POTS_Templates
advertisement

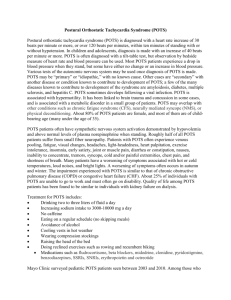
SAMPLE POTS TREATMENTS/PATIENT PLAN PATIENT NAME HEALTH PLAN Physician Information Addressing/Treating Medications/Appointments Appointments Medications Action Items Physician Action Items Patient Action Items Complete Items Primary Care Dr. Name/Info Cardiology Dr. Name/Info Not have my condition, and organizing my condition, take over my life. Blood Pressure Variations Central Line/Fluids Mental Fog Physical Activity Gastroenterology Dr. Name/Info Pain Management Dr. Name/Info Psychiatry Dr. Name/Info Neurology Dr. Name/Info Rheumatology Dr. Name/Info Goal Octreotide – 250mcg QID D5 Saline 1L .9% NaCl 1L BID Adderall – 10mg BID Cancel Appt Ordered Medication Order aggressive PT for home. 4/1 Tilt Table Test Nausea/Vomiting Chest Pain Be able to stand up and go places without an escort. Keep blood sugar in range. Eat on a schedule. Keep BP under 140/90. No Infections this year Keep my professional persona alive. Do my program 3 days a week. Be able to swim a mile without stopping. Not get nauseous before, during, and after every meal. Only puke once a week. Be free from pain. Only need meds 2 days a week Be at peace with my condition. Figure out how to handle pain without drugs. Know what triggers crashes and prevent them. Understand why I shake and stop it. Be able to walk down stairs. Be able to run 5 miles Patient Burden Chest Pain, Shaking Joint Pain Page 1 of 5 SAMPLE POTS TREATMENTS/PATIENT PLAN POTENTIAL PHARMACOLOGICAL/PHYSICAL THERAPIES Category Treatment Article Notes/Citations referenced in (#) article Dosage POTS type Negative Outcomes Diet Don’t eat carbs. (2)(3) Exercise Reconditioning (1)(2)(3) Aerobic exercise 20 min 3 times/wk PD, H If too vigorous, may worsen symptoms Hydration (1)(2)(3) 2 L/d PD Edema Salt (1)(2)(3) 2–4 g/d PD Edema Saline Vasoconstrictors Compression Socks N/A N/A Fludrocortisone acetate (1) Alternative is DDAVP (2) Use w/ salt tablets. May reduce renin! (3-9) 0.1–0.2 mg qd PD Hypokalemia, hypomagnesemia, edema Midodrine (ProAmatine) (1) Add to Fludrocortisone/DDAVP (2)Don’t use long term (3-10) 5–10 mg tid PD Nausea, itching scalp, supine hypertension Page 2 of 5 SAMPLE POTS TREATMENTS/PATIENT PLAN Clonidine HCI (Catapres) (1)(2)(3) Hyperadrenergic 0.1–0.3 mg bid; 0.1–0.3 mg patch/wk H Dry mouth, blurred vision Desmopressin acetate (DDAVP) (1) Alternative is DDAVP (3) 0.1–0.2 mg qhs PD Hyponatremia, headache Octreotide acetate (Sandostatin) (1) For Refractory Pts (2) Use if eating (splanchnic pooling) is a problem (3) helps, but SQ 50–200 μg SC tid PD Nausea, diarrhea, gallstones, SC Erythropoietin (Epogen, Procrit) (1) If nothing else works (2) Can help increase cell mass but expensive and risky. (3) helped symptoms, no major reduction in OT (1) if Midodrine isn’t tolerated (2) (3) 10 000–20 000 U SC/wk PD Pain at injection site, expensive 5–10 mg tid PD Anorexia, insomnia, dependency Methylphenidate (Ritalin, Methylin, Concerta, etc.) Others (2): Ergotamine, Ephedrine, Pseudoephedrine, Yohimbine, Theophylline (3) Phenylepherine Page 3 of 5 SAMPLE POTS TREATMENTS/PATIENT PLAN ACH Inhibitor SSRI SRNI (1) If Vasoconstrictors don’t work, try these. (1) SNRIs are better than SSRI for POTS (3) They anecdotally work Betablockers Pyridostigmine bromide (Mestinon) (1) Use for postviral/autoimmune (2) (3)(5-7)(9-10) 30–60 mg qd PD Nausea, diarrhea Escitalopram oxalate (Lexapro) (1) if SSRI is used, use with a SNRI (duloxetine/venlafaxine) (3) They anecdotally work 10 mg qd PD, H Tremor, agitation, sexual problems Bupropion (Wellbutrin XL) (1) 150–300 mg qd PD, H Tremor, agitation, insomnia Duloxetine HCI (Cymbalta) (1) Use w/ SSRI 20–30 mg qd PD, H Nausea, sleep disturbance Venlafaxine HCI (1) Use w/ SSRI (3) anecdotally works 75 mg qd or bid PD, H Nausea, anorexia, tremor Others (3) reboxetine and Sibutramine Bisopropol (2) Use w/ fludrocortisone Page 4 of 5 SAMPLE POTS TREATMENTS/PATIENT PLAN Alpha-2 agonists Sinus Node Blocker (1) (2) (3) (4) (5) (6) (7) (8) (9) (10) Propranolol (2) Use in low doses (3) 10mg longterm works Labetalol HCI (Trandate, Normodyne) (1) combined alpha/beta labetalol/carvedilol may work better Toprol (4,7,8) Methyldopa (2) (3) very limited evidence. Ivabradine (2) may be better than beta blockers for sinus tach (3) helps tach w/o messing with BP 100–200 md bid H Fatigue H Grubb, Blair. Postural Tachycardia Syndrome Clinican Update. American Heart Association. 2008. Abed, Howraa. Diagnosis and Management of POTS. Journal of Geriatric Cardiology. March 2012. A review of postural orthostatic tachycardia syndrome. Europace. 2009. Brady, P. Inappropriate sinus tachycardia and Overlapping Syndromes. October 2005. PACE. Vol 28. Pp 112-1121. Kanjawal, Y. The Postural Orthostatic Tachycardia Syndrome: Definitions, Dignosis, and Management. PACE. August 2003. Vol 26, pp 1747-1757. Autonomic Nervous Sytem Disorders. Merck Manual. Low, P. Postual Tachycardia Syndrome. March 20009. Journal of Cardiovascular Electrophysicology. Vol 20. Pp 352-358. Thieben, M. Postural Orthostatic Tachycardia syndrome: The Mayo Clinic Experience. March 2007. Mayo Clin Proc. Vol 82. Pp308-313. Maule, S. Orthostatic Hypotension: Evaluatino and treatment. Cardiovascular and Haematological Disorders – Drug Targets. Vol 7. Pp 63-70 Grubb, B. The postural tachycardia syndrome. A concise guide to diagnosis and management. January 2006. J. Cardiovac Electrophysiol. Vol 17. Pp 108-112. Page 5 of 5