clostridium difficile diarrhoea - West Hertfordshire Hospitals NHS Trust
advertisement
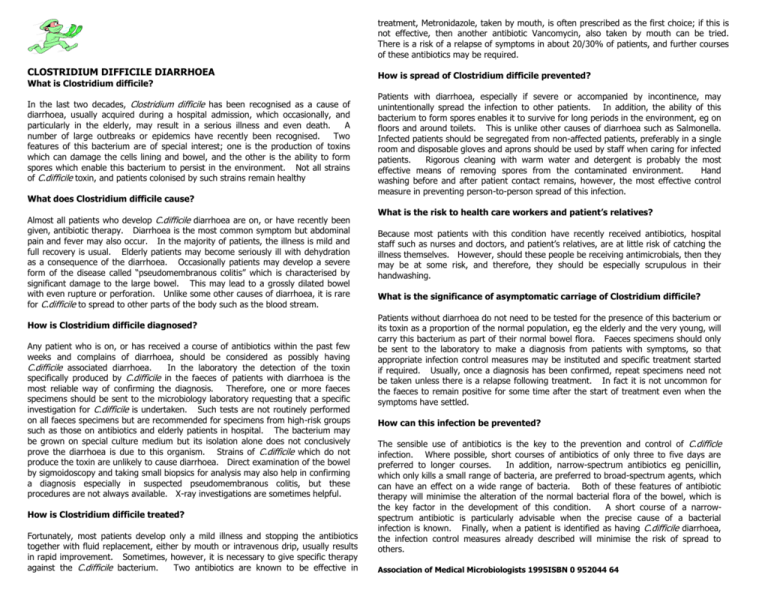
treatment, Metronidazole, taken by mouth, is often prescribed as the first choice; if this is not effective, then another antibiotic Vancomycin, also taken by mouth can be tried. There is a risk of a relapse of symptoms in about 20/30% of patients, and further courses of these antibiotics may be required. CLOSTRIDIUM DIFFICILE DIARRHOEA What is Clostridium difficile? In the last two decades, Clostridium difficile has been recognised as a cause of diarrhoea, usually acquired during a hospital admission, which occasionally, and particularly in the elderly, may result in a serious illness and even death. A number of large outbreaks or epidemics have recently been recognised. Two features of this bacterium are of special interest; one is the production of toxins which can damage the cells lining and bowel, and the other is the ability to form spores which enable this bacterium to persist in the environment. Not all strains of C.difficile toxin, and patients colonised by such strains remain healthy What does Clostridium difficile cause? Almost all patients who develop C.difficile diarrhoea are on, or have recently been given, antibiotic therapy. Diarrhoea is the most common symptom but abdominal pain and fever may also occur. In the majority of patients, the illness is mild and full recovery is usual. Elderly patients may become seriously ill with dehydration as a consequence of the diarrhoea. Occasionally patients may develop a severe form of the disease called “pseudomembranous colitis” which is characterised by significant damage to the large bowel. This may lead to a grossly dilated bowel with even rupture or perforation. Unlike some other causes of diarrhoea, it is rare for C.difficile to spread to other parts of the body such as the blood stream. How is Clostridium difficile diagnosed? Any patient who is on, or has received a course of antibiotics within the past few weeks and complains of diarrhoea, should be considered as possibly having C.difficile associated diarrhoea. In the laboratory the detection of the toxin specifically produced by C.difficile in the faeces of patients with diarrhoea is the most reliable way of confirming the diagnosis. Therefore, one or more faeces specimens should be sent to the microbiology laboratory requesting that a specific investigation for C.difficile is undertaken. Such tests are not routinely performed on all faeces specimens but are recommended for specimens from high-risk groups such as those on antibiotics and elderly patients in hospital. The bacterium may be grown on special culture medium but its isolation alone does not conclusively prove the diarrhoea is due to this organism. Strains of C.difficile which do not produce the toxin are unlikely to cause diarrhoea. Direct examination of the bowel by sigmoidoscopy and taking small biopsics for analysis may also help in confirming a diagnosis especially in suspected pseudomembranous colitis, but these procedures are not always available. X-ray investigations are sometimes helpful. How is Clostridium difficile treated? Fortunately, most patients develop only a mild illness and stopping the antibiotics together with fluid replacement, either by mouth or intravenous drip, usually results in rapid improvement. Sometimes, however, it is necessary to give specific therapy against the C.difficile bacterium. Two antibiotics are known to be effective in How is spread of Clostridium difficile prevented? Patients with diarrhoea, especially if severe or accompanied by incontinence, may unintentionally spread the infection to other patients. In addition, the ability of this bacterium to form spores enables it to survive for long periods in the environment, eg on floors and around toilets. This is unlike other causes of diarrhoea such as Salmonella. Infected patients should be segregated from non-affected patients, preferably in a single room and disposable gloves and aprons should be used by staff when caring for infected patients. Rigorous cleaning with warm water and detergent is probably the most effective means of removing spores from the contaminated environment. Hand washing before and after patient contact remains, however, the most effective control measure in preventing person-to-person spread of this infection. What is the risk to health care workers and patient’s relatives? Because most patients with this condition have recently received antibiotics, hospital staff such as nurses and doctors, and patient’s relatives, are at little risk of catching the illness themselves. However, should these people be receiving antimicrobials, then they may be at some risk, and therefore, they should be especially scrupulous in their handwashing. What is the significance of asymptomatic carriage of Clostridium difficile? Patients without diarrhoea do not need to be tested for the presence of this bacterium or its toxin as a proportion of the normal population, eg the elderly and the very young, will carry this bacterium as part of their normal bowel flora. Faeces specimens should only be sent to the laboratory to make a diagnosis from patients with symptoms, so that appropriate infection control measures may be instituted and specific treatment started if required. Usually, once a diagnosis has been confirmed, repeat specimens need not be taken unless there is a relapse following treatment. In fact it is not uncommon for the faeces to remain positive for some time after the start of treatment even when the symptoms have settled. How can this infection be prevented? The sensible use of antibiotics is the key to the prevention and control of C.difficle infection. Where possible, short courses of antibiotics of only three to five days are preferred to longer courses. In addition, narrow-spectrum antibiotics eg penicillin, which only kills a small range of bacteria, are preferred to broad-spectrum agents, which can have an effect on a wide range of bacteria. Both of these features of antibiotic therapy will minimise the alteration of the normal bacterial flora of the bowel, which is the key factor in the development of this condition. A short course of a narrowspectrum antibiotic is particularly advisable when the precise cause of a bacterial infection is known. Finally, when a patient is identified as having C.difficile diarrhoea, the infection control measures already described will minimise the risk of spread to others. Association of Medical Microbiologists 1995ISBN 0 952044 64