Human Tissues II
advertisement

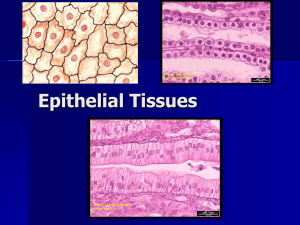
CLASS: 11:00 – 12:00 DATE: November 1, 2010 PROFESSOR: Cotlin I. II. III. IV. V. VI. VII. HUMAN TISSUES II Scribe: Adam Baird Proof: Page 1 of 7 PSUEDOSTRATIFIED CILIATED COLUMNAR EPITHELIUM [S56] a. Picture of psuedostratified epithelium b. Notice that the nuclei don’t line up very nicely. c. It is a simple layer. d. All of the nuclei are sitting at the basement membrane, but they don’t all necessarily reach the lumen. e. These cells are ciliated, which is seen in many pseudostratified layers. STRATIFIED EPITHELIUM [S57] a. Picture of stratified epithelium; “stratified” mean “multiple layers”. b. First picture reviewed: stratified squamous c. Second picture reviewed: stratified squamous d. Third picture reviewed: cuboidal/columnar NON-KERATINIZED STRATIFIED SQUAMOUS EPITHELIUM [S58] a. Picture of non-keratinized stratified squamous epithelium. b. What is the difference between a keratinized layer and a non-keratinized layer? A keratinized layer will be seen on the outer layers of the skin. So, our entire epidermis is stratified squamous epithelium (keratinized in most areas). Our oral cavity and esophagus is all stratified squamous. So in the outer regions of the mouth (near the skin) are keratinized; the inner regions of the oral cavity and the esophagus are squamous. The rest of the GI is columnar. The anal region is squamous. c. This is vaginal epithelium, which is also non-keratinized stratified squamous epithelium. Notice the basement membrane. Notice the lumen. Notice the outer-most layers are very thin. Notice the connective tissue and muscle. d. Sometime the cells of stratified layers will look like they are “sloughing” or “falling” off. The outer-most cells are still intact in a non-keratinized layer though. KERATINIZED STRATIFIED SQUAMOUS EPITHELIUM [S59] a. This is what a keratinized layer looks like. b. This is a picture of epidermis. Notice the dermis. Notice the basement membrane. Notice the epidermis. c. The living cells here are all squamous. d. The primary cells of epidermis are called keratinocytes, which produce large amounts of keratin. e. Keratin is an intermediate filament. f. Notice the dark line on this picture, which is formed from keratinocytes (because they make lots of keratin). These cells are undergoing an orchestrated cell death process: 1. The cells will die (apoptosis) 2. All that’s left is the “shell” of the cell 3. The keratin that is left over forms a network of “keratin molecules” g. Notice the living tissue. Notice the dead cells that are still together, forming the tight network of keratin molecules; this tight network acts as another layer of protection for our skin. h. Thin, smooth areas of our skin don’t have much keratin (like skin creases, skin around the areas of our joints, etc.); other areas have very thick layers of epidermis (like the palms of our hands, soles of our feet, etc.). i. A callus is formed from the body’s response to make more keratin. If you do a lot of yard work, for example, and develop blisters (abrasions), that’s just the body “bulking up on keratin” in hopes to thicken that area. KERATINIZED STRATIFIED SQUAMOUS EPITHELIUM [S60] a. This picture is looking a little closer up (higher magnification). Notice the relatively small (almost invisible) basement membrane. Notice the epidermal cells. Notice the dark line (made up of keratin molecules). Notice the stratified granulosa. Notice the grainy layer (where cells are dying). All that is remaining is the “husk of the shell” of the dead cell. b. Notice the “peaks and valleys” of the dark line. The material in between the peaks (the area that fills the valley) is the lamina propria. c. By definition, if a slide were labeled “stratified squamous”, you would assume that it would be non-keratinized. It is still important to distinguish between keratinized and non-keratinized when identifying stratified squamous slides though. STRATIFIED CUBOIDL EPITHELIUM [S61] a. Here is a picture of stratified cuboidal epithelium. b. Stratified cuboidal epithelium (and columnar epithelium) is pretty much localized to ducts works and glands. c. Notice the nice cuboidal layer, as well as the stratified cuboidal layer. STRATIFIED COLUMNAR EPITHELIUM [S62] a. Here is a picture of stratified columnar epithelium. b. Stratified columnar epithelium is defined by the outermost layer (the “luminal-most” layer). c. Some of layers may look cuboidal, but they are actually columnar. CLASS: 11:00 – 12:00 Scribe: Adam Baird DATE: November 1, 2010 Proof: PROFESSOR: Cotlin HUMAN TISSUES II Page 2 of 7 VIII. TRANSITIONAL EPITHELIUM [S63] a. We already talked about these a little bit. IX. TRANSITIONAL EPITHELIUM [S64] a. Notice the basal layer, stratified layer. b. This tissue will usually be seen in the “relaxed state” (because it has to have at least some pressure to get it distended). So if a section is opened up, it will distend because isn’t under pressure. X. TRANSITIONAL EPITHELIUM [S65] a. These cells may look cuboidal, and it may look stratified or even stratified squamous, but a closer looks shows that the outermost cells are cuboidal (sometimes described as “umbrella cells” because they have an outer puffiness). You can imagine that those outermost cells, when relaxed, will look like a cube. As they get pressure surrounding them, all of these cells will spread out and may even look squamous. BEGINNING OF THE NEXT POWERPOINT (INTRODUCTION TO HUMAN TISSUES II) XI. XII. XIII. XIV. XV. XVI. INTRODUCTION TO HUMAN TISSUES II [S1] a. For this lecture, we’ll be discussing glands. b. Why are we talking about glands though? Yes, we have a lot of them (like in our eyes, mouth, sweat glands, mucous glands lining GI tract, etc.). c. But more importantly, why are we talking about glands having just discussed epithelium? Because all glands are derived from epithelium. Glands are lined with epithelium too. d. TYPES OF GLANDS [S2] a. In the broadest sense, glands can be classified into two groups: 1. Exocrine Glands a. Cells that will secrete their products directly into the lumen. Those products will be carried through a duct (a tube system) and deposited somewhere else. 2. Endocrine Glands a. Composites of cells that will their products directly into themselves (into the matrix around them) and then be picked up into the blood stream (usually via a capillary system). b. For today’s lecture, we’ll mainly discuss exocrine glands. THE DEVELOPMENT GLANDULAR EPITHELIUM [S13] a. Glandular epithelium is derived from epithelium. b. The left figure will help explain exocrine development: 1. Here is the basic epithelium. There will be proliferation very early in development, which is like a “down-growth” into the tissue below. 2. Here is the epithelium. They have grown to the point that they have started to organize. Specific secretory cells will collect at the bottom. There will also be a maintained duct. All of the products will be secreted into this duct and carried out into the lumen. 3. Recall: These cells secreting into a duct work and they flow away c. The right figure will help explain endocrine development: 1. (Very similar to exocrine development.) There will be “down-growth” into the tissue below. Specific secretory cells will collect at the bottom. The stalk (or any type of duct work) disappears, leaving a packet of secretory cells with no duct. Basically, it’s a bunch of cells that are highly vascularized. 2. Recall: These cells will secrete right into the matrix around them, being picked up by the blood and carried away. OVERVIEW OF AN EXOCRINE GLAND [S4] a. The secretory portion is usually referred to as the acinus. The conducting port (which is just carrying the fluid) is referred to as the duct. b. Most are usually lobed. It looks similar to “grapes on a string/branch”. Imagine that this is branch, and all of the yellow ducts are progressive branches (they get smaller and smaller). The bundles are filled with secretory material. c. So there are many little bundles, connected to a tube, which is connected to a major gland. d. So, the carotid gland, for example, looks like this. EXOCRINE GLANDS CAN BE BASED ON THE FOLLOWING [S5] a. Exocrine glands can be defined based on how they are organized – their structure versus what they are secreting versus the mechanisms of those secretions. CLASSIFICATION BASED ON STRUCTURE [S6] CLASS: 11:00 – 12:00 Scribe: Adam Baird DATE: November 1, 2010 Proof: PROFESSOR: Cotlin HUMAN TISSUES II Page 3 of 7 a. Don’t worry about all of these labels. b. In summary, exocrine glands can be classified based on their structure: 1. Simple 2. Simple branched 3. Simple coil 4. Simple acinar 5. Compound (multiple branches) c. Many of our sweat glands are classified as simple. d. Salivary and mucous glands (along the GI tract, for example) are classified as compound. e. In all situations, these classifications have ducts that coalesce into larger ducts work. XVII. OVERVIEW OF SALIVARY GLAND [S7] a. This is a larger salivary gland. b. Notice that the acinar region looks cuboidal. c. There is a progression of layers though. Some of the duct looks “low cuboidal”. The interior layer is cuboidal. The lumen gets larger as more secretory products are moved through. The cells get larger as more secretory products are moved through as well. d. Because of the layer progression, it’s difficult to label exocrine glands. Some will look cuboidal, others may look pseudostratified (like a mix between columnar and stratified), still others (the large ones) may look stratified columnar…it’s a progression. It’s difficult to differentiate between where the duct starts and where the duct ends. e. Don’t worry about the specific terms here (like intercalated, striated, etc.). We’ll discuss them later. XVIII. CLASSIFICATION BASED ON SECRETORY PRODUCTS [S8] a. Exocrine glands can be classified based on what they secrete. 1. Serous secreting glands – Secrete lots of protein material, digestive enzymes, etc. a. Example: Parotid gland secretes amylase and lysozymes to help degrade our food. 2. Mucous secreting glands – Secrete a water, glycoprotein mix (mucous); found in esophagus and anal region for lubrication. 3. Mixed secreting glands – Secrete a mixture of mucous and serous secretions. 4. Don’t worry about intercalated and striated (which are part of the duct system). b. Notice the yellow structures. Myoepithelial cells cage the acinar glands of many glands. Myoepithelial cells are simply epithelial cells with muscle activity. (“Myo” indicates “muscle activity”.) So when material needs to be secreted, the myoepithelial cells contract, squeezing the material out (secretion). This is needed because there is no peristalsis in the ductwork. (Exceptions are restricted to the pancreas.) XIX. MYOEPITHELIUM CELL [S9] a. Here is a nice picture of myoepithelial cells. b. Bottom left picture: Stained brown for actin molecules, which “criss-cross” around the cell. When actin molecules get the signal to contract, they are able to move all of the material out. XX. SEROUS SECRETORY CELLS [S10] a. This is what serous secreting glands look like. b. Notice the little pink dots, which are secretory vesicles that are ready to be released when signaled. c. Recall: all protein material moves through the secretory pathway. XXI. MUCOUS SECRETORY CELLS [S11] a. This is very dense staining. It has a very dark, pixilated appearance (compared to mucous secreting glands that look like goblet cells because the cell volume is packed with secretory globules and droplets). So, the picture shows the nuclei being pushed to the edge, leaving the mucous filling visible. XXII. MIXED GLAND: SEROUS AND MUCOUS CELLS [S12] a. Parotid glands, for example, are mainly serous. b. Other glands, like the submandibular gland, are a mix between serous and mucous cells. XXIII. MECHANISMS OF EXOCRINE SECRETION [S13] a. There are 3 basic types of exocrine secretion. 1. Merocrine secretion - The basic type of secretion (by all cells) is exocytosis. Fibroblasts secreting collagen, for example, would be accomplished by exocytosis. Exocytosis, in this case, is known as merocrine secretion though. a. Vesicles fuse with the plasma membrane. Contents are dumped into the lumen. b. Most of the serous, mucous, and sweat glands (and most other glands) use merocrine secretion. 2. Holocrine secretion – Specific to sebaceous glands of the skin (which secrete oil through hair follicles for lubrication, for example). CLASS: 11:00 – 12:00 Scribe: Adam Baird DATE: November 1, 2010 Proof: PROFESSOR: Cotlin HUMAN TISSUES II Page 4 of 7 a. The whole cell is part of the secretory product. (“Holo” meaning “whole cell”.) The whole cell is released and disintegrated, and then the remaining contents are released. b. Restricted to sebaceous glands. 3. Apocrine secrection – Only parts of the apical membrane are pinched off (so the secretory product is actually pieces of cells). a. Only occurs in the mammary glands. Milk secretion has lots of fats and proteins. Some of the cells in milk secretion pinch off and are part of the released milk product. XXIV. HOLOCRINE SECRETION [S14] a. This is a sebaceous gland. b. It’s difficult to see, but there are small packets of material, which will eventually slough off the whole cell. XXV. MEROCRINE SECRETION [S15] a. Notice the secretory vesicles, which are fusing with the membrane. b. Whatever was in the vesicle is included in the secretion. c. This is basic exocytosis. XXVI. APOCRINE SECRETION [S16] a. This is mammary gland. Notice the simple columnar cells. b. Notice that whole parts of the cell are pinching and sloughing off. XXVII. CELLULAR ADAPTATIONS [S17] a. Pathology lectures will begin in a few days. Here are a few terms to keep in mind. 1. Hypertrophy – Increase in cell size 2. Atrophy (Hypotrophy) – Decrease in cell size a. For example: The cells of mammary glands will be short and fat at rest (hypotrophy). When they are signaled to produce milk, the cells will bulk in size and become broader (hypertrophy). 3. Hyperplasia – Increase in cell number 4. Hypoplasia – Decrease in cell number a. Note: There are tissues that can undergo both hypertrophy and hyperplasia. Sometimes the cells don’t hypertrophy though, but they can still exhibit hyperplasia as a way of making more of those same cells. 5. Metaplasia – transformation of one type of epithelium into another 6. Dyplasia – Abnormal (pathological) change in an epithelium XXVIII. EPITHELIUM RENEWAL [S18] a. Epithelium renewal: 1. Can be fast (as in intestinal epithelium, which is replaced every week) a. For example: As food is moved along the GI tract, stratified squamous cells of epithelial tissues are sloughed off, but are then regenerated. b. All of the tissue layers have stem cell basal populations. 2. Can be slow (as in large glands) 3. Can be variable (fast or slow) a. For example: More steady-producing areas may have a lower epithelium turnover rate. 4. In stratified layers, mitosis only occurs in the cells at the basal layer. a. For example: Cells that are attached to basement membranes will be the cells undergoing mitosis. Once the cells are pushed up in the layers, they lose the ability to regenerate. The basal stem cells are always the cells that are triggered for mitosis. 5. Capable of rapid repair and replacement of damaged cells. b. Carcinoma – Tumor of epithelial origin c. Adenocarcinoma – Tumor of glandular epithelium XXIX. SURFACE SPECIALIZATIONS AND CELL JUNCTIONS [S19] XXX. SURFACE MODIFICATIONS OF EPITHELIUM [S20] a. Recall: Cells can be defined by their surface modifications. b. Apical (or luminal) surfaces can be defined by: 1. Microvilli – Short, cytoplasmic processes extending from cell surfaces; non-motile 2. Stereocilia – Rather long microvili; non-motile; sometimes called “sterovili” now. 3. Cilia – Long, motile (or sometimes non-motile) cytoplasmic processes extending form surface; can be resolved by light microscopy. c. Basolateral surfaces can be defined by: 1. Basement membrane – We already talked about this (specialized structure connecting epithelium to underlying tissue) 2. Cell-to-cell and cell-to-matrix junctions – Anchor cell to another cell or the extracellular matrix CLASS: 11:00 – 12:00 Scribe: Adam Baird DATE: November 1, 2010 Proof: PROFESSOR: Cotlin HUMAN TISSUES II Page 5 of 7 3. Basal infoldings- infoldings at the basal surface to increase surface area; mitochondria concentration high. XXXI. MICROVILLI [S21] a. The main purpose of microvilli is to increase surface area. b. Microvilli characteristics: 1. Finger-like projections of plasma membrane 2. Localized to apical surface of epithelial cells 3. High-capacity absorption 4. Brush border (very prominent layer in the small intestine, for example) 5. Will have many receptors with carbohydrates attached 6. Contain microfilaments (actin and accessory proteins) c. As the surface area increases, so does absorbing and digesting rates XXXII. STRUCTURE OF MICROVILLI [S22] a. Actin is the core of microvilli b. Actin, in conjunction with myosin and a little accessory protein, produces the contractile ability. c. Structure of microvilli can be forced open to make more room, more surface exposure, and greater accessibility (like if your fingers were microvilli and they were spread apart upon contraction, for example). XXXIII. MICROVILLI WITH GLYCOCALYX [S23] a. Notice the long strands of carbohydrates that are added on through the secretory pathway (the glycocalyx sugar coat). Collectively, this is called the brush border. XXXIV. STEREOCILIA [S24] a. Stereocilia are just like microvilli, except they are longer b. Stereocilia have cross-bridges (sometimes) c. Stereocilia can be seen in the epididymis and in the ear canal (for increased surface area and absorption of fluid) d. Stereocilia are non-motile. They move according to the environment. e. Sterocilia have a core made of actin. XXXV. STEREOCILIA IN THE EPIDIDYMIS [S25] a. Stereocilia in the epididymis. This is a pseudostratified layer. b. Notice the long and stringy appearance. Notice that it’s not uniform. c. Microvilli, however, are short and uniform in size. Cilia are the same as microvilli, just a little longer. XXXVI. CILIA [S26] a. Cilia are motile elements. b. Cilia have microtubules in them (not actin) c. Cilia also increase surface area d. The primary purpose of cilia: to move fluid and mucous over the surface 1. Cilia are seen in the pulmonary tract. (The trachea is lined with highly ciliated pseduostratified epithelium.) 2. Cilia are very organized and beat in an upward fashion to keep debris out of the lower respiratory tract 3. In the ovaduct though, cilia move toward the ovary and uterus e. Primary cilia: 1. Recall that all cells are polarized (in some fashion) 2. Primary cilia are very rudimentary and have no motility 3. Primary cilia are very important during development though a. Primary cilia help a cell orient itself in its developing environment; it’s like a sensory organelle that feels the environment around it and responds accordingly. XXXVII. STRUCTURE OF CILIA [S27] a. Cilia have a core of microtubules (tubulin dimmers that polymerize into long arrays; have to be organized from scaffolding). Notice the basal bodies that are the scaffold for extending. b. Dyneins (which are molecular motor that can walk along microtubules) help organize. For example: If 9 people made a circle and arranged themselves together shoulder-to-shoulder. If one person in the circle pull back, the person in front of them will also move back, leading to a wave around the circle. This is how cilia move – and they can do so (in this coordinated fashion) – due to the connection of dynein arms. c. The coordination of cilia beating in the same direction at the same time can be seen especially in the respiratory tract. d. How all of the cells coordinate the cilia to beat (how it occurs) is unknown though. XXXVIII. BASAL BODY AND MICROTUBULES [S28] a. Left Picture: Here is a nice picture of microtubules. This is called the “9+2 arrangement”. CLASS: 11:00 – 12:00 Scribe: Adam Baird DATE: November 1, 2010 Proof: PROFESSOR: Cotlin HUMAN TISSUES II Page 6 of 7 b. Right Picture: Notice the basal bodies. Notice the extension of microtubules. XXXIX. BASAL AND LATERAL FOLDS [S29] a. The structures we have mentioned so far are found only in the apical region. Recall that at the apical region, there are projections that increase surface area. b. The basolateral region includes the basement membrane, as well as basal folds and lateral folds. At the basolateral region, there are infolding regions that increase surface area, which is important when transferring a lot of material at once. c. So there are projections at the top (apical) and infoldings at the bottom (basolateral). Both regions have characteristics to increase surface area. XL. VARIOUS JUNCTIONS OF EPITHELIAL CELLS [S30] a. Junctions can be categorized based on their structural role (or if they communicate, etc.) 1. Occluding Junctions 2. Anchoring Junctions (Cell-Cell, Cell-Matrix) 3. Chanel Forming “Communicating” Junctions (Gap Junctions) b. Tight junctions define the apical and basolateral region; their tightness keeps anything from leaking through or across the junction. c. Adherens – Connection sites to actin network; underlies plasma membrane d. Desmosomes – Connection sites to intermediate filaments; cell-cell junction; have extracellular proteins e. Hemidesmosomes – Half of a desmosome; cell-matrix junction (basement membrane) f. Gap junctions – channels that form between two cells; allow fluid to flow from one cell to another cell. XLI. JUNCTIONAL COMPLEXES [S31] a. Previously mentioned. Types of junctions: 1. Occluding Junctions – Occlude things from one side to another side. 2. Anchoring Junctions 3. Channel Forming “Communicating” Junctions XLII. JUNCTIONAL COMPLEXES [S32] a. This is what junctions look like. b. Tight junctions run all the way around the cell, forming a “band” around the cell (due to the tight juntions of other surrounding cells). This makes the cells look sewn together. c. Actin networks usually form bands around the cell too. d. Desmosomes (also known as macular adherens) are like nails, periodic attachment sites for intermediate filaments. e. Gap junctions are found in basal regions. They are broad and usually found in groups. XLIII. EM OF JUNCTIONAL COMPLEXES [S33] a. EM of tight junction b. Notice: It looks like two cells are sealed together. c. Between the other junctions, notice the intracellular space. XLIV. TRANSMEMBRANE LINKAGES BETWEEN CELLS AND EXTRACELLULAR STRUCTURES [S34] a. Intracellular Linkages 1. Desmosomes are attachments to intermediate filaments 2. Zonula adherens are attachments for actin filaments b. Extracellular Linkages 1. Many anchoring transmembrane proteins a. Tight junctions have claudins proteins. b. Adheren junctions have cadherin proteins 2. Example: Integrins that are cell-surface transmembrane protein, anchoring to the matrix XLV. TIGHT JUNCTIONS [S35] a. Tight junctions have occludin and claudin proteins b. Very tight, impermeable barrier (junction) c. Defines apical domain XLVI. ROLE OF TIGHT JUNCTIONS IN TRANSCELLULAR TRANSPORT [S36] a. Note glucose movement. It’s necessary to move glucose from one side of the junction to the other side of the junction, but if you open the junction, everything else will flow through. b. Example (of tight junctions that are “leaky”): Gall bladder, which concentrates bile. It’s necessary to take in lots of water, so the junctions become leaky. It’s necessary to the bile to be concentrated too, so in a regulated fashion, the junctions tighten up. The balance between leaky/tight keeps the water and bile concentration levels at the right balance. XLVII. TIGHT JUNCTIONS [S37] a. Notice the paracellular pathway CLASS: 11:00 – 12:00 Scribe: Adam Baird DATE: November 1, 2010 Proof: PROFESSOR: Cotlin HUMAN TISSUES II Page 7 of 7 b. When tight junctions become leaky, molecules move between the cells (paracellular pathway) XLVIII. ZONULA ADHERENS [S38] a. Here is what zonula adherins look like in a polarized cell. b. Notice the banding pattern around the cell. XLIX. ZONULA ADHERENS [S39] a. Notice the cadherins keeping the cells connected together. Also notice there is still some space between the cells. L. DESMOSOMES [S40] a. Desmosomes are the attachments for intermediate filaments b. Proteins in the middle keep the cells together LI. DESMOSOMES [S41] a. We’ll flip through the rest of these slides relatively quickly. b. Notice the fibers coming in together (like nails) LII. HEMIDESMOSOMES [S42] a. This is the structure where the cell is attached to an underlying matrix. In this case, it’s attached to the basement membrane. b. Notice that there are many proteins to keep everything together. LIII. HEMIDESMOSOMES [S43] a. Notice the basement membrane. b. The blue arrow is pointing to the hemidesmosomes LIV. STRUCTURE OF GAP JUNCTIONS [S44] a. “Little pore formings” b. Gap junctions physically line up cell-cell c. Gap junctions can “open and close”, which is critical in muscle tissue (because it allows for molecules and ions to be exchanges, propagating contractions). LV. GAP JUNCTION ORGANIZATION [S45] a. Seen in “little patches” b. Connexins are seen on the right (individual molecules) LVI. GAP JUNCTIONS [S46] LVII. NO TITLE [S47] a. Picture showing all of the junctions grouped together. [End 45:33 mins]