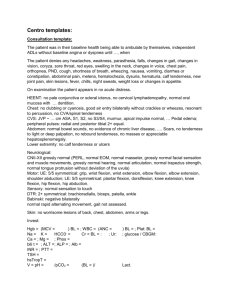
CASE Ⅰ (complete history)
advertisement
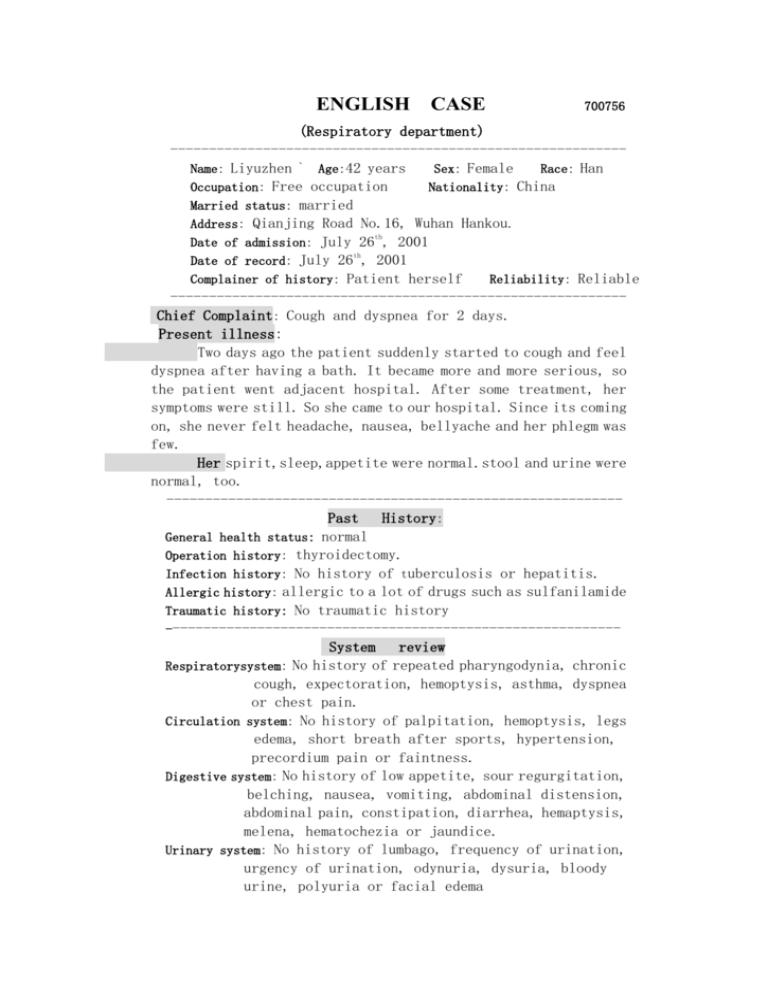
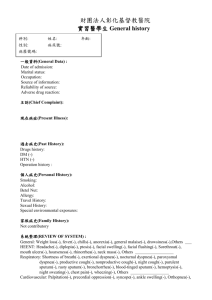
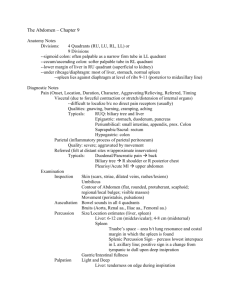
ENGLISH CASE 700756 (Respiratory department) ----------------------------------------------------------Name: Liyuzhen ` Age:42 years Sex: Female Race: Han Occupation: Free occupation Nationality: China Married status: married Address: Qianjing Road No.16, Wuhan Hankou. th Date of admission: July 26 , 2001 th Date of record: July 26 , 2001 Complainer of history: Patient herself Reliability: Reliable ----------------------------------------------------------Chief Complaint: Cough and dyspnea for 2 days. Present illness: Two days ago the patient suddenly started to cough and feel dyspnea after having a bath. It became more and more serious, so the patient went adjacent hospital. After some treatment, her symptoms were still. So she came to our hospital. Since its coming on, she never felt headache, nausea, bellyache and her phlegm was few. Her spirit,sleep,appetite were normal.stool and urine were normal, too. ----------------------------------------------------------Past History: General health status: normal Operation history: thyroidectomy. Infection history: No history of tuberculosis or hepatitis. Allergic history: allergic to a lot of drugs such as sulfanilamide Traumatic history: No traumatic history ----------------------------------------------------------System review Respiratorysystem: No history of repeated pharyngodynia, chronic cough, expectoration, hemoptysis, asthma, dyspnea or chest pain. Circulation system: No history of palpitation, hemoptysis, legs edema, short breath after sports, hypertension, precordium pain or faintness. Digestive system: No history of low appetite, sour regurgitation, belching, nausea, vomiting, abdominal distension, abdominal pain, constipation, diarrhea, hemaptysis, melena, hematochezia or jaundice. Urinary system: No history of lumbago, frequency of urination, urgency of urination, odynuria, dysuria, bloody urine, polyuria or facial edema Hematopoietic system: No history of acratia, dizziness, gingival bleeding, nasal bleeding, subcutaneous bleeding or ostealgia. Endocrine system: No history of appetite change, sweating, chilly excessive thirst, polyuria, hands tremor, character alternation, obesity, emaciation, hair change, pigmentation or amenorrhea. Kinetic system: No history of wandering arthritis, joint pain, red swelling of joint, joint deformity, muscle pain or myophagism. Neural system: No history of dizziness ,headache, vertigo, insomnia, disturbance of consciousness, tremor, convulsion, paralysis or abnormal sensation. ---------------------------------------------------------Personal History: She was born in Hubei.She never smokes and Drinks.No exposure history to toxic substances, and infected water.Her menstruation was normal. LMP:23/7,2001 ----------------------------------------------------------Family History: Her parents are living and well. No congenital disease in her family. ----------------------------------------------------------- Physical Examination Vital signs: T 36.6`C , P 80/min, R 22/min, BP120/80mmHg. General inspection: The patient is a well developed, well nou- rished adult female apparently in no acute distress, pleasant and cooperative. Skin: Normally free of eruption or unusual pigmentation. Lymphnodes: There are no swelling of lymphnodes. Head: Normal skull. No baldness, noscars. Eyes: No ptosis. Extraocular normal. Conjuctiva normal. The Pupils are round, regular, and react to light and acCommodation. Ears: Externally normal. Canals clear. The drums normal. Nose: No abnormalities noted. Mouth and throat: lips red, tongue red. Alveolar ridges normal. Tonsils atrophil and uninfected. Neck: No adenopathy. Thyroid palpable,but not enlarged. No Abnormal pulsations. Trachea in middle. Chest and lung: Normal contour. Breast normal. Expansion equal. Fremitus normal. No unusual areas of dullness. Diaphr- agmatic position and excursion normal. No abnormal breath sound. No moist rales heard. No audible pleural fricion. There are lots of rhonchi rales and whoop can be heard th Heart: P.M.I 0.5cm to left of midolavicular line in 5 interSpace. Forceful apex beat.No thrills.No pathologic heart murmur. Heart beat 80 and rhythm is normal. Abdomen: Flat abdomen. Good muscle tone. No distension. No visible peristalsis. No rigidity. No mass palpable. Tenderness (-), rebound tenderness (-).Liver and spleen are not palpable. Shifting dullness (-). Bowl sounds normal. Systolic blowing murmur can be heard at the right side of the navel. Extremities: No joint disease. Muscle strength normal. No abnormal motion. Thumb sign(+). Wrist sign(+). Neural system: Knee jerk (-). Achilles jerk (-). Babinski sign (-). Oppenheim sign (-). Chaddock sign (-). Conda sign (-). Hoffmann sign (-). Neck tetany (-) Kernig sign (-). Brudzinski sign (-). Genitourinary system: Normal. Rectum: No tenderness -------------------------------------------------------------------- Out-patient department data: No ----------------------------------------------------------- History summary 1). Li Yuzhen, female, 42y. 2). Cough and dyspnea for 2 days 3). PE: T 36.6`C, P 80/min, R 22/min, BP120/80mmHg.superficial nodes were not palpable. Normal vision. Upper palate haunch-uped. HR: 80bpm, rhythm is normal. There are lots of rhonchi rales and whoop can be heard .Flat abdomen, Tenderness (-),rebound tenderness (-).Liver and spleen are not palpable.Shifting dullness (-). Bowl sounds normal.. 4).Outpatient data: see above. ----------------------------------------------------------- Impression: Bronchial asthma Signature:He Lin 95-10033