ANOTHER POWERPOINT FILE (Clinical examination II)
advertisement

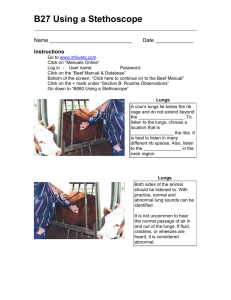
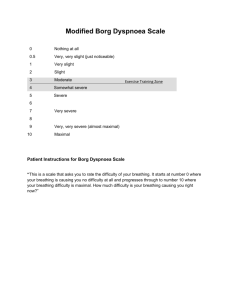
Clinical Diagnosis of Ruminant Animals Diseases Part II التشخيص االكلينيكي ألمراض المجترات الجزء الثانى By Prof. Dr. Ibrahim H.A. Abd El-Rahim Professor of Infectious Diseases, Animal Medicine Department, Faculty of Veterinary Medicine, Assiut University E-mail: vetrahim@hotmail.com Examination of the respiratory system فحص الجهاز التنفسى First observe the breathing from a distance, while listening for abnormal sounds associated with breathing. Next examine each segment of the respiratory tract separately in the following order: breath, muzzle, nose and nasal sinuses, pharynx and larynx, trachea and lungs. At the same time inspect the chest wall for pathological changes. Respiratory movements حركة التنفس - Breathing is best observed from behind and to one side of the animal, without disturbing the animal, by watching movements of the costal arch and flank. - Rate, intensity, type and rhythm should be considered. Intensity is normally moderately pronounced in cattle, so respiratory movements of chest and abdominal wall are clearly visible. - In normal breathing rhythm the ratio of duration of inspiration to duration of expiration is about 1.0 to 1.2; there is a short pause in breathing at the end of expiration. - Eupnoea: Breathing of normal frequency, intensity, type and rhythm is called eupnoea. 1 Dyspnea ضيق التنفس Difficulty in breathing with changes in normal characteristics (normal frequency, intensity, type and rhythm) accompanying respiratory disease. 1. Inspiratory dyspnoea ضيق التنفس أثناء الشهيق - It is characterized by more frequent breathing and by stronger and longer inspiration due to narrowing of the upper air passages and those forms of bronchopneumonia unaccompanied by pulmonary emphysema. - Signs of severe dyspnoea are extension of the head and neck, nostril dilation during inspiration, spreading of the scapulas, slack or sunken flanks and sagging belly; sometimes sounds of stenosis are audible at a distance from the animal. 2. Expiratory dyspnoea ضيق التنفس أثناء الزفير - If breathing out is impeded, expiratory dyspnoea occurs characterized by mainly abdominal breathing and stronger and longer breathing out than breathing in. - The forced breathing out distends the flank and anal region, and it is often accompanied by long groans. Other symptoms are breathing with the mouth open and the tongue protruded. 3. Mixed dyspnoea ضيق التنفس أثناء الشهيق والزفير - It occurs with chronic respiratory disease, and here there is difficulty in breathing in and out. - It occurs during primary pulmonary emphysema. Externally audible sounds associated with breathing أصوات غير طبيعية مسموعه ومصاحبة لعملية التنفس These have to be differentiated according to origin & cause, as follows: o Snorting - a sneezing sound produced by a brief, powerful expiration through the nose (occurs during irritation of the nasal mucosa). o Stenosis sounds - produced by constriction, in the upper respiratory tract. Nasal stenosis sound (snuffling). Pharyngeal stenosis sound (snoring). Laryngeal stenosis produces roaring in the throat (calf diphtheria). 2 o Coughing – Due to inflammation of the respiratory mucous membrane. The type of cough may provide a clue to the site of the lesion: it is relatively dry & powerful in diseases of the upper respiratory tract, and more moist & feeble during the more deep-seated bronchopneumonia, pulmonary emphysema or pleurisy. Nasal discharge االفزات االنفية - The colour is normally water-clear and serous, otherwise whitish and cloudy; red to rust-brown if due to haemorrhage. - The consistency is normally watery, otherwise mucoid or flocculated in catarrhal or purulent inflammation; lumpy or crumbly in necrotic inflammation. - The odour is normally odourless (foul in deep-seated tissue damage). - Any sputum ejected from the mouth or nose is always pathological, and should be examined in the same way as nasal discharge. Lungs and pleura الرئة والغشاء البلورى The lungs and pleura are examined by acoustic and sensitivity percussion, together with auscultation of the lung field. The lung field - Dorsal margin is the lateral edge of the trunk musculature. - Cranial border is formed by the posterior edge of the triceps muscle. Caudal border extends from its dorsal extremity at the 11th intercostal space, across the middle of the 9th rib to about two fingerbreadths above the elbow joint. - On the right side the posterior border extends 1 or 2 fingerbreadths further back (to about the 12th rib) compared with the left side. Acoustic percussion الطرق السمعى - The percussion hammer is held loosely between the thumb and index finger, and the pleximeter is pressed against the chest. - The first stage is horizontal percussion to establish the course of the caudal lung limits. This is best performed on the right side. 3 - The next stage is vertical percussion from above to below, commencing at the cranial edge of the thoracic lung field and extending backwards at each intercostal space. This establishes any change in the normal lung resonance. Table 1. Summary of types of sound heard during percussion of the lung field SOUND QUALITY CHARACTERISTICS OF TYPES OF PERCUSION RESONANCE Good resonance Normal lung sound without booming A fairly loud, It is heard over areas of emphysema and pneumothorax. subtympanic sound Circumscribed They are produced by air-free pneumonic lesions, areas of dullness abscesses, tumours, enlarged lymph nodes, prolapse of digesta-filled portions of the digestive system through the diaphragm, or pronounced thickening of the pleura. Auscultation السماع بإستخدام السماعه أصوات التنفس الطبيعى Normal respiratorz sounds Vesicular breathing is heard only in the caudodorsal third of the thoracic field. it resembles the start of the syllable “V”, whispered. In the rest of the field a mixed breathing sound occurs in which vesicular breathing is mixed with the dominant bronchial breathing, it resembles a prolonged syllable “ch”. أصوات التنفس الغير الطبيعى Abnormal respiratory sounds Areas of lung tissue that contain no air (pneumonic lesions, pulmonary oedema, large abscesses, neoplasms, Echinococcus cysts) are completely silent. Vesicular breathing sounds are enhanced during the deeper inspirations of dyspnoea and over emphysematous areas. Bronchial breathing is louder than normal in the various forms of stenosis of the upper respiratory tract and during laryngitis, tracheitis and bronchitis. 4 Pathological variations in respiratory sounds: أصوات التنفس فى الحاالت المرضية Rustling (crepitation), due to small-bubbled foam, occurs during pulmonary emphysema (like the light rubbing of fine sandpaper). Moist rales are heard when the bronchi contain watery secretion or exudation (pulmonary oedema, catarrhal bronchopneumonia, or aspiration pneumonia). It resembles simmering, the whipping up of froth . Dry rales are heard when the exudates thicken up to form thick mucus, resulting in elongated projections into the bronchial lumen and vibrate in air currents, producing dry rales. Friction sounds - Movement of parts of the pleura, thickened by inflammation, against each other produces friction sounds. Sounds may be heard during auscultation, and it is important not to confuse them with normal and abnormal breathing sounds: أصوات قد تتداخل مع أصوات التنفس Muscular tremor (which shakes the chest piece of the phonendoscope). Hair rustling (press the phonendoscope more firmly). Tooth grinding, swallowing, eructation and cud regurgitation. Grinding chewing (rumination), contractions of the forestomachs and painful moaning. Unilateral absence of breathing sounds may be due to pneumothorax. Examination of the digestive system فحص الجهاز الهضمى The general examination will have provided information on: Appetite and feed intake, الشهيه وتناول الغذاء Thirst and fluid intake, العطش وشرب الماء Rumination, االجترار Eructation (or development of bloat), التكريع Any regurgitation of feed or vomiting of stomach contents; الترجيع - Also the type and nature of defecation. التبرز - 5 تناول الغذاء وشرب الماء Intake of feed and water Appetite الشهيه Classification of inappetence according to the cause: o True or primary inappetence: It means absent or diminished appetite (due to poor feed quality or a disease of the GIT). o Secondary or symptomatic inappetence: It means poor appetite (due to diseases of organs unrelated to the digestive system, or a wide range of systemic diseases. The return of appetite is always a favourable sign for prognosis. The following types of appetite disorders are distinguished: - Diminished appetite, when the animal eats hesitantly or more slowly than its neighbours, or consumes only part of its ration, as during mild illnesses. - Complete inappetence (anorexia) occurs during persistent, severe diseases. - Abnormal appetite. - An appetite confined to certain feeds and abnormal appetite (licking disease, allotriophagia, pica) for substances other than feeds point to a metabolic or deficiency disorder. Rumination االجترار o Commencement of rumination, usually 1/2 to 1 1/2 hours after feeding. o Number and duration of rumination cycles, in a day there may be 4 to 24 periods of rumination each lasting 10 to 60 minutes, so that up to 7 hours may be spent ruminating every day. o Number of ruminated boluses: 360 to 790 a day. o Size of each ruminated bolus: about 80 to 120 g. A bolus can be recovered from the oral cavity by a quick thrust of the hand immediately after its return. o Number of jaw movements and chewing time per bolus: 40-70 chews within 45-60 seconds, depending on composition of the feed. 6 Disorders of rumination occur as a result of اسباب إضطرابات االجترار Pathological changes in the mouth, oesophagus or forestomachs (foreign body trauma, functional gastric stenosis), or May accompany severe diseases affecting general health and located elsewhere in the body; consequently primary and secondary (symptomatic) disorders can be distinguished. Features to be watched for are: - Delayed onset of rumination after feeding; Too few or too brief periods of rumination; Too few chews per bolus; Too short or too long duration of chewing per bolus; Superficial, intermittent or absent rumination; More rarely, faulty chewing or loss of the cud; Abnormally frequent or prolonged rumination, accompanied by salivation, smacking the lips or grinding the teeth (in brain diseases, lead poisoning or the nervous form of acetonaemia). Rumen فحص الكرش The rumen is examined by: o Observation of the left flank, o Palpation (through the abdominal wall and through the rectum), o Auscultation, o Percussion, and o By collecting and testing a sample of rumen fluid. o Particular cases may require laparoscopy, rumenography, telemetric recording or (in calves) radiography. o Sometimes a diagnosis can be established only after exploratory rumenotomy. Observation المالحظة Observation of the hollow of the left flank provides information on: - The degree of fullness of the rumen (hollow flank - not full; tensed - normal; bulging - overfull), and - The intensity of contractions, which are clearly visible only in cattle having a thin abdominal wall. 7 Palpation التحسس - Abnormal filling with gas or foamy feed mass (bloat) produces taut, elastic tension with a more or less pronounced bulge in the dorsal part of the left flank. - Overloading of the rumen with solid food produces a firmer, barely yielding consistency. - In functional stenosis of the stomach the rumen is dilated, tone is abolished and it is usually overloaded with fluid or foamy food masses responding to punching with fluctuation and splashing. - During advanced rumen acidosis (lactic acid) the contents of the forestomachs are very fluid. Auscultation إستخدام السماعه Attention is paid to the nature, strength and frequency of rumen sounds, which in health cattle take the form of a periodic rustling sound, increasing, to a crescendo then falling away. The normal rate of rumen sounds is 2 or 3 strong contractions/ 2 minutes. Hypermottllty — increase in the rate of rumen movements — occurs during vagus stimulation. Hypomotility — decrease in the rate of rumen movements — occurs when a ration poor in fibrous structure is fed, during forestomach disorders (indigestion). Atony — stop of rumen movements — occurs during severe forestomach disorders (traumatic reticuloperitonitis, rumen acidosis, etc.). Acoustic percussion of the rumen الطرق السمعى للكرش Subtympanic sound: It is the normal rumen sound in the dorsal part of the left abdominal wall. Damped sound: Ventral to this there is a relative damping of the percussion sound. This zone becomes completely damped when the rumen is overloaded. Drum-like boom: In bloat (tympany). Tympanic sound: In left-sided abomasal displacement. Box sound: In fresh cases of traumatic reticuloperitonitis. Pain percussion: in rumenitis and large abscesses of the rumen. 8 Tests for foreign bodies إختبارات للكشف وجود االجسام الغريبة o Back grip: A fold of skin over the withers is pulled up so that the animal's back is suddenly pressed down. o Pole test: A pole 1-1 1/2 metres long is placed under the animal and held at each end by two assistants. The pole is pulled upwards slowly, and then allowed to fall suddenly. o Pain percussion: It is carried out with a fairly heavy hammer having a rubber head applied with short strokes. o Palpation for tenderness: A strong pressure is applied with the fist or the palm of the hand to the reticular projection field. o Leading the animal up and down a steep slope Increased sensitivity is manifested by signs of tenderness (a sighing grunt or brief holding of the breath). Liver الكبد Examination of the bovine liver commences with: Inspection of visible mucous membranes. Palpation and percussion of the liver region. Dorsally behind the right costal arch is the site for palpation of the liver by forceful pressure on the abdominal wall by the finger tips, just behind the last rib Examination of urine and faeces. Liver function test. Rectal exploration االستكشاف عن طريق المستقيم o Rectal examination of the intestines includes the rectum itself, (e.g. thickness and tension of the wall). o Organs that can be felt through the rectum are: - The caudal loops of intestine, Internal genital organs and parts of the peritoneum, rumen, Left kidney (sometimes the caudal pole of the right kidney), Aortic bifurcation, Bony pelvis, Sacrum, Internal ilio-femoral lymph nodes, Urinary bladder o Pregnancy disgnosis 9 Conditions can be diagnosed through rectal examination: حاالت يمكن تشخيصها بواسطة االستكشاف عن طريق المستقيم 1. Acute enteritis: mesenteric lymph nodes slightly enlarged; 2. Chronic enteritis: mesenteric lymph nodes enlarged & firm (paratuberculosis or leukosis), or hard (tuberculous calcification); thickened wall (paratuberculosis. 3. Intussusception (jejunal invagination). 4. Volvulus and strangulation of the small intestine. 5. Intestinal obstruction. 6. Torsion of intestinal mesentery. 7. Dilation and torsion of the caecum. 8. Intestinal rupture with generalized peritonitis. 9. Necrosis of adipose tissue. 10.Dilation and overloading of the rumen 11.Displacement of the abomasum to the right, with or without torsion 12.Excessive placental fluid. 13.Simple dilation of the abomasum. 14.Displacement of the abomasum to the left. 15.Accumulation of purulent exudate within the cavity of the omental bursa. 16.Kidney disease. Examination of faeces فحص البراز - Faeces are inspected, felt and smelt for the characteristics such as amount, colour, and consistency. - Examination for parasites, bacteria, viruses or poisons may be indicated, particularly in diarrhoea, depending on concomitant circumstances (single animal affected or whole herd; type of feeding and management; environmental factors). Abnormal contents of faecal matter محتويات غير طبيعيه بالبراز Abnormal contents are detected by inspection and feeling, as follows: - In very severe enteritis, faeces may be replaced by fluid. Greyish-white mucus (sign of intestinal obstruction). Fibrin (during severe catarrhal enteritis) Blood from posterior segments of intestine appears bright red in the form of streaks on the surface of the faecal matter. 10 - Blood from anterior portions (chocolate brown or black (melaena), and well-mixed with faecal matter. - Gas bubbles (in diarrhoeic excrement, and paratuberculosis). - Macroscopically visible parasites (tapeworm segments, roundworms) may be included here. Examination of the udder فحص الضرع For examination of the udder: - Case history (husbandry conditions, milking techniques, milking hygiene, treatment) - Inspection, - Palpation, - Inspection of the udder secretion, and - If necessary biochemical and microbiological examination of milk samples. Inspection )المالحظة (المشاهدة والتوقع - Asymmetry of the udder is usually due to atrophy (or more rarely hypertrophy) of one quarter. - Enlargement of the whole udder or one quarter may conceal rupture of the rectus abdominis muscle, a flank rupture extending as far as the udder, abscess or haematoma. Palpation التحسس This includes: Teat canal, Teat cistern, Wall of the teat, Udder cistern, Udder skin and Glandular tissue of each quarter. - Swelled, hot, painful palpation (acute mastitis) Hard indurated (fibrosed) udder tissue (chronic mastitis) Physiological oedema occurs shortly before calving A pathological form of oedema leading to induration of the skin and subcutaneous tissue “hard udder”. - Each quarter is felt in the milked-out state for consistency (granules, nodules, diffuse hardening, acute swelling, consistency). - Mastitis of infectious origin leads to enlargement of the mammary lymph nodes. 11