers surfaces of the body as membranes- outer surface of the body, outer surface of organs, lining of tubes and cavities and also forms the glands of the body. 3. Functions Since epithelium has a variety of locations, epithelial tissue has many functions. The cell shape and number of cells in the layer reflect the functions. a. Protection forms a barrier between the organism and the external environment - stratified epithelium b. Absorption, secretion and excretion - simple cuboidal and simple columnar epithelium c. Diffusion, filtration and osmosis - simple squamous epithelium 3 B. Specialization of Epithelial Cell Surfaces The free surface of many epithelial cells is highly modified for absorption and movement of substances along the surface. 1. Microvilli - function for absorption. Some epithelial cells have on their free surface small cytoplasmic projections, the microvilli, which increases the surface area for absorption. The E/M resolved these structures as cytoplasmic projections containing the microfilaments, actin. In the L/M, the microvilli appear as the striated or brush border on the free surface of the epithelial cells. 2. Cilia - function for moving substances along the surface. Some epithelial cells have on their free surface cilia. The cilia are motile structures containing microtubules. The cilia rhythmically move to propel material along the epithelial surface. 3. Smooth Surfaces - function to reduce friction. Smooth surfaces are found lining the blood vessels and lining the body cavities, these surfaces are non-wettable compared to rough surfaces that are wettable. C. Classification of Epithelial Tissue Epithelial tissues are classified by the number and arrangement of cell layers and shape of the cells at the free surface. 1. Cell Layers a. Simple epithelium - a single layer of cells in contact with the basement membrane. b.Stratified epithelium - 2 or more layers of cells, only the deepest layer is in contact with the basement membrane. c. Pseudostratified epithelium (false) - the tissue appears to consists, of several layers but it is a single cell layer as all cells touch the basement membrane. It appears stratified because some cells are short and do not reach the free surface, while the tall cells which reach the free surface have their nuclei at various depths giving the layer it’s apparent stratified appearance. 2. Cell Shape a. Squamous cell - cell is flat and thin, with a central oval nucleus. b. Cuboidal cell - cell is equal in LxWxD, appears as a square in a section of a tissue with a centrally located spherical nucleus. c. Columnar cell - cell is taller than wide and deep; appears as a rectangle in a section of a tissue with an oval nucleus towards the base of the cell. Epithelial tissue is named according to the number of cell layers and shape of the cell at the free surface. 3. General Classification of Epithelium as a Sheet or Membrane Simple Epithelium a. Simple squamous 1. Structure - a single layer of squamous cells in a thin sheet resting on the basement membrane. 2.Location and 3. Functions - Lines capillaries as a barrier separating blood from tissue fluid. Lines alveoli or air sacs of the lungs, separating air from the tissue fluid. In these locations the simple squamous functions for diffusion and osmosis. Simple squamous also forms the Bowman's capsule of the nephron (kidney tubule), in this location it functions for filtration. Endothelium - simple squamous that lines all blood and lymphatic vessels and the heart. Mesothelium. - simple squamous that lines the thoracic, abdominal and pericardial (ventral) body cavities. 4 The mesothelial cells plus a thin layer of loose connective tissue below is the serous membrane. The mesothelial cells secrete a clear watery fluid, serous fluid to keep the membrane moist. The serous fluid act as a lubricant to prevent friction as the organs move over each other in the body cavities. b.Simple cuboidal 1. Structure - a single layer of cuboidal cells resting on the basement membrane. 2. Location - makes up secretory part and ducts of glands, part of kidney tubule, outer layer of ovary 3. Functions - secretion, absorption c. Simple columnar 1. Structure - a single layer of columnar cells resting on the basement membrane. 2. Location and 3. Functions - nonciliated simple columnar epithelium functions for absorption and secretion. The nonciliated columnar epithelial cells have on their free surface microvilli. Some of the columnar cells are modified to secrete mucus, the goblet cell. The goblet cell can be considered to be a unicellular gland. The secreted mucus lubricates the material in the digestive tract as it passes through. The ciliated columnar epithelial cells have cilia on their free surface. These cells line the upper respiratory tract (bronchi, nasal cavities), oviducts. The cilia move substances along the surface to sweep passageways clear. d. Pseudostratified columnar 1. Structure - All cells contact the basement membrane, but short cells do not reach the free surface. The nuclei of the taller cells are found at different levels in the cells, which gives the appearance of cell stratification. On the free surface of the pseudostratified columnar epithelium are cilia. Scattered among the ciliated columnar are goblet cells. 2. Location - lining of the trachea and primary bronchi. 3. Functions - secretion and sweeping passageways clean of dust and mucus. The mucus traps the dust and debris and the cilia wave-like movement sweeps the mucus and trapped materials up to the mouth for elimination. Mucous membrane lines internal passageways that lead to the outside. The mucus secretions moisten and lubricate the membrane. The epithelial histology changes in different mucous membranes. Stratified Epithelium e. Stratified squamous 1. Structure - composed of 2 or more cell layers, the precise number of cells varies in different locations. The basal cell layer rests on the basement membrane. The basal cells are columnar to cuboidal cells, in the middle cell layers the cells become polygonal (more irregular and flatter). Toward and at the free surface there are flat squamous cells. The basal cells undergo mitosis. These cells are pushed toward the surface to replace older cells sloughed off by abrasion (desquamation). 2. Location - found in those regions of the body subjected to friction and abrasion, such as the epidermis of the skin, linings of the mouth, pharynx, esophagus, anus and vagina. 3. Function - Protection a. Keratinized stratified squamous - On the external surface of the body the stratified squamous becomes keratinized to prevent drying out and to protect against abrasion. Keratin is a tough waterproofing protein that resists friction and bacterial invasion. b. Nonkeratinized stratified squamous - Forms the lining of the upper and/or lower ends of organs systems that open to the outside, such as the digestive, repiratory, urinary and reproductive systems. This epithelium is kept moist by glands that secrete mucus, viscous fluid that moistens and lubricates the free surface. These linings are considered to be mucous membranes. 5 f. Transitional epithelium 1. Structure -The shape of the surface cells and numbers of cell layers varies depending on whether the urinary bladder is empty or full. a. Empty bladder- when bladder is empty, the epithelium is relaxed, the basal cells are cuboidal to columnar and there are several cell layers. The surface cells are large rounded dome-shape cells. b. Full bladder- when bladder is full, the epithelium is stretched, the cells flatted out, the cell layer is 3-4 cells thick, surface cells become large flat and squamous-like cells. 2. Location -This stratified epithelial tissue lines the urinary bladder and ureters. 3. Function - This tissue allows the organs to expand with little resistance. This tissue lessens the chance of organ rupture and reduces discomfort as the organs become full. 4. Glandular Epithelium A gland consists of epithelial cells that produce secretions. a. Unicellular glands Goblet cells - mucus secreting b. Multicellular glands These glands are clusters of epithelial cells derived from the epithelial membrane and reside in the connective tissue. 1. Exocrine glands - connected by duct to the epithelial membrane. They produce specific secretions. 2. Endocrine glands - ductless glands secrete into blood. II. Connective Tissue Connective tissue is the most abundant of the basic tissues. Connective tissue has many different forms and a variety of functions. A. General Characteristics Connective tissue is characterized by an abundance of intercellular substance. The cells are widely scattered. Running through the intercellular substance are blood vessels (vascular tissue) and nerves. The intercellular substance or matrix consists of ground substance and fibers. The cells and fibers are deposited in the ground substance. The living connective tissue cells make and maintain the intercellular substance. The ground substance has various degrees of consistency from fluid to solid. B. Functions Connective tissue forms a framework of the organs in which cells of the organ can be held in place. It serves to attach one type of tissue to another. It serves to hold tissues and organs in place. It forms a rigid support framework of the body. It protects and insulates organs. It serves as a storage site for excess adipose tissue (fat) and blood. It serves as a site for blood cell production and destruction. It serves for transport of material. C. Classification Due to structural diversity, connective tissue is classified into 3 major groups. 1. Loose (areolar, adipose, reticular) ———––– Connective tissue proper (soft) 2. Dense - irregular and regular (parallel)—–––– White fibrous – irregular arranged – dermis 6 regular arranged – tendons and ligments Yellow fibrous – regular arranged – fenestrated (broken) membranes of the elastic arteries, such as in the aorta bundles of elastic fibers – ligamenta nucha in the neck, helps support the neck, ligamenta flava in the vertebral column, attach vertebrae to each other 3. Specialized (cartilage, bone, blood) \ / hard D. Components of Connective Tissue Proper 1. Cells - There are several kinds of cells in connective tissue. The fibroblasts (fibrocyte) and macrophage are most common in the connective tissue proper. a. Fibroblast (fibrocyte) - from a surface view the cell is stellate shape with a central oval nucleus. From a side view the cell is spindle-shape. These cells are up against the fibers. The fibroblasts (fibrocytes) produce and maintain the ground substance and fibers of the connective tissue. Blast cells - retain capacity for cell division and secrete ground substance and fibers. Cyte cells-just maintains the ground substance and fibers. b. Macrophages - irregular shaped cells, that are the phagocytes. They move through the loose connective tissue by ameboid movement and phagocytose foreign matter in the connective tissue proper. When not moving the macrophages are attached to the fibers. c. Other cells - Plasma cells (B-lymphocytes), other WBC, and fat cells, Mast cells. 2. Intercellular Material or Matrix The intercellular material or matrix consists of ground substance and fibers. a. Ground substance - is amorphous and homogeneous. It has consistency that varies from fluid of the blood to loose watery gel of connective tissue proper to semi-solid gel of cartilage to a solid gel of bone. The main organic molecule found in the ground substance is hyaluronic acid. It has a slippery jelly-like consistency. It is composed of protein and polysaccharide. b. Fibers - There are 3 types of fibers. 1. Collagenous (white) fibers are tough, strong, thick, non-elastic fibers. The fibers are made of the protein, collagen. The collagenous fibers have great tensile strength due to the overlapping arrangement of parallel oriented collgen molecules. The collagenous fibers are relatively thick fibers compared to elastic fibers and are branching in some types of connective tissue. The collagenous fibers are white in color and sometimes referred to as white fibers. __________ 2. Elastic (yellow) fibers - thin homogenous fibers, which branch in some types of connective tissue. The fibers are elastic, in that after being stretched or compressed the fibers return to their original shape and length. These fibers are made of the protein, elastin. Elastic fibers are yellow in color and sometimes called yellow fibers. 7 3. Reticular fibers - short, thin, fine branching collagen fibers. The reticular fibers are fine bundles of the collegen protein. They are non-elastic fibers. The reticular fibers are arranged in a tight framework called a reticulum or stroma. The fibers form an internal framework of the organs in which the cells of the organs can be trapped, supported and held in place. The reticular fibers are part of the basement membrane. Reticular fibers are non-elastic and are composed of the protein, collagen. The reticular fibers are similar to collagenous fibers, except the reticular fibers are arranged in a net-like configuration. Types of Connective Tissue The connective tissues are classified according to the nature of the ground substance and types and organization of the fibers in the ground substance. E. Types of Connective Tissue Proper (soft connective tissue) 1. Loose (Areolar) connective tissue Structure - The collagenous and elastic fibers are loosely and irregularly arranged (unorganized) with a great deal of ground substance between the fibers. The cells of the loose connective tissue are of many different types - fibroblasts and macrophages are the most common plus WBC such as lymphocytes and mast cells. The ground substance is a loose watery gel. b. Location - Loose connective tissue is the most widespread connective tissue of the body (superficial fascia). The loose connective tissue attaches the dermis of the skin to skeletal muscle. It also is beneath the epithelial tissue that lines organs. As a denser connective tissue it fills spaces between organs to hold organs and blood vessels in place (deep fascia). It acts as a packing material. c. Function - Loose connective tissue holds cells of tissues in an organ. 2. Adipose or fat tissue Structure - The tissue is composed of groups of fat cells (adipocytes) surrounded by loose connective tissue. Each adipose cell contains a large fat droplet of triglyceride in the center of the cell. A thin ring of cytoplasm at the cell’s periphery surrounds fat droplet. The shape of the cell gives it the name, the signet ring cell. b. Location - Adipose tissue is abundant in the subcutaneous layer of the skin and surrounds organs of the body. c. Functions - Adipose tissue serves as a storage site for fat and acts as an energy reserve. In the subcutaneous layer of the skin it has an insulating function against heat lost. As it surrounds the body organs it protects these organs from injury as it act as a shock absorber. 3. Reticular tissue a. Structure - consists of a network of reticular fibers, reticular cells (fibroblasts) and macrophages in a loose watery gel ground substance. b. Location - This tissue provides structural support for the cells of a tissue in an organ, such as the liver, spleen, lymph nodes and skeletal muscle. c. Function - Forms a framework to trap and hold cells of an organ in place. 4. Dense Connective tissue Fibers are closely packed. a. Dense Irregular Arranged Collagenous Connective tissue 1. Structure - Dense irregular arranged collagenous connective tissue contain the same components as loose areolar connective tissue, but has fewer cells and more collagenous fibers. The fibers are thick, closely interwoven and randomly oriented to form a compact tissue with little ground substance. 8 2. Location - This tissue forms the dermis of the skin and capsules around organs, such as kidneys, organs of the thoracic and abdominal cavities (liver, spleen), perichondrium, periosteum, and surrounding joint cavities. The fascia organization of the connective tissue fibers resembles that of plywood. All fibers in one layer run in the same direction. The fiber in the next layer runs in another direction. 3. Function - Protection and attachment. b. Dense Regular Connective tissue 1. Dense Regular Arranged Collagenous Connective tissue a. Structure - The collagenous fibers are tightly packed in parallel bundles. The fibers run in one direction. The fibroblasts are few and are in parallel rows between the collagenous fiber bundles. There is very little ground substance. The abundance of the collagenous fibers gives this tissue great tensile strength and a white appearance. This tissue can be referred to as white fibrous connective tissue. b. Location - This connective tissue forms the tendons, (cord-like structures) that attach muscles to bones, and ligaments that attach bones to bone. The aponeuroses are broad sheets that act as tendons attaching muscle to some structures. c. Function - attachment of structures to each other. 2. Dense Regular Arranged Elastic Connective tissue a. Structure - This tissue contains elastic fibers regularly arranged. The elastic fibers are fused into a sheet to form a membrane. Since these membranes are broken they are called fenstrated membranes. b. Location - This type of tissue is found in the walls of the large arteries, trachea and vocal cords. c. Function - The elastic fibers and membranes allow this tissue to be stretched and then-return to its original length after the stretch. F. Blood Blood is a connective tissue, since it has cells, plasma, the ground substance and fibers, the components of connective tissue. The fibers, fibrin, form during clotting. G. Hard Connective Tissue 1. Cartilage a. Structure - Ground substance is a semi-solid gel in which collagenous fibers are embedded. The ground substance contains hyaluronic acid and chondroitin sulfate, the latter molecule gives the ground substance gel a firm consistency. The fibers and ground substance are produced and secreted by the chondroblasts. When the chondroblasts become surrounded by the matrix they reside in spaces, the lacunae. The mature cartilage cells are now called chondrocytes. The chondrocytes are spherical cells. The cartilage surface is covered with a fibrous connective tissue covering, the perichondrium. Within the perichondrium there are blood vessels, undifferentiated cells and chondroblasts. It is from the perichondrium. that the cartilage mainly grows. There are no blood vessels or nerves running through the ground substance of the cartilage, thus the cartilage is avascular. b. Growth of cartilage 1. Interstitial growth – Cartilage grows from within due to division of the chondrocytes and deposition of martrix. Interstitial growth occurrs when the cartilage matrix is pliable during childhood. 2. Appositional growth – Cartilage grows from the inner surface of the perichondrium as the chrondroblasts lay down cartilage. The martix accumulates beneath the perichondrium causing growth in cartilage from the outside of the cartilage. There are 3 kinds of cartilage due to the kinds of fiber embedded in the ground substance. 9 a. Hyaline cartilage 1. Structure - The collagenous fibers are dispersed throughout the ground substance, but the fibers are not distinguishable in the ground substance. The hyaline cartilage matrix appears homogenous. Unstained the matrix has a glassy, milky blue-white smooth appearance. 2. Location - This tissue is widely distributed in the body. It is found in the embryonic skeleton, the costal cartilages at the ends of the ribs where the ribs attach to the sternum, nose, parts of the larynx, the "C"-shaped rings of the trachea and rings of the bronchi and the articular cartilage on the ends of bones, where bones meet to form joints. 3. Function - Hyaline cartilage is found where support and flexibility are needed. b. Elastic cartilage 1. Structure - Elastic cartilage contains elastic fibers in the ground substance. 2. Location - This tissue is found in the pinna of the external ear, larynx and epiglottis. 3. Function - Elastic cartilage is found where flexibility is needed. c. Fibrocartilage 1. Structure - Fibrocartilage contains dense irregular arranged collagenous fibers in a little ground substance with scattered isolated groups of hyaline cartilage. 2. Location - Intervertebral disks, pubic symphysis, articular discs in certain joint cavities, such as the knee joints 3. Function - Fibrocartilage has a weight bearing function. 2. Osseous (Bone) Tissue Structure - The matrix of the osseous (bone) tissue is a solid, rigid mineralized gel with collagenous fibers. Within the matrix, the inorganic salt crystals are deposited in the ground substance and among the fibers. These crystals are hydroxyapatite crystals composed of Ca, OH and PO4. The cells that make the osseous tissues are called osteoblasts. The osteoblasts when surrounded by the osseous tissue reside in spaces, the lacunae and are now called osteocytes. The osteocytes are stellate shaped cells having osteocyte processes. Radiating from the lacunae are small canals, called canaliculi, in which the osteocyte processes reside. Osteoclasts are cells in the osseous tissue that dissolves bone. Osteoblasts and osteoclasts working together constantly alter the density and the shape of bone in response to stresses place upon the bone. b. Location – Osseous (bone) tissue forms the adult skeleton. c. Function - This tissue functions for support, movement, protection, mineral reservoir and houses sites of blood cell formation. Triglyceride (fat) storage in the yellow marrow. d. Growth of Bone – Appositional growth - Bone grows by apposition as the osteoblasts in the inner layer of periosteum and from the endosteum lay down bone matrix. Thus bone grows from the outer surface and from the inner surface. There are 2 types of osseous (bone) tissue in the adult skeleton. a. Compact Osseous (Bone) tissue Compact bone is the main type of osseous tissue. The basic unit of compact bone is the Haversian system or osteon. Each Haversian system has central Haversian canal, which contains blood vessels and nerves. Concentric rings or layer or lamellae of bone matrix surround the Haversian canal. Between the lamellae are the lacunae, which contain the osteocytes. The osteocytes’ processes lie in the canaliculi. It is through the canaliculi and the lacunae that the osteocytes are interconnected to each other. This arrangement allows for diffusion of substances between the osteocytes. Covering the outside of the bone is a layer of dense irregular arranged collagenous connective tissue, the 10 periosteum. Sharpey's fibers attach the periosteum to the bone. In the periosteum there are blood vessels and nerves that penetrate into the bone. Undifferentiated cells and osteoblasts allow the bone to grow in thickness from the inner layer of the periosteum. Compact bone forms the outer part of an entire bone. b. Cancelleous (Spongy) Bone tissue The bone is in irregular meshlike arrangement of thin plates, called trabeculae. The cancelleous bone is found toward the inner part of the bone extending into the marrow cavity under the compact bone. Cancellous bone is covered by an endosteum. It consists of undifferentiated cells and osteoblasts, etc., which allows the bone to grow in thickness from the inside and osteoclasts which causes bone resorption. Appositional bone growth from the osteoblasts in the inner layer of the periosteum and from the endosteum. Canelleous bone grows in thickness from the endoseteum surrounding its outer surfaces. III. Muscle Tissue The cells of muscle tissue are elongated, thin cells. Muscle tissue functions by contraction and relaxation for movement, stabilizing body positions, regulating organ volume and generating heat. The characteristics of muscle tissue that allow it to carry out its functions are: 1. irritability - responds to stimuli and conduct impulses; 2. contractility - shortens and thickens to generate a force to do work; 3. extensibility - can be stretched; 4. elasticity - returns to original shape after shortening or lengthening. There are 3 types of muscle tissue. A. Skeletal muscle Skeletal muscle is voluntary muscle, contractions are controlled by conscious will of the individual. Skeletal muscle requires nerve stimulation for contraction. 1. Location - Skeletal muscle is attached to the skeleton. 2. Function - Skeletal muscle causes movement of the bones at the joints and "locks" the joints for maintaining posture. 3. Structure - Skeletal muscle cells are long cylindrical shaped cells, grouped together into masses called muscles. Within the muscles, the cells are grouped into bundles (fascicles) with the cells parallel to each other. Within each skeletal muscle cell there are longitudinal running microfilaments containing the proteins, actin and myosin. These microfilaments, called myofilaments, are grouped into larger units, called myofibrils. The myofibrils have alternating light (I band) and dark (A band) band patterns crossing them due to the parallel and in register arrangement of the actin and myosin. This banding pattern gives the skeletal muscle in longitudinal section its cross-striated appearance. Each skeletal muscle cell is so large that it is multinucleated cell, with oval-shaped nuclei located just under the cell membrane, i.e. peripheral located nuclei. B. Smooth muscle Smooth muscle is involuntary muscle, contractions are not controlled by conscious will of the individual. Smooth muscle does not require nerve stimulation for contraction. 1. Location - Smooth muscle cells are located in the walls of hollow internal organs, such as blood vessels, digestive system, respiratory system and reproductive system. 2. Function - Smooth muscle controls movement of the contents within the lumens of hollow internal organs by controlling the diameter of the lumen of the hollow organ and by regulating the volume 11 of organs. 3. Structure - Smooth muscle cells are spindle-shaped cells which taper to points. The smooth muscle cells are smaller than the skeletal muscle cells. There is a single oval shaped centrally located nucleus in each cell. The smooth muscle cell contain actin and myosin myofilaments but not in an orderly arrangement to give A and I band patterns, thus the muscle is called smooth. The smooth muscle cells in the muscle are arranged in sheets with the cells offset and overlapping each other. C. Cardiac muscle Cardiac muscle is involuntary muscle. 1. Location - Cardiac muscle forms the wall of the heart. 2. Function - Cardiac muscle on contraction develops the force or pressure to pump the blood through the blood vascular system. 3. Structure - Cardiac muscle cells are short branching cylinders, organized into a branching network. The cardiac muscle cells contain cross striated myofibrils similar to skeletal muscle cells, but the striations are not as distinct. Each branch has 1 or 2 oval, centrally located nuclei. Where adjoining cardiac muscle cells meet end to end a thickening of the cell membrane forms, the intercalated disk. In the intercalated disk there are desmosomes for strength to prevent the cells from pulling apart on contraction and relaxation and gap junctions. The intercalated disk is unique to cardiac muscle and can only be seen in longitudinal section of cardiac muscle. Importance of the gap junctions in the intercalated disks. The gap junctions allow for quick conduction of impulses across the cells of the cardiac muscle. The gap junctions allow impulses to reach all cardiac muscle cells at one time so that the entire heart contracts at once. Thus the cell mass is acting as an entire functional unit, which is, called a syncytium. In the heart have a site that initiates the impulse which spreads across the cardiac muscle cells through the gap junctions and triggers a wave of contraction through the entire muscle mass at one time producing a great force of contraction. IV. Nerve Tissue Nerve tissue is specialized for conduction of nerve impulses. Nerve tissue is composed of 2 kinds of cells. A. Nerve cells or neurons The neurons are cells that receive and transmit the nerve impulses. The neuron is the structural and functional unit of the nervous system. . 1. Function - The neurons conduct information in the form of the nerve impulse or action potential from one part of the body to another. 2. Structure - The neuron is a long thin structure. It has three basic parts a. Cell body, Perikaryon, Cyton - the area of the cell that contains the nucleus and other cellular organelles. b. Cytoplasmic Processes 1. Axon - A long thin cytoplasmic process that conducts the nerve impulse away from the cell body. 2. Dendrites - Projecting from the opposite side of the cell body one or usually more shorter processes. The dendrites conduct nerve impulses to the cell body. B. Neuroglial Cells Neuroglial cells are supporting and nutritive cells. They do not conduct impulses. Neuroglial means 12 nerve "glue", as these cells hold the neurons together in the nerve tissue. Neurilemmal cell is an example of a neuroglial cell found in the peripheral nerve. Coverings of the axon A visible fatty insulating sheath, the myelin sheath, covers most axons. The myelin sheath is made by the neurilemmal cells. The myelin sheath is not continuous, but has gaps, the neurofibral nodes (nodes of Ranvier). The neurofibral nodes maintain contact between the neuron and the intercellular fluid, as the myelin sheath is an insulating material. This allows for rapid rapid nerve impulse transmission. Each neurilemmal cell makes a small segment of myelin along the length of the axon.. 3. Location - Neurons and neuroglial cells are found in the nervous system. A nerve is a group of neurons bound together by connective tissue. V. Membranes Membranes are flat sheets of pliable tissue that cover or line a part of the body. The combination of epithelial tissue and underlying connective tissue makes up an epithelial membrane. The epithelial membranes of the body are mucous membranes, serous membranes and cutaneous membrane (skin). A synovial membrane which lines joint cavities contains connective tissue but has no epithelium. A. Epithelial Membranes 1. Mucous Membranes A mucous membrane (mucosa) lines body cavities that open to the outside. The digestive, respiratory, reproductive and urinary tracts are lined by mucous membranes. These membranes contain a lining layer of epithelium and an underlying layer of connective tissue. The epithelial membrane of the layer is the primary body’s defense mechanism against pathogens. As these organisms have difficulty in penetrating the layer. Tight junctions prevents materials from leaking between the cells on their lateral surfaces. Goblet cells and other cells of the membrane secrete mucus. Mucus is a viscous fluid prevents the body cavities from drying out. Mucus traps debris in the respiratory tract and also lubricates food as it passes through the GI tract. The epithelial layer secretes enzymes for digestion and is the site for absorption of digested foods from the GI tract due to microvilli. The epithelium of the mucous membrane varies in different parts of the body. For example, in the small intestine the epithelium is nonciliated simple columnar; in the trachea the epithelium is pseudostratified ciliated columnar. The connective tissue layer of the mucous membrane is composed of areolar connective tissue and is called the lamina propria. The lamina propria supports the epithelium, binds the epithelium to the underlying structures, protects the underlying structures and gives flexibility to the membrane. The lamina propria contains blood vessels for exchange of materials from the lamina propria and the epithelium. 2. Serous Membranes A serous membrane (serosa) lines body cavities that do not open to the outside and covers organs 13 that lies within the body cavities. Serous membranes consist of simple squalors epithelium (mesothelium) below which is areolar connective tissue. The mesothelium secretes a watery (serous) fluid that permits organs to move easily over each other and slide against the internal walls of the body cavities. The serous membranes are composed of two layers: The layer covering the wall of the cavity is the parietal layer; the layer covering and attaches the organs to wall of the cavity is the visceral layer. The name of the serous membrane differs depending upon in which body cavity it is found. The pleura lines the thoracic cavity and covers the lungs. The pericardium lines the pericardial cavity and covers the heart. The peritoneum lines the abdominal cavity and covers the abdominal organs. 3. Cutaneous Membrane The cutaneous membrane (skin) covers the surface of the body. It has on its free surface the keratinized stratified squamous epithelium (epidermis) which protects the underlying dermis of areolar and dense irregular connective tissue. 4. Synovial Membranes Synovial membranes are not epithelial membranes. The synovial membranes line freely movable joint cavities. These cavities do not open to the outside. The synovial membranes is composed of a discontinuous layer of synoviocytes which lines the cavity and deeper layer of areolar and adipose connective tissue. The synoviocytes secrete synovial fluid which lubricates and nourishes the cartilage covering the ends of the bones in the joint cavity. The synovial fluid also contains macrophages to phgoctyose debris from the joint cavity. 14