Student Radiographers
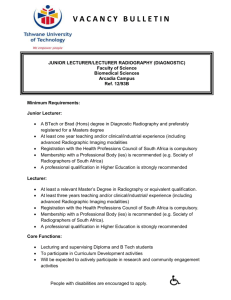
advertisement

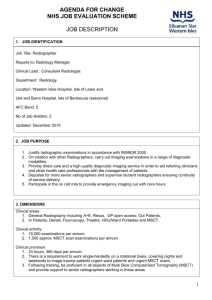
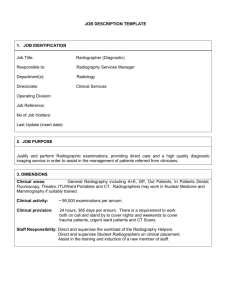
AGENDA FOR CHANGE NHS JOB EVALUATION SCHEME JOB DESCRIPTION 1. JOB IDENTIFICATION Job Title: Radiographer Reports to: Radiology Manager. Clinical Lead : Consultant Radiologist Department: Radiology Location: Western Isles Hospital, Isle of Lewis and Uist and Barra Hospital, Isle of Benbecula (sessional) AFC Band: 5 No of Job Holders: 2 Updated January 2015 2. JOB PURPOSE 1. Justify radiographic examinations in accordance with IR(ME)R 2000. 2. On rotation with other Radiographers, carry out imaging examinations in a range of diagnostic modalities. 3. Provide direct care and a high quality diagnostic imaging service in order to aid referring clinicians and other health care professionals with the management of patients. 4. Deputise for more senior radiographers and supervise student radiographers ensuring continuity of service delivery. 5. Participate in the on call rota to provide emergency imaging out with core hours. 3. DIMENSIONS Clinical areas: 1. General Radiography including A+E, Resus, GP open access, Out Patients, 2. In Patients, Dental, Fluoroscopy, Theatre, HDU/Ward Portables and MSCT. Clinical activity: 1. 15,000 examinations per annum. 2. 1,500 approx: MSCT scan examinations per annum Clinical provision: 1. 24 hours, 365 days per annum. 2. There is a requirement to work single-handedly on a rotational basis, covering nights and weekends to image trauma patients urgent ward patients and urgent MSCT scans. 3. Following training, be proficient in all aspects of Multi Slice Computerised Tomography (MSCT) and provide support to senior radiographers working in these areas. 1 Staff Responsibility: 1. Direct and supervise the workload of Radiographic Helpers and Radiographic Assistants. 2. Direct, supervise and assess Student Radiographers on clinical placement. 3. Assist in the training and induction of new members of staff. 4. ROLE OF DEPARTMENT 1. Provide a high quality, efficient and effective Radiology services to a diverse range of patient types and clinical conditions. 2. Diagnostic imaging equipment is used to carry out radiological examinations on adult and paediatric patients and reports are provided to referring clinicians. The report assists the referrer in providing a diagnosis of the patient’s condition in order to decide on an effective course of treatment and care. 3. Interventional Radiology is carried out to assist in the treatment of a patient’s condition. 4. The departmental clinical governance strategy ensures a high standard of care for patients undergoing radiological examination and promotes multidisciplinary team working. 5. Provide a suitable environment for the training and assessment of Student Radiographers 5. KEY RESULT AREAS Clinical 1. Act independently in the assessment of referrals for X-Ray examinations, taking full responsibility for the justification of general X-Ray examinations in order to reduce unnecessary ionising radiation exposure of patients in accordance with IR(ME)R 2000. 2. Ensure that patient radiation doses are kept as low as reasonably practicable by adoption of optimal radiographic technique/ exposure factors/ shielding as described in departmental protocols. 3. Maintain a high level of expertise in the safe operation of all X-Ray equipment and manage faults effectively as per departmental fault reporting procedure. 4. Provide advice verbally to clinicians on the nature of a diagnostic image. 5. Work as part of a team to ensure effective communication and delivery of care. 6. Prioritise workload depending on the severity of a patient condition and the direct impact on their management; organise Radiographer cover appropriately. 7. Liaise with fellow healthcare workers and referring clinicians to provide a high quality imaging service to patients. 8. Maintain accurate patient records by input of accurate information to reflect the service provided and meet professional standards. 9. Participate in the out of hours on call system. 10. Work independently when providing an on call service to patients requiring urgent imaging due to acute trauma or illness, mainly overnight and weekends; prioritise workload depending on the severity of patients’ condition and the direct impact on their management. 11. Following the required departmental training and assessment of competence in both IV cannulation and contraindications to contrast media, perform IV cannulation for patients requiring the injection of contrast media in accordance with departmental protocols. 12. Maintain the required knowledge and skills to provide effective training keeping up to date with current advances in technology and diagnostic techniques. 13. To be prepared to undertake training in all aspects of the CT scan service to enable independent working within this area, and to provide a comprehensive on-call service, if and when the service is required. 14. Ensure safe and efficient use of CT scanner. Take action to resolve faults/problems following the fault reporting procedure. 15. Critically analyze radiographs to maintain a high standard of Radiography and to determine the need for additional images to further aid patient diagnosis. 16. Be responsible for Radiation Protection of self and other members of staff/ visitors by ensuring compliance with Departmental Local Rules and Systems of Work. 17. Direct other staff as necessary in wearing of Lead Aprons/ Thyroid Shields and correct positioning to minimise radiation dose in the course of their work. 2 18. Maintain a clean and safe working environment for both patients and staff in accordance with infection control policies. Managerial 1. Be able to exercise personal responsibility and make decision in complex and unpredictable circumstances e.g. imaging in A+E and theatre during a multiple trauma situation. 2. Be actively involved and ensure Radiographers are committed to departmental Audit and Quality Assurance, maintaining effective Clinical Governance, thus enabling change to departmental policies, procedures and practices. 3. Work together with senior radiographers, radiographic helper (summer post only) and radiographic assistants, to achieve the desired quality of patient care and optimum imaging 4. Maintain all documentation and comply and be involved in the revision and implementation of departmental and professional policies and protocols such as: a. Health & Safety including risk assessment and Control of Substances Hazardous to Health (C.O.S.H.H.) b. Radiation Protection Procedures including Local Rules and Systems of Work c. Ionising Radiation (Medical Exposures) Regulations 2000 - IR(ME)R2000 d. Child Protection Procedures e. Quality Assurance Program f. Clinical Effectiveness g. Departmental Imaging Protocols h. Data Protection i. Code of Professional Conduct. j. Infection Control (both hospital and specific departmental procedures) 5. Contribute to the betterment of the clinical service by approaching the Senior Radiographers with ideas for discussion. 6. Deputise for the senior staff to maintain continuity of service in their absence prioritizing the patient’s needs before clerical duties. Educational 1. Participate in mandatory training (Cardio Pulmonary Resuscitation, Moving and Handling, Violence and Aggression, Infection Control and Fire Safety) and actively pursue and provide Continuous Professional Development keeping an up to date personal record. 2. Maintain knowledge of technological and technical advances in methods of diagnostic Imaging in order to promote a culture of continuous improvement within the department. 3. Develop knowledge and understanding within an evidence-based framework and transfer to situations encountered in practice. 4. Participate in Radiography ‘in-service’ and contribute to promote personal development and educational opportunities in the department. 5. Take responsibility for implementing a Professional Development Plan (PDP), highlighting any difficulties in achieving goals. 6a. EQUIPMENT AND MACHINERY 1. Ceiling suspending general X-Ray tubes (Digital Radiography) , static X-Ray tables with rise and fall function and floating top, bucky assemblies (erect and supine) and operator console. These are used for general x-rays e.g. chest, abdomen and extremities. 2. Digital Fluoroscopy equipment with flat plate detectors in a multipurpose room used for screening examinations such as Barium swallows and Barium enemas. 3. Mobile X-Ray units: Battery operated x-ray equipment that is capable of being used remote from department for A & E, ward and theatre Radiography 4. Mobile Image Intensifiers for Theatre Fluoroscopy, used for orthopaedic, surgical and urology cases. 3 5. Orthopantomogram (OPG) and lateral cephalostat unit for dental and Maxillo Facial/orthodontic referral. 6. State of the art 64 Slice CT (computerised tomography) Scanner including table and gantry, operator console and post processing hardware/software used for image manipulation and storage. 7. Contrast injector pump and CO2 insufflator for colonography. 8. Computerised Radiography system (CR) consisting of sophisticated image display and manipulation software, as well as associated hardware including CR Cassettes, CR Readers, monitors and laser printer. 9. Digital Radiography, RIS, National PACS. 10. Computers. 11. Label Printers. 12. Immobilisation devices such as foam pads and bucky bands. 13. Patient slides for transfer onto CT table and general X-Ray table. 14. Patient Hoists 15. Patients are moved around the X-Ray Rooms/Department on trolleys and chairs when required 6b. SYSTEMS 1. RIS (Radiology Information System) for patient registration, link to PACS and data management. 2. CR (Computerised Radiography) System including image manipulation and storage software. 3. DR (Digital Radiography) System for exposing, storing and image manipulation. 4. National / Local PACS (Picture Archive and Communication System) for storage, access and transfer of images locally or to and from the national Archive.. 5. Manual records if PAC system is down. 6. Access the internet and trust intranet via the resource room PC or the e-library to access relevant information for personal and professional development. 7. Use software programs such as Microsoft word and excel to create documents and tables. Used for quality assurance and audit. 8. Handling of patient medical notes. 9. Recording daily contrast media and cannulation in CT department. 7. ASSIGNMENT AND REVIEW OF WORK 1. The Radiology Manager, Senior Radiographers and Radiologist will be available to consult on a daily basis and provide allocation of duties and training when required. 2. Demands for diagnostic imaging are generated by the specific service needs of each clinical area from within the Board. Images must be suitable for diagnosis and archived on the PACS. 3. Radiology Manager or Senior Radiographers may not be available to consult on an out of hours 4 basis to provide direct supervision. If senior staff are not available, the post holder will therefore work on own initiative. A Radiologist will be available for consultation as part of the Radiology Obligate Network with a mainland Health Board. 4. Radiology Manager or Senior Radiographers will delegate other non-clinical tasks. 5. Radiology Manager will undertake appraisal in order to agree an annual performance development plan. 8. DECISIONS AND JUDGEMENTS 1. Be accountable for own professional actions, working independently. 2. Routinely using skills to assess a patient’s condition, often acute, and decide on an appropriate method to obtain a radiograph from a range of options. 3. When acting in the role of practitioner under IR(ME)R decide whether an X-Ray request is justified as the correct examination to diagnose a patient’s condition. 4. Plan and prioritise own patient workload e.g. managing in-patient work flow and whilst on-call. 5. Decide when to refer to a Senior Radiographer for help or advice. 6. The final decision to X-ray or not X-Ray a patient is the Radiographer’s responsibility. 7. Follow the Departmental fault reporting procedure. 8. Access condition of patient to determine if a reaction is exhibited after contrast has been administered. 9. MOST CHALLENGING/DIFFICULT PARTS OF THE JOB 1. On a daily basis be prepared to operate Imaging Equipment in differing and demanding environments. 2. Being able to manage an unpredictable work load effectively and interact successfully with fellow health care professionals 3. Give assistance to Senior Radiographers, being actively involved oneself in performing X-Ray examinations at all times. 4. Cope with the mental and physical demands of working in acute areas, independently, sometimes having to provide images on severely injured, abusive or violent patients 5. Combining training in new techniques or newly procured equipment with normal patient workload. 6. Supervise and train Student Radiographers whilst maintaining a high throughput of patients. 7. As the only Radiographer on call for the hospital overnight and at weekends meet the demands of Accident and Emergency whilst also covering emergency CT’s, portables and urgent InPatient referrals. 8. Exposure to unpleasant odours and bodily fluids frequently throughout the day. 9. Producing high quality CT scans/radiographs under challenging circumstances especially on-call. 10. Duties can be reassigned at short noticed to allow for staff shortages. 11. Aware of how quickly a controlled and stable situation can become an emergency, life threatening. 12. Multi-tasking between one specialist modality and another on a daily basis. 13. Keeping up to date with ever changing technology. 14. Combine training in new techniques/newly procured equipment with normal patient workload while being based at a rural hospital. 15. Maintain and continually develop clinical knowledge and skills while living and working in a remote and rural location. 5 10. COMMUNICATIONS AND RELATIONSHIPS Patients: 1. Provide information by explanation of often-complex procedures, listening to the patient’s requirements in order to encourage compliance with the imaging process. CT can be claustrophobic so adequate patient preparation is essential. Some patients will have a barrier to understanding or be unable to communicate. 2. Patients will have injuries or illness that will require the adaptation of the imaging technique, utilisation of developed motivational and persuasive skills to acquire correct position and reduce mobility to produce an acceptable diagnostic image. 3. Advise and assist colleagues in their handling of patients concerns. 4. When requested provide reassurance and factual information regarding the risks associated with an imaging procedure. 5. After the examination the patient understands the procedure for receiving their results and advised of appropriate aftercare when necessary. Radiologists: 1. Discuss the patients imaging protocols in order to produce optimal examination. 2. Seek advice when necessary. Relatives/Carers: 1. Provide reassurance and receive information 2. Ask for assistance with, and instruct in methods of immobilisation, maintaining Radiation Protection. 3. Provide information using tact and diplomacy in the context of the regulations governing the Data Protection Act. Radiography Staff (internal/external): 1. 2. 3. 4. 5. Consult Senior Staff for advice Delegate tasks to Radiographic Helpers and SATO. Discuss department policies and suggest improvements Pass on information relating to patient transfer to colleagues Provide advice and assistance to other members of staff. Medical Staff/Nurse Practitioners: 1. 2. 3. 4. 5. 6. Query incorrect or unnecessary referrals in order to reduce patient radiation dose Provide advice on guidelines for relevant X-ray or CT examinations Provide and explain instructions for patient preparation prior to imaging Provide and explain advice for aftercare of patients following imaging procedures Provide advice on the nature of an image Seek help and advice with patients in pain or who are immobile Student Radiographers: 1. Decide whether the Student is capable of performing an examination safely with the patient’s consent and after suitable tuition 2. Advise the student as to the best professional practice in any situation 3. Provide constructive criticism as part of the assessment process for an individual examination. 6 11. PHYSICAL, MENTAL, EMOTIONAL AND ENVIRONMENTAL DEMANDS OF THE JOB Physical Skills: 1. Manipulate and position all patients providing immobilisation when required, for their x-ray or CT examinations which demands a high degree of accuracy to minimise radiation dose. 2. Have the expertise to handle and operate highly specialised and expensive x-ray equipment. 3. Following the appropriate training perform IV cannulation for patients undergoing IVU and CT examinations and inject contrast media, which carries the risk of anaphylactic reaction. 4. Be able to work at speed when performing radiographs and CT for a critically injured patient often prior to emergency surgery. 5. Possess keyboard skills for the entry of data into the RIS, CR, DR and National PACS. 6. Possess computer skills for making patient appointments. 7. The setting up and filling of the injector pump must be carefully done to avoid contamination and ensure that no air is injected into the patient. 8. For mobile units there is a requirement to precisely manoeuvre large, unwieldy equipment in restrictive places e.g. in Theatre, in the side rooms on the ward or in a sterile environment. These units are positioned using multi-planar locks. This requires significant hand-eye coordination and spatial awareness. Physical Demands: 1. Maintain a level of physical fitness to frequently move ceiling mounted X-Ray tubes throughout three dimensions during all shifts. 2. Walk long distances when driving mobile X-Ray units to carry out ward radiography throughout a shift when required. 3. The majority of the working day and night is spent standing and walking and bending to position patients. 4. Cleaning of X-ray equipment regularly and changing mattress sheets involves bending and lifting. 5. Frequent transfer of patients from trolleys, beds and chairs onto X-Ray or CT tables requires the use of safe lifting and handling skills, using mechanical aids when required. 6. Carry large cassettes to and from the X-Ray facility to the CR Reader. Mental Demands: 1. Providing supervision to students when performing and assessing one’s own examinations requires frequent concentration in unpredictable situations throughout the majority of the shift period. 2. Prioritising workload requires diplomatic skills in discussion with referrers who all believe their patient should take priority. 3. When on call at night or weekend take responsibility for the entire radiography service alone, managing patients and equipment. 4. Should imaging equipment malfunction during an examination (occasionally during a theatre case), evaluate the situation and, where appropriate, provide an immediate solution. 5. The CT scanning procedure involves a series of multiple tasks prior to the scan involving intense concentration at the same time keeping the patient at ease. 6. Due to the high dose of radiation involved in CT scanning, means that there is absolutely no margin for error. This puts strain on the CT operator particularly in an emergency situation when working independently at night. 7. Occasionally in the case of CT breakdown, offer apologies to referrers and patients, handling patient’s complaints as a result. Emotional Demands: 1. Perform radiographic examinations, including CT, and care to terminally ill patients. 2. Provide examinations for critically injured patients in the accident and emergency department, sometimes bleeding heavily with distorted or severed limbs and/or severe burns. 3. Move quickly from a routine examination to an acute setting due to sudden and unpredictable demand e.g. X-Ray of a painful finger with no history of trauma to a victim of a road traffic accident 7 requiring multiple X-rays, independently taking responsibility for the diagnostic imaging service to that patient. 4. Communicating with distressed/anxious/worried patients/relatives. 5. X-raying a patient when there is a query of a Non Accidental Injury (NAI). Working Conditions: 1. Tiredness may result from working a 9-5 shift and going on call at 5pm and finishing at 9am the following day. 2. Exposure to unpleasant odours and bodily fluids frequently throughout all shifts. 3. Be required to wear heavy lead rubber aprons during Fluoroscopy Procedures sometimes in a hot theatre environment. 4. Risk of exposure to scattered Ionising Radiation particularly during fluoroscopic procedures. 5. Moving from cold air conditioned areas to hot conditions in the working areas. 6. Working constantly in artificial lighting with little or no natural daylight. 7. Potentially exposed to verbal abuse from some patients. 8. A risk of physical abuse from patient’s who may be confused, disorientated etc. 9. Work in cool conditions to facilitate the necessary temperature for the computers to operate the CT scanner. 12. KNOWLEDGE, TRAINING AND EXPERIENCE REQUIRED TO DO THE JOB 1. HPC Registration 2. BSc (HONS) in Radiography 3. Evidence of Continuing Professional Development, including an up to date portfolio. 4. Evidence of the required experience, knowledge and skills acquired through Radiographer rotation through operational areas in Diagnostic Radiology. 5. Ability to take responsibility and act in a supervisory capacity. 6. Good communication skills. 7. Team Worker 13. ORGANISATIONAL POSITION See attached sheet 14. JOB DESCRIPTION AGREEMENT I agree that the above Job Description is an accurate reflection of my duties and responsibilities at the date of signing. Job Holder’s Signature: Date: Manager’s Signature: Date: 8 PERSON SPECIFICATION Job Title: Radiographer AFC Band 5 Department: Radiology Main Location: Western Isles Hospital, Stornoway, Isle of Lewis FACTOR ESSENTIAL DESIRABLE EXPERIENCE Undergraduate experience in a wide range of diagnostic imaging investigations Proven ability to work independently as well as part of a team QUALIFICATIONS TRAINING RESEARCH PUBLICATIONS Diploma of the College of Radiographers or a Bachelor of Science in Diagnostic Radiography or equivalent. Evidence of ongoing professional development HPC Registration KNOWLEDGE AND SKILLS DISPOSITION Ability to undertake all forms of general radiography Good communication skills Exposure to and some knowledge of advanced imaging techniques and modalities Ability to prioritise and good time Management Experience of MSCT scanning Evidence of understanding of the specific challenges of remote and rural working Experience of lone working out of hours (OOH) Ability to work in a pressurised, acute environment Ability to work unsupervised Flexible to meet the changing needs of the service. OTHER Driving Licence and use of a vehicle 9 RADIOLOGY ORGANISATIONAL CHART NHS WI Radiology Directorate Radiology Department Manager Band 7 Sonographer Radiographers x 3 Band 6 Senior Radiographers X 5 Band 5 Radiographers x 2 (Vacant post) System Administrator x 1 Radiographic Assistant x 2 Radiology Admin Assistant x 1 (Service Change posts yet to be banded under AFC) Band 2 Summer Helper Summer Helper Summer Helper Student Radiographers/ Work placement students 10