PosturalOrthostaticTachycardiaSyndrome
advertisement

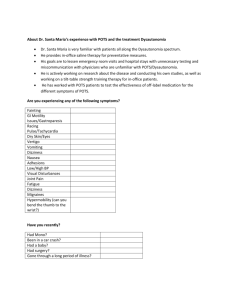
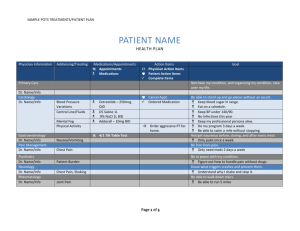
Postural Orthostatic Tachycardia Syndrome (POTS) Postural orthostatic tachycardia syndrome (POTS) is diagnosed with a heart rate increase of 30 beats per minute or more, or over 120 beats per minutes, within ten minutes of standing with or without hypotension. In children and adolescents, diagnosis is made with an increase of 40 beats per minute or more. POTS is often diagnosed with a tilt-table test, but observation by bedside measure of heart rate and blood pressure can be used. Most POTS patients experience a drop in blood pressure when they stand, but some have either no change or an increase in blood pressure. Various tests of the autonomic nervous system may be used once diagnosis of POTS is made. POTS may be “primary” or “idiopathic,” with no known cause. Other cases are “secondary” with another disease or condition known to contribute to development of POTS; a few of the many diseases known to contribute to development of the syndrome are amyloidosis, diabetes, multiple sclerosis, and hepatitis C. POTS sometimes develops following a viral infection. POTS is associated with hypermotility. It has been linked to brain trauma and concussion in some cases, and is associated with a metabolic disorder in a small group of patients. POTS may overlap with other conditions such as chronic fatigue syndrome (CFS), neurally mediated syncope (NMS), or physical deconditioning. About 80% of POTS patients are female, and most of them are of childbearing age (many under the age of 35). POTS patients often have sympathetic nervous system activation demonstrated by hypovolemia and above normal levels of plasma norepinephrine when standing. Roughly half of all POTS patients suffer from small fiber neuropathy. Patients with POTS often experience venous pooling, fatigue, visual changes, headaches, light-headedness, heart palpitation, exercise intolerance, insomnia, early satiety, joint or muscle pain, diarrhea or constipation, nausea, inability to concentrate, tremors, syncope, cold and/or painful extremities, chest pain, and shortness of breath. Many patients have a worsening of symptoms associated with hot or cold temperatures, loud noises, and bright lights. A worsening of symptoms often occurs in autumn and winter. The impairment experienced with POTS is similar to that of chronic obstructive pulmonary disease (COPD) or congestive heart failure (CHF). About 25% of individuals with POTS are unable to go to work and must often go on disability. Quality of life among POTS patients has been found to be similar to individuals with kidney failure on dialysis. Treatment for POTS includes: Drinking two to three liters of fluid a day Increasing sodium intake to 3000-10000 mg a day No caffeine Eating on a regular schedule (no skipping meals) Avoidance of alcohol Cooling vests in hot weather Wearing compression stockings Raising the head of the bed Doing reclined exercises such as rowing and recumbent biking Medications such as fludrocortisone, beta blockers, midodrine, clonidine, pyridostigmine, benzodiazepines, SSRIs, SNRIs, erythropoietin and octreotide Mayo Clinic surveyed pediatric POTS patients seen between 2003 and 2010. Among those who responded to the survey, 18.2% experienced a complete recovery from POTS, and 52.8% continued to have symptoms, but noted improvement. Male patients were twice as likely to have recovered. The average respondent had POTS for about five years at the time of the survey. Both the patients who fully recovered and those who did not had mental health scores similar to the national norm. About 80% of POTS patients have a relapsing-remitting course, with symptoms that come and go. Up to 75% of pediatric patients diagnosed with POTS will have either an improvement or resolution of symptoms by 21-25 years of age. References and recommended readings Postural Orthostatic Tachycardia Syndrome. Dysautonomia International website. http://www.dysautonomiainternational.org/page.php?ID=30. Accessed March 4, 2015. Postural Orthostatic Tachycardia Syndrome. The Children’s Hospital of Philadelphia website. http://www.chop.edu/conditions-diseases/postural-orthostatic-tachycardiasyndrome#.VKp6qFaVj-Y. Reviewed March 3, 2014. Accessed March 4, 2015. Postural tachycardia syndrome (POTS). Rare Diseases Research Network website. https://www.rarediseasesnetwork.org/ARDCRC/patients/learnmore/POTS/. Accessed March 4, 2015. POT syndrome. MedicineNet.com website. http://www.medicinenet.com/pot_syndrome/article.htm. Reviewed October 4, 2011. Accessed March 4, 2015. Review Date: 1/5/15 Contributed by Elaine Hinzey, RDN, LD/N