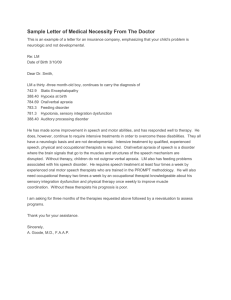
CHRONIC BENIGN INTRACTABLE LOW BACK
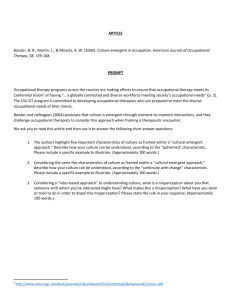
advertisement

CHRONIC BENIGN INTRACTABLE LOW BACK PAIN (CBILBP): How do occupational therapists working in primary care facilitate patients with this condition? CONTENTS Section Page Numbers Introduction Definitions for study 1 Background 1 Aims of study 3 Literature review 4 Methodology 13 Ethics 16 Design 18 Pilot study 18 Method Sample 19 Data collection 20 Data analysis 23 Results Survey 25 Telephone interviews 29 Trustworthiness 38 Discussion Results 41 Literature 48 1 Methodology 48 Design 49 Sample 50 Data Collection 50 Data Analysis 54 Limitations of the Study 54 Conclusions 55 Recommendations 56 Acknowledgements 58 References 59 Appendices 72 2 Abstract The prevalence of chronic low back pain is increasing and is apparent in the number of patients who continue to be referred to a tertiary pain management service. Ten years ago the Clinical Standards Advisory Group (CSAG) recommended a biopsychosocial assessment of all patients with acute low back pain to identify the potential risk factors for future chronicity and disability. With no concrete evidence to refer to, this study investigated the experiences of occupational therapists in primary care under the themes of assessment and intervention, knowledge of clinical standards, prevention of disability and multi-disciplinary working to measure the provision of occupational therapy with low back pain patients before referral to a tertiary programme. An exploratory design, employing a five step phenomenological approach was chosen to elaborate information drawn from a survey questionnaire. Telephone interviews were conducted with five occupational therapists working with chronic low back pain. The combined data revealed that there were no specific services for chronic low back pain and that the primary reason for referral to occupational therapy, whether in physical or mental health, was not the low back pain. Occupational therapists proved well equipped to deal with this client group in their caseloads due to their focus on occupational performance. Assessment and intervention were holistic and demonstrated a full understanding of the effects of low back pain and the ability to be active with the pain and this facilitated patient empowerment. Occupational therapists were not conversant with the CSAG recommendations but there was evidence to suggest that disability could be minimised. Occupational therapists were competent to work independently and in a multi-disciplinary approach with this client group. A lack of services for chronic low back pain was identified. 3 Introduction Definitions for study In areas of rural Wales hospital care is often in generic community facilities supported by General Practitioners. The establishment of local health boards in April 2003 has revised the politics of care again. Some patients have to travel long distances to access consultant physicians and surgeons, although there is some provision for outpatient appointments in local day hospitals. For the purpose of this analysis primary care is the period before patients are referred to one of the few residential pain management programmes in tertiary care. The primary care runs from the patient’s first appointment with the GP, complaining of low back pain, to the time when no further pathological intervention is considered useful. Chronic back pain is defined as pain that has persisted for longer than 3 months or past the time of healing (The College of Anaesthetists and the Pain Society, 2003) and ‘most commonly it is assumed that pain which persists for six months progressively leads to the chronic pain state, resulting in preoccupation with pain, depression, anxiety and disability’ (Wall, Melzack, 1999, p540). This leads to ‘occupational role disruption, psychosocial withdrawal, feelings of helplessness, loss of self esteem and physical incapacity’ (Strong, 1996, p6). Background The prevention of chronic low back pain is a major concern and efforts to contain the situation continue to emerge (NICE, 2003). Strong (1996) reports that the incidence of chronic pain is as high ás 82% of the community and at least 50% of these are related to chronic back pain, which is a major problem. GP consultations for low back pain have been estimated at 14 to 15 million per year in the United Kingdom (Clinical Standards Advisory Group (CSAG), 1994). Two prospective studies (Thomas et al., 1999, Croft et al., 1998) of patients who consulted the GP concluded that although 4 many patients discontinued to visit the GP about back symptoms after the first few months, they reported pain and increased disability at twelve months. Thomas et al., (1999) concluded that persistent low back pain was related to the patients’ premorbid state. Prevalence appears to be increasing due to cultural changes that have influenced attitudes and beliefs, contributing to psychological distress and long term disability (Buchbinder et al., 2001, Palmer et al., 2000, Waddell et al., 1999, Bandolier, 1995). Patients referred to a multi-disciplinary residential pain management centre present with acquired bio-psycho-social disabilities resulting from their inability to cope with chronic low back pain. Recent studies (Frost et al., 2001, Birkholz & Aylwin, 2000, van Tulder et al., 2000, Gibson, Strong 1998) focus quite emphatically on patients’ severe physical, emotional and social impairment, with limited reference to the input of specific health disciplines or occupational therapy intervention in particular. Personal experience advocates that occupational therapists are well qualified to facilitate improvement in some patients presenting with the effects of chronic low back pain and this is supported in the literature (Carruthers 1997, Strong, 1996, McCormack, 1990, Heck, 1987). Occupational therapists assess the impact of pain on occupational performance in all activities from self-care to family relationships, and work in partnership with patients to develop an optimal programme for living with the pain (Unruh et al., in Strong et al., 2002). They are holistic in approach, acknowledging emotional and social, as well as physical distress. However, it seems that occupational therapists have not recorded their personal experiences of assessment and treatment of patients with chronic low back pain, whether working individually, or in a multi-disciplinary team. It is unclear what, if any, occupational therapy is available in the pre-tertiary pain management programme period, or whether in fact it has any significant effect on patients, before admission or in preventing admission. It is not unusual to become insular in our own field of work, 5 losing sight of the approaches or treatments of fellow therapists working in other sections of medicine. As an Occupational Therapist working in a tertiary pain management programme, it is important to be informed about the pre-treatment history of the patients that are referred to, and treated at, the centre. A colleague investigated iatrogenic factors contributing to patients’ consequent disability with low back pain and discovered that poor information from clinicians, influencing patient beliefs about their condition, was a contributing factor (Hafner, 1999). The author considered that occupational therapists may be contributing to patient disability. This study sets out to: Record the experiences of occupational therapists working with chronic low back pain in primary care. Evaluate the knowledge of occupational therapists in primary care working with chronic low back pain patients. Assess the potential of occupational therapy in primary care preventing disability in patients with chronic low back pain. Discover whether occupational therapists in primary care can contribute to the management of chronic low back pain more effectively alone, or in a multidisciplinary team. Aims of Study Patients presenting at a chronic pain management programme with chronic benign, intractable low back pain are not always reliable witnesses about occupational therapy input in previous interventions. Many have been subjected to several treatments with no success or long lasting effect and they are frequently only able to identify the doctor or consultant involved. The report about other clinicians is often vague and identities confused. However it is apparent that patients are often more 6 disabled than they need to be due to poor or unhelpful advice (Hafner, 1999). It is possible that occupational therapists are equally responsible for contributing to this disability following the assessment and treatment they offer patients in primary care, or that in fact there is no occupational therapy input available or provided. This study asks: How does Occupational Therapy assessment and intervention, in primary care, affect patients with chronic, benign, intractable, low back pain? Answers to the following queries will help to verify a satisfactory conclusion. 1. What occupational therapy assessment and intervention is offered to patients with low back pain? 2. Are occupational therapists in primary care conversant with clinical guidelines and recommendations for low back pain? 3. Can occupational therapy in primary care prevent disability in low back pain patients? 4. Can occupational therapy assessment and intervention for low back pain stand alone in primary care or contribute more effectively within a multi-disciplinary approach? Literature Review Experiences and approaches of occupational therapists working with CBILBP in primary care A literature search on the Ovid Database (Medline, Cinahl, Amed, PsychINFO, Healthstar and Embase), Evidence Based Medicine, including Bandolier and the Cochran Library as well as a manual search revealed no articles about the occupational therapists’ experiences of working with chronic low back pain in primary 7 care. Several early articles (McCormack, 1988, Baptiste, 1988, Strong, 1987, Giles & Allen, 1986, Flower, 1981) commonly described the role of occupational therapists with chronic pain, not principally low back pain. Assessment and treatment focussed on improving performance and occupational roles through the use of graded activity, stress management and counselling. Towards the end of the decade chronic pain was being recognised as an illness rather than a disease (Waddell, 1987) and medical approaches to treatment were evolving. A more structured approach to pain management was observed in the 1990s. Carruthers (1997) identified an increasing interest of occupational therapists in pain management in the ten years leading up to her study. Strong (1996) had no doubt that occupational therapists are well equipped to enhance patients’ performance skills in the assessment (Gibson, Strong, 1998), and treatment of chronic low back pain and O’Hara (1996) advocated their role as facilitators and advisers to enable independent functioning. The authors favoured a cognitive behavioural approach to the overall management of chronic pain. Occupational therapists are certainly recognised as an integral member of the residential pain management multidisciplinary team (Birkholz, Aylwin, 2000), and are recommended by the Pain Society as team members in the treatment of chronic pain (1997b). The potential of occupational therapy is not in doubt but there is sparse evidence of implementation or practice experiences. Knowledge of occupational therapists working in primary care working with CBILBP An initial report (CSAG, 1994) and subsequent clinical guidelines (Waddell et al., 1999, Newton et al., 1999, Royal College of General Practitioners, 1999) recommend the bio-psycho-social assessment and treatment of patients with acute low back pain. The intention is to minimise future chronicity and disability by the identification of 8 psychosocial risk factors and to recommend multi-disciplinary treatment and management. Occupational therapists are well qualified to offer biopsychosocial assessment and treatment programmes for patients, to encourage problem solving skills and to prevent the onset of a chronic lifestyle (O’Hara, 1996). Their focus on occupational performance makes them essential personnel for the patient with reduced physical and emotional strategies consequent to the pain (Unruh et al., in Strong et al., 2002). Little et al., (1996) and Newton et al., (1999) were not reassuring about the implementation of the CSAG recommendations overall and occupational therapy was not categorised: neither was occupational therapy included in the advisory group (Waddell et al., 1999). Koes et al (2001) compared international clinical guidelines for the management of low back pain in primary care and commented that guidelines for the United Kingdom included acute pain, rather than chronic pain, assessment and treatment. However four main groups of psychosocial risk factors for the development for chronic disability are listed. The United Kingdom guidelines are commended, as they are common for all primary care health professions although the list does not include occupational therapists. Further commendations are cited for a compilation of their recommendations and for upgrading the recommendations as new evidence has become available (Newton et al., 1999). Specific recommendation for chronic pain is to refer for exercise therapy. No literature was found on occupational therapists’ contribution, knowledge of, or adherence to clinical guidelines for assessment and treatment of acute or chronic low back pain. The National Occupational Therapy Pain Association (NOTPA, 2004, Appendix G) recommends that therapists have a certain level of knowledge about pain and its management. The joint publication of the College of Anaesthetists & the Pain Society (2003) reinforces that all personnel involved in the management of chronic pain, not 9 specifically low back pain, should be trained ‘adequately to ensure a safe and effective service’. NOTPA (2004) and Birkholz & Aylwin (2000) stipulate occupational therapy remit as goal setting and graded activity pacing, to reduce flare-ups and setbacks, to improve occupation, as part of the interdisciplinary pain management team. It is unclear if they relate this to primary care, as well as the established residential pain management programmes in tertiary care, for patients with prevalent symptoms. There is concern that lack of training for occupational therapists in chronic pain may account for the lack of input (Strong et al., 1999, Carruthers, 1997). A study by Jones et al (2000) concluded that education about chronic pain had a significant effect on the beliefs of occupational therapists working with this client group, but a study has yet to emerge about the evidence of the impact on practice as a consequence. Brown (2002) and Steuart-Corry et al., (1997), discerned that occupational therapists working with chronic pain patients were unable to reach a consensus on treatment approaches, although they did not define low back pain or refer to primary care specifically. In their letter to Carruthers & Madeley, Steuart-Corry et al (1997) state that although there is basic training for occupational therapists in pain management at undergraduate level, there is every need for further training to extend understanding and techniques in pain management. Potential of occupational therapy in primary care preventing disability in CBILBP patient Gaynord (1996) presented a case study of a patient with fibromyalgia and osteoarthritis in an endeavour to clarify the role of the occupational therapist in primary care. She wanted to demonstrate that primary care therapists were well suited to long term rehabilitation support by reporting clinical details. The co- 10 operation of the patient, family and occupational therapist lead to improvements in the patient’s coping strategies. The patient enhanced functional levels through improved sleep, relaxation practice, goal setting and pacing and the provision of appropriate household aids. It has been recognised that occupational therapists are well qualified to manage pain from a holistic perspective (McCormack, 1990) with their focus on increasing the patients level of functioning (Shannon, 2002, Chesney, Brorsen, 2000, Moran & Strong, 1995). There is no indication in the literature that pure occupational therapy intervention in primary care prevents disability in long term chronic back pain, rather it decreases disability. Taylor’s (2001) examination of undergraduates over their three year training established that patient independence is only empowered when they have some choice in their treatment. O’Hara (1996) opined that specialist equipment, for patients with chronic pain, is provided when its use will help the patient to regain control over the practical aspects of their lives. If the equipment enables the family member to care more easily for the patient, then the invalid role is reinforced. The therapist’s role can be to provide information relating to equipment so that the patient is able to make informed choices about purchasing equipment. Davis (1996) in her paper on primary care management of chronic musculoskeletal pain identified chronic pain as a common problem and that treatment was inconsistent. Having acknowledged the ongoing effects of chronic pain she made suggestions for the assessment and treatment in primary care. Several theories were recommended including pharmacological intervention, physical therapy and relaxation, with no suggestion of appropriate therapists or of low back pain specifically. Turner (1996) undertook a meta-analysis of educational and behavioural approaches for back pain in primary care based on randomised trials. She concluded 11 that a cognitive behavioural approach to treatment may be appropriate, particularly as a means of preventing the progression of acute back pain to chronic disabling back pain. However more studies are recommended. A physical therapist is mentioned as a contributor to treatment, but it is unclear if this is a physiotherapist or an occupational therapist as the article is of American origin. Apparently occupational therapists have the skills and approach for clients with low back pain but there is no account of the outcomes of the intervention. Can occupational therapy in primary care stand alone for CLBP or is a multidisciplinary approach more effective? Desirable Criteria for Pain Management Programmes (The Pain Society, 1997a) stipulates that no single profession can possess all the skills required to effectively address patient needs in pain management programmes. Fixed sessions for healthcare personnel including occupational therapists (Royal College of Anaesthetists & the Pain Society, 2003) should be available. O’Hara (1996) supports the multi-disciplinary approach to chronic pain as it provides mutual support for the patients and a forum within which they have shared experiences, symptoms and fears. She sees it as an extension of what she calls the uni-disciplinary model, which is an interaction between the patient and one clinician only. Emulating much of the literature she interprets, rather than researches, the role of occupational therapists opining that the aim of intervention in pain management is educative and participative, so that the patients play an active role in their own treatment. Clinicians suggested include an occupational therapist, physiotherapist, clinical psychologist and nurse and she maintains that the range of core skills available in this combination support the patient in learning to manage pain. 12 Birkholz & Aylwin (2000) reinforce the premise that occupational therapy is a specialist area within a specialised multi-disciplinary team and that pain management is successful because of the mixed input of the specific skills. Criteria for pain management programmes as prepared by the Pain Society (1997a) recommended an occupational therapist trained in pain management as a key clinical member. One short report was found relating to an occupational therapy treatment programme for chronic pain (Carruthers, 1997), but this was not specific to low back pain. The paucity of exercise was identified, and physiotherapy input as part of the programme was recommended as essential to address this limitation. Patients attended for two hours weekly, learning to take responsibility and control through task performance and education. Interactive group work was a positive approach, repetition of information facilitated learning, and the format of the programme was continuing to evolve despite the lack of resources. Several years ago Strong (1987) suggested that patients with chronic benign pain including low back pain, needed to be treated by a team of variously skilled practitioners including occupational therapists. The consensus between her (Strong, Unruh in Strong et al., 2002) and O’Hara (1996) is that occupational therapists are core members of a multi-disciplinary team. Both authors favoured a multi-disciplinary approach to all chronic pain management and discussed occupational therapy as part of that formula. In a separate article Strong (1998) did suggest incorporating cognitive behavioural therapy with occupational therapy as a psycho-educational treatment for low back pain. Patients in the treatment group showed greater improvement over time than the control group in terms of increased patient control and reduced helplessness, disability and pain intensity. The occupational therapy programme complemented the input of the psychologist. 13 Phenomenology as an approach to occupational therapists experiences with CBILBP. That phenomenology is well suited to occupational therapy study has been acknowledged by Kelly (1996), and demonstrated and debated at length by Finlay (2000, 1999, 1998, 1997). Finlay’s (1999) evidence was based on her study of clinical reasoning strategies, which lead her to conclude that occupational therapists actually use a phenomenological process of multi-dimensional thinking anyway to understand individual’s meaning. Tryssenaar’s (1999) study enabled understanding of the phenomenon or experience of what it was actually like becoming an occupational therapist in practice. The case study approach generated elaborate and extensive data to identify the emergent themes of the experience, while encouraging the researcher to reflect on her own experience and practice in an empathic fashion. Very recent studies (Reynolds & Prior, 2003, Reynolds, 2003) questioned patients about the value of artistic intervention. Reynold’s (2003) own study favoured in depth interview rather than the template approach to gather clues of the patients’ experiences. Henare et al (2003) employed patients’ paintings, and their explanations of these paintings, to gain an understanding of the reality and experience of patients’ chronic pain. The phenomenological methodology of exposing emergent themes in that study enabled one practising occupational therapist, one occupational therapy lecturer and one nurse lecturer to gain a greater understanding of the common losses and lives of chronic pain patients, while encouraging patients to share their experiences. When questioning parents of children with Juvenile Idiopathic Arthritis, Schroder et al (2003) were able to gain greater perception of parents’ perceptions through semistructured, flexible interviews, which extracted information on the struggles and concerns of parents. The information would be utilised when working with other 14 parents with arthritic children. In similar vein, Finlay (1998) was able to gain insight and make sense of what occupational therapists felt about their patients. While acknowledging certain limitations of their study, Helm & Dickerson (1995) gained useful feedback on the effect of hand therapy to modify intervention in occupational therapy using video taped interviews. Udell & Chandler (2000) confirmed that their phenomenological study was well suited to the topic and yielded rich data on the opinions of three Christian Occupational Therapists addressing the spiritual needs of clients, using an interview format. The phenomenological methodology in the quoted studies was receptive to the experiences and expressions of the therapists and patient interviewed. The information was gathered at face value, and the emergent themes of the studies were collated as evidence-based practice for future interventions. A more formal quantitative approach may have been stilted and failed to allow the data to evolve through the descriptions of those studied (Schroder et al., 2003, Finlay, 1998). A close biographical account of the experiences of higher degree graduates (Dawkins & May, 2002), could never have been explained in quantitative terms. Vigilance about trustworthiness reinforced the researchers’ desire to elaborate the true facts (Schroder et al., 2003, Udell & Chandler, 2000, Finlay, 1998). Crotty (1996, p19) reasons that nurse researchers require a ‘method of enquiry that will not prejudice the subjectivity of the experience under study’. Reflexivity is the responsibility of the researcher and bracketing presuppositions and preconceptions (Henare et al., 2003, Schroder, 2003, Udell & Chandler, 2000, Finlay, 1999, Crotty, 1996) during data collection and analysis recorded as true an account of the subjects’ viewpoint as possible. Common themes in the data were identified and recorded, with minimum bias. 15 The literature review has identified the current state of research, located theoretical frameworks and drawn implications for the research to explore (Grbich, 1999). The paucity of evidence of occupational therapists’ experiences suggested potential to elaborate. Much of the more recent research on chronic low back pain is based on the outcomes of multi-disciplinary pain management programmes working in a cognitive behavioural approach (Williams et al., 1996, Gough & Frost, 1996, Moran & Strong, 1995). The responsibilities of each team member are not isolated, even if the team members are identified. A systematic review (van Tulder et al., 2000) of behavioural treatment makes no reference to clinicians involved, or occupational therapists’ experiences. The literature established that the knowledge and input of occupational therapists with this client group is unclear. Shannon (2002) confirmed the dearth of documentation on the efficacy of occupational therapy treatment in multi-disciplinary pain management programmes. While opinion suggested there was no shortage of confidence in the ability of occupational therapists to work with this client group, there was little evidence of their experiences or effectiveness. Particularly difficult to decipher is the occupational therapy contribution in the preferred multi-disciplinary care approach to pain management or the occupational therapists providing individual treatment. Phenomenology has been rationalised as a suitable methodological approach for research founded in occupational therapy particularly as a rich source for evidence based practice (Henare, et al., 2003, Taylor, 2000, Helm & Dickerson, 1994). Methodology Methodology has been interpreted as the theory or approach underlying the method (Racher, 2003, Sim, Wright, 2000, Koch, 1995, Silverman, 1993). Phenomenology is a qualitative research approach with roots in philosophy and psychology, and it 16 focuses on the lived experience of humans (Taylor, 2000, Corben, 1999, Polit & Hungler, 1997, Bowman, 1994). Crotty (1996) suggests that humanistic psychology has played a significant role as it centres on experience as a phenomenon in the study of man. Phenomenology allows individuals to describe their real experiences in their own words (Sim, Wright, 2000, Grbich, 1999, Bowman, 1994). Polit & Hungler (1997) present it is a useful approach when a phenomenon has been poorly conceptualised or defined, as is the topic for this study. The concurrence is that phenomenological research is underpinned by the writings of Edmund Husserl (1859 -1938), (Racher, 2003, Grbich, 1999, Corben, 1999, Finlay, 1999, Seymour & Clark, 1998). Husserl posited phenomenology as the only rigorous science that was not tainted by subjectivity and this is measured by the researcher‘s ability to suspend previous knowledge while gathering new knowledge (Racher, 2003, Lowes, Prowse, 2001, Seymour & Clarke, 1998). Suspension is achieved by bracketing out or putting to one side preconceptions and beliefs following examination and acknowledgement, while remaining open to the participant’s point of view in the experiences reported (Finlay, 2000). This openness is termed intuiting (Grbich, 1999, Polit & Hungler, 1997). The focus of the theory is the interpretation of people’s experiences with a certain phenomena or concept and to describe lived experience and perceptions (Finlay, 1997, Polit & Hungler, 1997) by returning to the phenomenon (Sim, Wright, 2000, Grbich, 1999). This makes the key elements description and interpretation of the gathered information (Seymour & Clark, 1998). Traditionally the philosophy considers that humans exist quite independently (Grbich, 1999) and their unique experience of the world is a result of that existence (Dawkins & May, 2002). Phenomenologists attempt to understand phenomena or human activity from the viewpoint of the person being studied, in the belief that individuals need to be understood within their everyday environment (Dawkins & May, 2003, 17 Shepherd et al., 1993). The phenomenon here is the therapeutic strategies used by occupational therapists working with patients with low back pain (Guidetti, Tham, 2002). Phenomenology has been proposed as an exercise in critique (Crotty, 1998, Seymour & Clark, 1998, Koch, 1995), which encourages some evaluation of all that is taken for granted (Grbich, 1999, Kelly, 1996). The main source of data in phenomenological research is the co-participation of researcher and participant in deep conversation. The participant takes the lead and the researcher strives to enter the individual participant’s world or experience (Lowes, Prowse, 2001, Polit & Hungler, 1997). Everything is examined at first hand with an open mind, and ‘the data must be allowed to emerge in their own form and speak for themselves’ (Crotty, 1996, p20) as common themes relating to the phenomenon under discussion. The research interview is a purposeful, data-generating activity and a good interview generates quality data (Lowes, Prowse, 2001). Due to the debate surrounding the phenomenological approach (Lowes, Prowse, 2001, Annels, 1999, Finlay, 1999, Koch, 1995), this study chose to adopt Crotty’s (1996) theory. He posited that phenomenology today is about ‘people’s subjective, everyday experiences’: that is ‘ experience as people understand it in everyday terms,’ where the term ‘phenomenon’ is interchanged with the term ‘experience’ (1998, p83). In his book (1996) he debated the use, and interpretation of, phenomenology in nursing research, referring to thirty studies apparently employing the phenomenological approach. As a result of his study he devised a ‘step by step methodological research process’ (Crotty, 1996, p158-159) based on the core principles (Grbich, 1999) of phenomenology philosophy. 18 The research question and the evolution of the data often dictate the framework of qualitative research, and Crotty’s theory lent itself to the flow of the topic under investigation. The aim of this study was to determine how occupational therapists facilitate patients in primary care with chronic benign intractable low back pain. One way to determine the outcome was to question occupational therapists about their work, to record, analyse and understand their experiences, while suspending and bracketing any personal preconceptions and beliefs of the author in production of the findings. The stepwise process runs through five stages. 1. The focus on the point of interest, that is the phenomenon. 2. The phenomenon is as it really is. This is established by listening and laying aside all previous ideas judgements, feelings, assumptions, connotations and associations that the researcher would think about in a general situation. 3. The documentation of the description of the experience is based on specific responses. 4. The description comes from the sample and it does not include any interpretation on the part of the researcher. 5. The information is true and characteristic. (Adapted from Crotty, 1996, p158-159). This process will be demonstrated by this study. Ethics Ethical approval for this study was granted by the local Research and Development Committee, the University Ethics Board and the local Research Ethics Committee. Ethics committees may be the gatekeepers but ultimately it was the researcher who 19 was responsible for ensuring that the project was ethical throughout the study (Sim, Wright, 2000, Seale, Barnard, 1999). The fundamental ethical principles for research (Butler, 2003, College of Occupational Therapists, 2003, Sim, Wright, 2000, Seale & Barnard, 1999, Polit & Hungler, 1997) required that the researcher: protect the autonomy of others (autonomy), respect the dignity of others (respect), promote others wellbeing (beneficence), refrain from causing harm (non-maleficence), deal with others fairly (justice). The design of this study involved the use of a survey questionnaire and telephone interview. Each approach had some ethical implications for the researcher. Both approaches required participant consent: one was implied by the return of the questionnaire and the other written, to take part in a telephone interview. Informed consent is sometimes problematic in a qualitative approach to research as the exploratory nature makes it difficult to introduce and explain (Polit & Hungler, 1997). The introductory letter (Appendix C) to occupational therapists contained a full explanation of the process and nobody was approached for telephone interview without the opportunity to acquire sufficient information (Sim, Wright, 2000), or to ask for further explanation. Written consent was obtained for all telephone interviews and all parties were offered the right to withdraw from the study at any time (Seale, Barnard, 1999, Parahoo, 1997). Telephone interviews were offered as a paced experience to minimise any discomfort, at the therapists’ convenience. Ongoing or process consent (Polit & Hungler, 1997) was recognised by member checking when participants collaborated in the ongoing decision making within the study. 20 Confidentiality of data was protected as transcripts and data were coded and identities were secured elsewhere (Taylor, 2001, Seale, Barnard, 1999, Grbich, 1999). All information was respected as valid, and consent to formal member check was agreed at the conclusion of the telephone interview to ensure that participants felt fairly represented in the analysis of the data (Tryssenaar, 1999, Polit & Hungler, 1997). Moral or legal obligation about exposing confidential information was not challenged (Butler, 2003, Polit & Hungler, 1997). The tape-recorded interviews were erased at the conclusion of the study. Continued contact with the sample can be an issue if participants are known to the researcher, or if they work in the same environment, as it can blur the specific role as researcher or practitioner (Butler, 2003, Conneeley, 2002). Co-opting clinicians from other Health Boards and Trusts gave the parity of sample but guarded against the perils of direct daily contact. It precluded potential bias or flawing of data by researcher or the participants (Butler, 2003), due to familiarity or misguided loyalty. The author is satisfied that she has adhered to the research standards of the College of Occupational therapists. (2003). Design Since the literature review revealed a lack of research in the experiences of occupational therapists working with patients with chronic low back pain, an exploratory approach to this study was elected. Pilot Study 21 A pilot study was carried out to improve and assess the feasibility of the projected study (Sim, Wright, 2000, Polit & Hungler, 1997, Ballinger & Davey, 1998, Walker, 1996), particularly to establish clarity of the questions, to obtain constructive criticism on the format, content, and the length of the questionnaire. Questionnaires were posted to three occupational therapists not included in the main study with an explanatory letter, a comments sheet (Ballinger & Davey, 1998), and stamped addressed envelope (Appendix B). The study resulted in minor adjustments to the questionnaire to encourage completion of the questionnaire. Please complete ALL the questions whether this is your remit or not. Please answer the following questions even if you have answered ‘No’ to questions 12 and 13. A question was added to clarify respondents’ definition of chronic pain to ensure parity of understanding of the condition for discussion, and a larger box was provided to elaborate on multi-disciplinary preferences. Due to the constraints of time the study ran with these adjustments. In terms of face validity, the respondents were able to relate the content of the questionnaire to the study under review. Content validity was assured by requesting information on various facets of the occupational therapists’ experiences of patients with low back pain (Sim, Wright, 2000, FoulderHughes, 1998 Parahoo, 1997). The answers to the pilot study confirmed reliability as the participants interpreted the instructions in the same way (Foulder-Hughes, 1998, Parahoo, 1997). It was decided to use the original telephone interview format, as it was designed to encourage participant lead with only prompts or reflection from the interviewer, allowing flexibility to encourage the richness of data. The same ethical considerations applied as for the main study. 22 METHOD Sample Permission and names of practising occupational therapists were obtained from eight Head Occupational Therapists (Appendix A), from four areas of Mid-Wales. The list of names made it easier to follow up those who did not return the initial survey (Curtin & Jaramazovic, 2001). Only one Head declined due to shortage of clinicians and an emphasis on hospital discharge. Forty occupational therapists were selected at random by an independent clerk. A postal survey questionnaire (Appendix C) was distributed to ascertain that there was occupational therapy available for patients prior to attending the tertiary in-patient programme. This was to record a profile about the respondents (Foulder-Hughes, 1998), and included open questions to gain detailed views and perceptions of the sample (Curtin & Jaramazovic, 2001). A questionnaire was chosen to encourage respondents to comply because they were not faced directly with an interview (Foulder-Hughes, 1998, Ballinger & Davey, 1998), and to gain a smaller sample for telephone interview. Returned questionnaires implied consent to use the data. Inclusion criteria for telephone interview were, occupational therapists working with low back pain patients in primary care. A purposive, that is a typical (Sim, Wright, 2000, Polit & Hungler, 1997), criterion sample of five occupational therapists working with chronic low back pain was selected. All volunteered (Dawkins & May, 2002) to take part in the telephone interview at a time convenient to them for which individual informed consent was obtained. Data Collection Data collection tools were: 1. A survey questionnaire (Appendix C) to identify occupational therapists working with chronic low back pain, requesting demographic background and open 23 questions designed to elicit the broader context of the occupational therapists’ experiences with patients with chronic low back pain. 2. A tape-recorded telephone interview with a prepared interview schedule (Appendix D) to elucidate the verbal account of occupational therapists’ experiences with chronic low back pain. Triangulation which is the implementation of more than one collection technique in one study increases the probability of revealing richer data (Hammell, 2002, Sim, Wright, 2000, Polit & Hungler, 1997, Silverman, 1993), leading to richer information for analysis. Survey So that non-respondents could be sent another questionnaire to maximise the response rate (Curtin & Jaramazovic, 2001), postal questionnaires were coded and logged (Ballinger & Davey, 1998) and sent to forty occupational therapists in the Local Health Boards and Trusts. Information on the study, consent forms for telephone interviews and stamped addressed envelopes were included (Appendix C). Non respondents received the questionnaire twice over a two-month period. Returned questionnaires were logged and the data recorded under question numbers and topics. Demographic data was tabulated and numbered under the headings of 1. age, gender, years worked, title, type of work, client group, qualifications 2. training in pain, additional training in pain, work with pain now, ever worked with pain 3. reason for referral, origin of referral, multi-disciplinary working and requirements for additional training about pain and confirmed the background of the respondents. Open responses were recorded as question numbers and headings under definition of chronic pain, clinical guidelines for low back pain, effects of chronic low back pain, 24 strengths and weaknesses of patients with low back pain, interventions offered, progress observed and the effects of occupational therapy intervention. These questions elaborated the therapists’ observations and understandings of the patient with chronic low back pain. Interviews Unstructured interviews were designed to elucidate the participants experience without imposing any of the researchers personal views, particularly when the researcher had no concrete views (Polit & Hungler, 1997), and took place over a four week period. Interviews were preferred as potentially they yielded deeper data (Parahoo, 1997). The integrity of the interviewee was respected at all times (Sim, Wright, 2000), and the primary data collection instrument was the researcher who interviewed and listened to the recorded data (Conneely, 2002, Beck, 1994, Sheperd et al., 1993). The resulting data was a creation between the researcher and the researched (Polit & Hungler, 1997, Koch, 1995) with an emphasis on the opinion of the participant (Seymour & Clarke, 1998). Telephone interviews were chosen to limit the amount of travelling involved for face to face interviews in a large rural area, and were arranged following receipt of consent forms from volunteer therapists. Background information was discussed and times were set to cause least disruption in the busy schedules of participants and researcher. Interviewees were advised to ask for breaks at the outset of the interview to avoid fatigue. Interviews lasted from 15 minutes to 45 minutes and were numbered one to five. The interviews were guided, semi-structured and circular to yield conversation (Sim, Wright, 2000, Crotty, 1996). The interviewer prepared broad, open ended questions 25 on the interview schedule, to avoid bias (Pearce & Richardson, 1996), initially inviting the therapist to ‘tell’, as an icebreaker to talk (Hand, 2003) about the assessments and interventions they offered patients with low back pain. The researcher demonstrated active listening (Sim, Wright, 2000, Crotty, 1996) and encouragement by prompting, probing, reflecting, paraphrasing and discussing with the interviewee. The interview did not follow an exact order, as some flexibility was desirable to allow the researcher to follow up issues raised. The interview schedule was prepared to ensure that all participants reported on the same topics to aid reflection, but was not designed to inhibit the intuiting of the researcher or the flow of the participant. The interviews explored the experience of working with chronic low back pain to generate data based on the respondents’ personal experiences (Dawkins & May, 2002, Parahoo, 1997). Permission to member check was requested at the conclusion of each interview. All participants agreed to read the interview hard copy to authenticate the content. The researcher jotted phrases in a reflective diary as the interview allowed and then recorded related reflections (Taylor, 2001, Sim, Wright, 2000, Grbich, 1999, Finlay, 1998), within two hours of the completed dialogue. There were also opportunities to debrief with colleagues, none of whom are occupational therapists, but who are experts in the area of pain management and one who is an experienced researcher. The tape-recorded interviews were scribed individually by an independent cleric and the hard copies distributed to the participants for authentication (Appendix E). Data Analysis Analysis and results were based on the aptitude of the analyst (Lowes, Prowse, 2001, Holloway, Wheeler, 1998), and the individuals’ representation of their experiences (Seymour, Clark, 1998). Initially the accuracy and quality of the data 26 depended on what the respondent wanted to disclose and the integrity of the sample to contribute accurately (Pope et al., 2000, Parahoo, 1997, Silverman, 1993). The analysis of survey and interview texts was performed manually (Sim, Wright, 2000) with the aid of a word processor. The researcher devised her own method of analysing the data, which on later reading compared to the editing analysis or categorisation scheme described by other writers (Taylor, 2001, Polit & Hungler 1997, Bowman, 1994). This involved comprehending, synthesising, theorising and recontextualising, moving backwards and forwards from the raw data to emergent themes. This approach worked best for the researcher (Sim & Wright, 2000, Polit & Hungler, 1997). Data provided a description, but not an explanation, and the role of the researcher was to sift and interpret to make sense of what had been reported (Pope et al., 2000). Although critiqued as a rather laborious process it enhanced the data rather than reduced it to numerical coding. Survey The demographic material had been coded and sectioned under headings at collection and the categories were then totalled, collated, recorded and reported. Individual open questions were analysed independently on separate sheets and categorised into common topics. By reading and rereading the responses new categories emanated from the text until no new categories were realised. The responses to these open questions reported broader data on therapist experience than anticipated. It was decided to store these findings before the interview process began (Polit & Hungler, 1997). This was to reduce bias and to bracket the information before collecting data yet to be revealed by the telephone interview. Interview 27 After verification of the text by the sample therapists, the researcher read the texts several times to get a feel of the interview and the experiences of the interviewees and the interviewer. Themes emerged after repeated reading and were drawn from common words, phrases, sentences and themes that highlighted any commonality (Dawkins & May, 2002, Taylor, 2001, Corben, 1999). The highlighted text was then categorised in accordance with the aims of the study, and recorded on separate sheets under the headings of Assessment and Intervention, Clinical Guidelines, Disability Prevention, and Multi-disciplinary/Individual Therapy. During the reading additional themes emerged which were tabulated under the headings of Reasons for Referral, Holistic Approach, Concerns of Occupational Therapists and Independence and Empowerment. All quotations were numbered according to coding of participants and page numbers from the text. Each category was reread and re-evaluated several times to compare and synthesise the comments of each section. Therapist quotations were reported to support the outcomes presented. The open question response and interview response themes were compared for further commonality (Henare et al., 2003, Bowman, 1994) using the same technique, and the findings were presented in the Discussion (p 40). Results SURVEY QUESTIONNAIRE Demographic Background: (Questions 1 to 9, 11 to 13, 15 to 17, 23, 24, 26) Twenty six occupational therapists responded to the postal survey. Eight were unable to complete the exercise either because there was no service in their area or they did not feel qualified to answer. One therapist was actually taking a career break. Some questions were omitted by respondents, and the figures for individual question response are included in each question result. 28 The majority of participants were aged 30 to 50 years with one under 30 and three over 50 years. Sixteen females and two males responded. Twelve therapists had qualified by Diploma in Occupational Therapy, Five BSc OT and one had a post graduate MSc OT. Therapist years of service were recorded as: 1 to 5 years 5 to 10 years 11 to 15 years > 15 years 4 Therapists 3 Therapists 3 Therapists 8 Therapists The majority ranked themselves Senior Occupational Therapists, five were Heads of Departments and two Basic Grade therapists. Many therapists were employed in more than one area of work in hospital and community settings, Acute Psychiatry, Elderly Mentally Ill, Out Patients and Community. No one worked purely with chronic low back pain patients although eleven clinicians reported some input with low back pain patients now. Patients were not referred for low back pain alone, but rather for depression or physical assessment in mental health services and general functional assessment and rehabilitation at home or work for non specific physical conditions in physical health. Referrals were taken mainly from GPs with fewer from other professionals and Consultants. Therapists reported seeing patients for assessment and treatment who had experienced low back pain for: 3 months 6 months 1 year 18 months 2 years >2 years 1 therapist 4 therapists 4 therapists 1 therapists 2 therapists 6 therapists Only one therapist reported definite training for chronic low back pain, although two had actually spent a short time at a back school, and two had done short 29 placements. Therapists had not attended additional training and were generally self-taught through reading of journals or talking to physiotherapists. Ten therapists said they would like more training. All therapists preferred multi-disciplinary team work to give the maximum input to patients, utilising the breadth of combined expertise. Quotations included ‘each discipline would have unique perspective and advice’, ‘so that the person is worked with holistically’. The initial sample experiences then were broad, working in physical and mental health, generally at a senior level. Low back pain was not a primary cause for referral and back pain assessed was chronic (had lasted longer that six months). Training in chronic pain was sparse and multi-disciplinary working was the favoured option. Clinical Guidelines for Low Back Pain (Questions 18, 19) Acute low back pain Chronic low back pain Not one of the seventeen responding Not one of the fifteen responding therapists was aware of any formal therapists was aware of any formal clinical assessments clinical assessments In Practice Reported approaches and suggestions Reported approaches and suggestions for assessment of acute low back pain for the assessment of chronic low back pain Read medical history, noting previous full medical history as would expect interventions, patient take history from patient’s view, Observation Occupational probably already altered lifestyle to accommodate problem therapy functional 30 observation occupational therapy functional / assessment / ADL lifestyle Review of exacerbating pain features, measure the effects of the pain rather patients perception of level of pain, than causes posture, transfers seating/bed, assessment / ADL to patient’s perception of pain and driving, work, leisure exacerbating features, posture, Concentrate on patient goals transfers, seating/bed, driving, work, Would pass on to physio leisure Although there was no knowledge of the CSAG guidelines (1999, 1996, 1994), particularly acute guidelines and the prevention of disability, the consensus report in approach to assessment in both clinical areas focussed mainly on the physical presenting symptoms and the patients’ ability to cope with their everyday demands. One therapist wrote that she would look at the triggers for both and focus on how to minimise them. CATEGORIES FROM OPEN QUESTIONS The results not directly answering the aims are presented in Appendix F. Interventions (Question 21) This question asked for interventions offered or that would be offered to patients with chronic low back pain. The analysis of fourteen responses revealed a high proportion of physical interventions including the use of equipment, emotional issues, problem solving and education. Physical interventions recommended: functional, environmental, workplace, home, driving, ergonomics of home and work environment assessments graded exercise fatigue management, relaxation, energy conservation and joint protection 31 physical coping strategies and lifestyle advice such as transfers from chair, posture and manual handling, providing equipment for example a wheelchair, and compensatory techniques to enable maximum performance One therapist working in mental health recorded referral to colleagues in physical service for specialist input and another, immediate referral to a Consultant, GP or general hospital for specialist input. Neither defined the nature of specialist input. Interventions for emotional issues recommended anxiety management assertiveness training talking therapies mainly The enhancement of problem solving skills, were suggested as well as patient education to enable self-sufficiency and independence. Specific approaches were Solution Focussed Therapy goal setting, planning and pacing alternatives, enabling techniques for carrying out ADL, work and leisure balancing work, rest and play and evaluation education about the back and potential damage education re-good posture, exercise programme and back strengthening One therapist noted working in conjunction with the patient to identify ADL/occupation the individual is having difficulty with, and to provide interventions to address these areas. Overall the interventions recorded, emulated the holistic approach gathered from other open questions. TELEPHONE INTERVIEWS 32 Nine therapists gave consent to a telephone interview although only five actually confirmed working now or ever with chronic low back pain. Three therapists worked in community mental health, one in hospital and community physical, and one worked with elderly rehabilitation in hospital and community. All were of a senior grade and carried their own caseload. Results emerged during the analytical process (Polit & Hungler, 1997), and were scribed under headings taken from the aims of the project and additional themes that emerged in the analysis. Assessment and Intervention Assessment Therapists reported the use of a holistic and general occupational therapy assessment, not specifically geared to low back pain but which highlighted the effects of back pain. Primary assessment would be from a mental health perspective and obviously we take into account then if people are having problems with pain management…. (Therapist 3) No specific assessments ………………….general occupational therapy assessment……..I would find out exactly how it’s affecting their everyday life to make sure we can gear the intervention part for them (Therapist 1) Most problems….are sort of multi-complicated………….I tend to look at them as what are the problems and what can I do to help. (Therapist 2) One therapist favoured a common sense approach to find the patient’s perspective on what they wanted and what they felt would help, as well as a home visit to check out the environment for potential adaptations. She used a talking solution focused approach to enable patients to identify the immediate functional difficulties impeding their lifestyle. Another used a broad multi-disciplinary physical and cognitive assessment, also used by nurses and physiotherapists, to identify all the problems the patients were having. They looked at patients’ lifestyle, perception and beliefs about increased pain. The patients with low back pain were very chaotic and so previous interventions and present coping strategies were reviewed. One therapist in 33 mental health suggested that she would refer the patient to an occupational therapy physical service if available. Another identified the appropriate referrals herself from the weekly referral meeting. Intervention The patients with back pain were fairly entrenched and required longer-term intervention. Common approaches to intervention were improving function by employing activity scheduling, goal planning, and pacing, while problem solving through talking. Showing them how to do things in a different way rather than the way they did things before ……their back pain………….perhaps they used to cut the whole hedge…………….to do half an hour today and half an hour tomorrow……….looking at how they manage their anxiety…. things like confidence building (Therapist 3) A variable approach to the supply of aids and adaptations was apparent and therapists:- …….would deal with the practical side of things….….there is a fair bit of chair raising, and toilet raising, grab rails and that kind of thing (Therapist 2) ………do look at equipment in the short term……we try not to use equipment at all………….unless we feel we cannot work with the client………..if they’re not ready to accept that the pain can be alleviated (Therapist 5) One therapist found that moving and adapting the home with equipment reduced physical dysfunction and emotional distress and improved patient control. It was a joint problem solving process between the patient and therapist to find a way of doing things. She was not the only therapist to offer relaxation exercises. Three therapists focused on talking therapy, and detailed pacing and cognitive plans to manage the over activity cycle. She was the only clinician to address the unthreatening nature of chronic pain with the patients. 34 The data revealed a limited range of specific intervention for chronic back pain which focused mainly on enabling patients to work with their pain. One therapist identified the need for education about chronic pain and no therapists mentioned pain relief. It was a management of ongoing pain, allowing the patients to live more easily with it. The general approach to intervention demonstrated practical coping strategies with some cognitive input to increase the patients’ overall self-management. The supply of aids and adaptations was seen as a facilitator by two therapists, while one considered them unnecessary. All therapists were competent to offer some pain management strategies using occupational therapy principles. Clinical Guidelines No interviewees had knowledge of any clinical guidelines for the assessment and treatment of chronic low back pain. I don’t follow any particular guidelines. (Therapist 1) I haven’t got access to any specific to low back pain. (Therapist 4) However one therapist admitted that she would like some and another assumed that they existed but she did not know. Disability Prevention There were varying attitudes to the ability of occupational therapy to prevent patient disability. Prevention was impeded by the timing of referral and, therefore, the timing of intervention as well as on the poor understanding of chronic pain by other professionals. Things have become really entrenched and we often wonder if they’d been seen earlier or if psychological problems had been tackled earlier, whether or not the outcomes of people would be different. (Therapist 3) I feel that what we can offer is just a glimpse really of the fact that there is a way forward………………….I feel that it is fine when we can provide the intervention but I don’t think it’s enough, it’s 35 not intensive enough for them……….There is a perception that nothing can be done…….it’s the time factor…..it’s so much easier to be handing out a prescription than to work with the client. (Therapist 5) However one therapist reported timely intervention by astute colleagues. Nursing staff are very good - if they think there is a functional problem, that I can help with they do actually refer straight on to me. (Therapist 4) Prevention depended on the attitude and motivation of the patient concerned and the willingness to take things on board, and was not necessarily related directly to the input of the therapist, but that did not exempt or limit input. ……. there are interventions that can be done, but mostly I get people in this area who accept that they’ve got aches and pains and get on with it (Therapist 2) …..we find that people look after their pain and are unwilling to view things (Therapist 5) There was conflict of interest and potential impediment if patients were over cared for by family or external agencies. A vicious circle evolved because patients were inactive due to somebody else doing it for them. There was a difference of opinion about the supply of aids and adaptations. This concerned what the patient was ready to accept and what the therapist felt was suitable. Often I find that people don’t really want things [aids] ……unless they absolutely have to have them because they don’t want people seeing them in a wheelchair as much as anything. (Therapist 2) …..look at maybe equipment and adaptations to people’s property and their home…….to see if there is anything we can do to change (Therapist 4) There was an awareness of therapist responsibility to enable the patient to visualise intervention, to achieve the potential while being cognisant of what the patient wanted and was prepared to accept. Alternative approaches were sought to reduce stress on painful joints and looking at what patients can do within their living patterns, rather than focussing on the pain. Patients referred to mental health facilities, sometimes as a last resort, presented for multiple reasons and interventions were prioritised. 36 Often the physical services do not feel that they can cope with people with mental health problems, especially if they are psychotic…… ……..They’re re-presenting because of their mental health problems, the back pain is something that we work with to try and reduce some of the problems. Because if you’ve got severe mental health problems and you’ve got chronic back pain it’s not going to be very easy is it? So by trying to get rid of some of the physical symptoms it can actually help with their mental health. (Therapist 4) Therapists accepted that timely assessment and intervention would go some way to limiting disability but this could depend on patient motivation and goals, and sometimes external factors inhibited progress. Prioritising patient needs when they presented with multiple difficulties was a consideration. Provision of aids as prevention was not conclusive. Multi-disciplinary/Individual Working Availability of multi-disciplinary team work was favoured to maximise patient opportunity through the use of complementary and individual philosophy. Other team members get involved and I think because we’ve got the ability to refer to each other quite quickly things get sorted …………………it works very well I think (Therapist 2) We can’t say that occupational therapy is the best thing out, it’s just part of an overall treatment plan for people, we need everybody. (Therapist 4) I think it’s essential with a multi-disciplinary team because I feel people that we have worked with have been looking for the magic cure and I think the fact that we do have an occupational therapist, physiotherapist and nurse……………………using the same approach …………….. gives the clients confidence that there isn’t another professional out there that may be able to cure that. (Therapist 5) I do work quite closely with our community psychiatric nurses here ……… (Therapist 1) Recognition of the strengths of multi-disciplinary working did not discredit individual occupational therapy input, and occupational therapists’ skills were recognised with a confidence in their own professional ability. In fact one therapist suggested:I think it would be the depth of the service that I could offer as an occupational therapist. I actually think occupational therapists can take a lead in it, but I may be biased (Therapist 5) 37 While managing her own caseload in mental health one therapist was sometimes called in as a co-worker for specific occupational therapy intervention, like relaxation, or to carry out an assessment for aids and adaptations. This was a short term contact and the patient was under the overall supervision of the psychiatric nurse keyworker. There was flexibility within teams to use both approaches. ……..a lot of work is done individually and then I suppose we work in both ways really so not everybody that we see has got anybody else involved in the team. It depends on the individual really………….Say you’ve got someone being treated for depression they might refer them broadly to the team or they might refer strictly to the occupational therapist or depending on what they identify and then from our assessment if we think we need to involve other people we do……………I think one person being involved is O.K. as well (Therapist 3) I do go in as an occupational therapist and do an occupational therapy assessment, and just be the only professional involved then (Therapist 2) The multi-disciplinary approach is favourable to give patients access to maximum skills according to assessment of need, but it is recognised that occupational therapy can stand alone. One comment however gave concern as it was suggested that as professionals ‘not everyone knows what everyone does’. Anecdotal discussion on the understanding of professional roles is ongoing. ADDITIONAL THEMES Reasons for Referral No therapist recollected a referral specifically for low back pain. The nearest was an example of a basic referral in mental health. Please can you see this man who had an accident at work and has been off with back pain and is now saying he’s depressed and asking for counselling (Therapist 3) Other therapists confirmed that the referrals were more general and that back pain was only part of the presenting problem:I don’t remember anybody ever being referred for low back pain ………they’d probably be referred for a stroke or hip replacement … …..with maybe lower back pain as part of that……..I think a lot of back pain would really be referred to the physiotherapist (Therapist 2) 38 Referral to us would be the mental health condition like depression or anxiety . We don’t offer a service specifically for pain management (Therapist 3) usually mental health and it’s usually because they are unable to function on a daily basis………………………..problems come from things like low back pain, that the back pain is actually so much it’s affecting their mental health (Therapist 4) The lack of a specific service for low back pain was identified, but this did not preclude appropriate treatment as part of presenting difficulties. Holistic Approach An obvious aspect of occupational therapy was the holistic approach to patient assessment and intervention. One therapist acknowledged ‘looking at the whole package’ as the patient could be having a social problem or difficulties with the home and another tended to look at everything to do with the person’s lifestyle. …..if there’s a problem that we need to look at it from all aspects whether it’s physical, mental or psychological…………I think as O T s we’re trained to do all of it………….It’s an ongoing holistic assessment (Therapist 4) I think occupational therapists have a good grounding in looking at the whole person. They have medical training………psychological training…………physical training………..allows the occupational therapist to look at the understanding of occupation in a client’s life. (Therapist 5) Occupational therapists identified the effects of chronic back pain on patients’ lifestyle and addressed physical, emotional and social aspects of life, recognising that improvement impinges on all these aspects of life style. Concerns of Occupational Therapists A lack of actual occupational therapy services for chronic low back pain is apparent. I don’t know where people go if they haven’t got a mental health problem as well …….who would deal with it on the physical side actually……… …………some doctors or departments are more familiar with OT… ………perhaps there isn’t a service in some places (Therapist 3) 39 However the participant occupational therapists were competent and motivated to treat the patients referred, while two expressed specific interest in the work of other therapists to improve knowledge. We have the skills to work with them……………I do feel it’s a huge area that occupational therapists could work with (Therapist 5) always questioning yourself whether there is any more that you could be offering…………………………..in process of changing assessments to look into a lot more detail to do with occupation…(Therapist1) Therapist 5 concluded that therapists with a specific interest in low back pain would find relevant courses to develop their skills further. The interest and competency of the sample was apparent. Independence/Empowerment Occupational therapists recognised the right of patients to be involved in their own treatment and to have an opinion about their individual needs. There’s no point in going about what I might think is best for them because it might not be what they want so it’s got to be working with them…….they are capable of doing things themselves despite them being in pain….It’s trying to get them to be a bit more confident so that they are capable of doing things themselves despite being in pain….. the aim for them is to realise this for themselves. (Therapist 1) …..making sure the person is in the centre and it’s all their ideas…. ……….the answer has come from within us……….if you’ve got the expert telling you what you should or shouldn’t be doing, it doesn’t sink in as much…………finding out what they want and what they feel will help and trying things out……….. (Therapist 4) I think we can work with people……………….which then enables them to go off and explore other avenues. (Therapist 5) A particular patient was asked what it would take to put the washing on the line and she suggested a basket on a trolley would be higher up. Because the patient came up with the idea then she was the expert. Empowerment through efficacy, as the patients realise their own potential, was a criterion for occupational therapy in the management of low back pain. Resume 40 Although the main presenting patient problem was not low back pain, and occupational therapists were not specifically trained for low back pain intervention, they demonstrated competence to work with this condition. They were able to identify the effects of low back pain, as well as work with the patient to enable them to live with the pain. Physical and emotional recommendations and problems were addressed through talking to the patient and working with patient identified needs. Aids and adaptations had some value but patients were not always receptive to using them. Whether the use of aids contributed to disability or empowerment is not conclusive. Some patients chose to manage independently without occupational therapy or multi-disciplinary intervention whether through habit or lack of motivation is undecided. All the therapists interviewed had an interest in facilitating the patient to the limit of their present knowledge, and at least two wanted more knowledge and understanding to improve intervention. Trustworthiness The author has worked in an interdisciplinary residential pain management programme for ten years and is expert in the cognitive behavioural approach to low back pain and other chronic pain disturbance. The purpose of this study was to explore occupational therapists’ experiences with low back pain in a different clinical setting. The tendency to compare her own setting actually opened up the interview discussion, and she did not assume that occupational therapists would be inappropriate in their approach to chronic back pain (Hafner, 1999). Acknowledged flaws (Savin-Baden & Fisher, 2002) in this study were mainly related to the researcher’s inexperience and her learning curve, the one impinging on the other. She understood that rigour is ensured by the use and description of systematic design (Barbour, 2001, Mays, Pope, 1995), and by reflexivity (Hand, 2003, Koch, Harrington, 1997) but took time to fully grasp the process. However by the third and 41 fourth interviews she was more immersed and relaxed into the interview content through more comprehensive listening and understanding. The researcher acknowledged her values, assumptions and background (Hand, 2003, Henare et al., 2003, Conneeley, 2002) and acknowledged the expertise of the participants within the framework of their broad case load. Reflexivity ‘distinguished how subjective and inter-subjective elements impinged (and possibly transformed) both the data collection and the analysis’ (Finlay, 1998, p 453) and recorded the researcher’s personal sensitivity to the collected data (Hammell, 2002, Mays, Pope, 2000, Koch, Harrington, 1998, Krefting, 1991) consequent to her personal experiences. The descriptions collected were a reflection of the participants’ perceptions of their own world (Finlay, 1998). The criteria of credibility, transferability, dependability and confirmability (SavinBaden & Fisher, 2002, Taylor, 2001, Polit & Hungler, 1997) were applied in this study. Credibility relied on the integrity of the occupational therapists taking part and the recurring themes in the texts. The researcher recorded in a reflective diary and took the opportunity to debrief with experienced colleagues to maintain objectivity. Triangulation was employed to ensure internal validity (Barbour, 2001, Shepherd et al., 1993), which enhanced reliability by identifying convergence of data to corroborate the overall results (Conneeley, 2002, Mays, Pope, 2000, Grbich, 1999). Member checks confirmed the accuracy of the typed interview (Dawkins & May, 2002, Trysennaar, 1999, Helm & Dickerson, 1995). The researcher’s credentials established that she was well qualified to undertake the study (Hammell, 2002, Trysennaar, 1999). The interview sample were representative occupational therapists and the full description of the research design is transferable to other settings (Taylor, 2000, Polit & Hungler, 1997, Krefting, 1991), although the reader rather than the researcher 42 takes responsibility to establish transferability to test the trustworthiness (Taylor, 2000). There was no hypothesis in this phenomenological research so there was nothing to prove or contest. Dependability was related to the consistency of the data, and was confirmed through triangulation and detailed explanation of the research process (Pearce, Richardson, 1996, Krefting, 1991). Different types of data were reconciled and proved accurate (Sim, Wright , 2000, Grbich, 1999, Silverman, 1993), and the combination of survey questionnaire with open ended questions and semistructured interview, facilitated an exploratory approach (Sim, Wright, 2000). Peer evaluation of this study may have strengthened dependability (Taylor, 2000), but the study was an assessment of personal competence. Confirmability, the objectivity and neutrality of the data (Polit & Hungler, 1997), was addressed as the researcher recorded intrusive personal opinions about the phenomenon in a reflective diary (Henare et al., 2003, Taylor, 2001), with a view to dismissing, judging and defending against any interpretation in the researcher’s self interest (Conneeley, 2002, Fisher & Savin-Baden, 2001, Koch, 1995). Confirmation of the data was achieved by member checking, informally and formally (Conneeley, 2002, Polit & Hungler, 1997, Parahoo, 1997), so that any misunderstandings or misinterpretations on the part of the researcher were checked. The complete interview was despatched for inspection and no comments were altered, therefore reliability was not compromised (Savin-Baden & Fisher, 2002, Polit & Hungler, 1997). A clear audit trail described data collection, interpretation, and sufficient data for the reader to judge the outcomes as credible (Hand, 2003, Lowes, Prowse, 2001, Barbour, 2001, Mays, Pope, 1995). Due to the sample size and the non-experimental nature of the methodology, the goal of the project was not replication or generalisation of the results (Sim, Wright, 2000, Polit & Hungler, 1997, Corben, 1999, Krefting, 1991). Rigour was ensured by the use of a systematic design demonstrating 43 data collection, interpretation, and sufficient data for the reader to judge the outcomes as credible (Barbour, 2001, Mays, Pope, 1995). Rigour was achieved by ensuring maximum trustworthiness and minimum bias (Hand, 2003, Finlay, 1998). The researcher wanted to focus on the pure data (Taylor, 2001, Crotty, 1996). It was not possible to test the data descriptions with other occupational therapists’ (Pearce, Richardson, 1996), experienced in pain management and member checking only established clarification during interview and the accuracy of the printed text. Member checking has been questioned, as a measure of proof that results are believable (Polit & Hungler, 1997) and because of the inconsistencies in its use (Savin-Baden, Fisher, 2002). This study sent the typed interview for verification, although this is not necessarily standard procedure. The researcher was dependent on the integrity of each participant to establish credibility and dependability. However, the validity of the interview responses was enhanced by the researcher, who, informally sought clarification during the interview process (Parahoo, 1997). Bracketing has been queried as a reliable approach to objectivity (Lowes, Prowse, 2001) and it has been suggested that trustworthiness and rigour are only proven when the interview process has been fully explained. If the researcher had not reported her reservations the reader would be unable to make a valid judgement about trustworthiness of the study (Crotty, 1996). Idealisation of the process would have served no purpose and the researcher took responsibility and acknowledged the reality of the process. The completed study was proof read by an independent scrutiniser. Discussion This study set out to gather the experiences of occupational therapists working with patients with chronic low back pain in primary care, and to establish available input before admission to a multi-disciplinary residential pain management programme. It 44 revealed that occupational therapy assessment and intervention is available in primary care and those therapists were equipped to enhance patients’ skills by facilitating and advising (O’Hara, 1996), although no specific service for low back pain was available. Patients were not referred for low back pain specifically, either in mental or physical health, but felt physically and emotionally empowered following assessment and intervention, due to taking responsibility for their own intervention. Achievement improved their confidence and self esteem so that they continued with self-management, increasing their leisure activities and sometimes returning to work. However some therapists felt that they could have done more, if time and structure of approach were improved. There were few contrasts (Guidetti & Tham, 2002) between the outcomes of the two sets of data. All those interviewed had worked with chronic back pain whereas the survey only identified eleven out of the eighteen working with back pain now. It is impossible to comment on the caseload of the non-respondents. The discussion will look at the combined results using the headings of the interview themes. Assessment and Intervention Assessment Assessment as described in the survey concentrated more on the physical components of the pain. A full medical history and the patient’s perception of the pain was recommended, although they identified the effects of chronic back pain and the strengths and presenting problems of patients, (Appendix F) very comprehensively. These included emotional, social difficulties and aspects of loss, as well as goal setting and motivation, which suggested deeper therapist knowledge than at first deduced. The interviews elaborated a more holistic approach employing an occupational therapy or multi-disciplinary assessment, relevant to the client group, to 45 identify all the presenting problems. Referral to mental health was on emotional grounds and back pain was not always identified, but became apparent from the holistic assessment. The two therapists in physical health quoted broad referrals requiring thorough assessment to isolate all the difficulties experienced by the patient, including back pain. In the 1980s assessment focussed on improving performance and occupational roles (McCormack, 1988, Flower, 1981), and later writers (Gibson & Strong, 1998, O’Hara, 1996) identified the expertise of occupational therapists as assessors. There is no significant change in the expertise of occupational therapists in assessment. Intervention It has been suggested that occupational therapists have been unable to reach a consensus about their treatment approaches to chronic pain (Brown, 2002, SteuartCorry et al., 1997, Davis, 1996). The survey elicited more specific interventions for patients as if therapists had been able to focus better on a written response. Suggestions included graded exercise, fatigue management, relaxation, transfers, manual handling, anxiety management, assertiveness training and education about the back and posture. Interviews revealed some focus on goal setting, activity scheduling and pacing, supply of aids and adaptations; ergonomics and relaxation were also recommended, and education on chronic pain in one case emulating NOTPA (2004) recommendations. Both reports recognised the value of talking therapy and therapeutic support. The interview could have probed further to reveal individual interventions and examples. However on further review it appeared that both revealed physical, emotional and problem solving skills to enhance patient selfsufficiency. Recommended interventions (Baptiste, 1988, Strong, 1996) do not seem to have evolved specifically and the cognitive behavioural approach (Birkholz, Aylwin, 2000, Strong, 1996, O’Hara, 1996) remains the prerogative of the multi-disciplinary 46 pain management programme reported in the literature (Williams et al., 1996, Gough & Frost, 1996). Clinical Guidelines Occupational therapists were not aware of any specific guidelines for the assessment of acute or chronic low back pain. This general lack of knowledge and implementation of clinical guidelines by all clinicians is supported in the literature (Newton et al., 1999, Waddell et al., 1999), and in fairness occupational therapists were not involved in the working party (1994). Whether this is a valid reason for lack of knowledge may go to debate, but it is increasingly challenging for all clinicians to be conversant with all guidelines, particularly when they cover a broad client group. The occupational therapists in this study did not avoid patients with back pain and their assessments highlighted patient difficulties, while their intervention enabled patients to deal with the effects and nature of the chronic back pain. The special interest group (NOTPA) is beginning to gain notoriety outside the multidisciplinary pain management programmes. There are specific recommendations and guidelines for occupational therapy practice for patients with chronic pain, which includes low back pain. Therapists in the survey confirmed that they had received very little training, if any, in chronic pain interventions, but credit goes to those who had expanded their knowledge by self learning. Only ten showed interest in further training, but therapists choose their own areas of interest in continuing development. Those who had worked with chronic back pain have unknowingly embraced several of the NOTPA recommendations by adapting their occupational practice. This suggested that occupational therapists are well qualified to apply their expertise in occupational performance to chronic low back pain, even though it is recommended that all therapists working with pain undergo extra training (Steuart-Corry et al., 1997, 47 NOTPA). Establishing consistency of practice is challenging in all areas of medicine and progress is a process. Disability Prevention The survey findings confirmed that occupational therapists were unaware of clinical guidelines for acute back pain which have been introduced to prevent the development of disability and chronicity, consequent to poor screening in the early stages of acute low back pain (CSAG, 1994). In the interview it was acknowledged that timing of referral was important to provide or encourage suitable intervention, before patients became entrenched in their condition. Motivation and aptitude of the patients to make changes to their lifestyle to enable them to live with the pain, was a concern, while it was recognised that disability could be enhanced by the acceptance of input from family or carers. One therapist in agreement with O’Hara (1996) saw suitable aids and adaptations to the home as an enabling rather than disabling factor, but O’Hara recommended caution to provide for the patient, not the carers, and patient choice was important (Taylor, 2001). The fact that some patients seemed to cope independently with aches and pains and declined aids and adaptations did not highlight the direct need for occupational therapy intervention in one case. However no opinion on the effect of discussion between therapist and patient was addressed, and patients may have felt more confident just by discussing their own coping strategies with an empathic clinician. No specific question was asked in the survey concerning disability prevention, but it was reported that weaknesses of patients included reduced stamina, low mood, negative view of illness and the effort needed to maintain lifestyle (Appendix F). It could be argued that therapists were only in a position to prevent disability with the co-operation of the patient, based on the patients’ motivation. Conversely it could be 48 argued that it is the job of the therapist to create that motivation through information sharing and support to put the theory into practice. Hafner’s (1999) conclusions about iatrogenic factors were unsupported in this study and there was no other literary evidence to compare. Multi-disciplinary or Individual Approach In the main, both outcomes favoured a multi-disciplinary approach to assessment and intervention for patients with low back pain. However all therapists in the interview acknowledged that occupational therapists also had the skills to work individually with this condition. In fact one was adamant, although maybe biased, that occupational therapists have the in depth understanding and knowledge to independently treat patients, with low back pain. The survey offered a straightforward choice between the two approaches, which limited the information supplied. One of the advantages of a telephone interview is that the interviewer had the opportunity to explore further, and was able to encourage discussion on the options rather than relying on the response to a written multiple choice question. The literature supported the multi-disciplinary approach (Birkholz & Aylwin, 2000, Pain Society, 1997, Strong, 1996, O’Hara, 1996), emphasising that occupational therapists are core members. One study by Carruthers (1997) confirmed that although the preference was more than one discipline to work with the patients, their occupational therapy programme continued to help patients with chronic pain. ADDITIONAL THEMES Reasons for Referral Both outcomes noted that no patients were referred specifically for low back pain, and one therapist in mental health expressed concern about lack of specialist 49 services locally. Low back pain was identified at assessment as a contributing factor to physical and mental dysfunction. The fact that the therapists were able to provide intervention is commendable and is witness to their holistic skills, but this does not provide a satisfactory solution to reducing the increasing effects of low back pain. Essentially a biopsychosocial assessment at an earlier stage of pain, at less than three months duration, would go some way to reducing the prevalence of debilitating low back pain reported (Buchbinder, et al., 2001, Waddell et al., 1999). Occupational therapists with their experience in occupational performance would be well qualified to contribute, if not organise, the service. Holistic Approach Both samples emphasised the holistic approach of occupational therapists to assessment and intervention. This was the strength of the therapists as they offered physical, emotional and social support to enable patients to deal with the overall effects of their back pain. This had already been identified, as part of the occupational therapy role (O’Hara, 1996, Strong, 1996, McCormack, 1990) in chronic pain, and occupational therapists will recognise the ethos of the occupational therapy philosophy. All therapists had an understanding of the nature of chronic pain and therefore understood that patients were able to function physically, emotionally and socially with their pain to minimise their disability. Concerns of Occupational Therapists Ten of the survey respondents identified the need for further training in chronic low back pain, and the interviews revealed that there was an interest in the evolution of pain management and the relevant interventions. One therapist interviewed identified occupational therapists as the ideal interventionist or leader in this field due to their specific skills. A lack of services was a concern, as well as a lack of structure and time, to offer a more comprehensive assessment and intervention. 50 Independence/Empowerment Taylor’s (2001) study evidenced undergraduates’ understanding of patient choice to be involved in decisions concerning their own intervention towards empowerment. Therapists were equally aware that patients are capable of deciding their own goals, and this is what motivates them to move forward. Returning to O’Hara’s (1996) theme of only providing aids and adaptations for the patient if they want them, emphasises the importance of the inclusion of patients in the preparation of their own treatment plans. This empowerment was reported in the progress and effects of assessment and intervention in the survey, as generally patients seemed more in control of their condition, as they were exploring community opportunities and adapting their approach, while reducing the passive role. The Literature Review To date, no studies have been found about the experiences of occupational therapists working with patients with chronic low back pain in primary care. However there were some comparisons in the roles described in the literature (Strong, 1996, O’Hara, 1996, Baptiste, 1988, Giles & Allen, 1986). There has been some debate about the role of a literature review in phenomenological research. Provided it is delayed until after data generation to bracket information, it has been acknowledged as an integral part of a study (Lowes, Prowse, 2001). Conversely a comprehensive literature search can detract from an exploratory study (Sim, Wright, 2000). In this study the literature search highlighted the paucity of evidence and stimulated the research (Lowes, Prowse, 2001). Methodology 51 Crotty’s (1996) five step process proved a suitable format for this study. He had recognised (1998) that modern phenomenology research is more a study of the subjective experience, and that there has been misuse and misunderstanding of the philosophical underpinnings. Originally designed as a theory and philosophy (Sim, Wright, 2000), phenomenology had no basic guidelines for research practice (Finlay, 1999). This study relied on a secondary source for a formula and discussion was based on the theorising of other secondary sources. Purism is a challenge in the evolving nature of qualitative research (Finlay, 1999, Crotty, 1996), but appraisal of philosophical underpinnings has been advised (Finlay, 1999, Seymour & Clark, 1998, Koch, 1995). This study favoured a basic theory (Hammell, (2002), Shepherd et al.,1993) to discover the suitability of the framework in practice (Finlay, 1999). Briefly Crotty’s (1996) process was interpreted as: 1) The phenomenon was the therapists who worked with chronic low back pain. 2) The experiences were described in the telephone interviews and reinforced by the open question responses of the survey. The interviewer kept a reflective diary and debriefed with her peers. 3) The interviews were scribed by an independent clerk. 4) The texts were member checked by the participants and the clinical supervisor verified them. 5) The researcher was dependent on the integrity of the participants and reflexivity to establish trustworthiness in the study, and reported a clear audit trail for the data. The researcher acknowledged that Crotty’s framework was conducive to her study from the outset (Shepherd et al., 1993), although it would not necessarily be appropriate for all studies. A more experienced researcher may have been more confident to let the study flow in a less structured way towards greater maximisation 52 of the data, but there was a desire to get it right. The aim of the study was to remain faithful to the meanings and intentions of the participants (Walker et al., 1999), and the structure facilitated trustworthiness. Design The exploratory design elaborated the experiences of occupational therapists. The method was responsive to the phenomenon and the researcher continually engaged in a dialectical analysis to evaluate the effect of her subjectivity on the research (Finlay, 1999), while mistakes were acknowledged and evaluated (Savin-Baden & Fisher, 2002). Richer data than anticipated emerged from the survey questionnaire (Sim, Wright, 2000, Polit & Hungler, 1997). Storing the collated and analysed survey data before the interview (Polit & Hungler, 1997) contributed to trustworthiness as well as improving the quality of the data to answer the research question. Sample Personal identification of the sample was unnecessary for the study but the researcher needed to know where the sample had come from (Corben, 1999), to assure the credibility of the findings. Primarily five therapists appeared a suitable number to manage due to the potentially lengthy nature of the data collection and analysis, in the time available. The response to the postal questionnaire provided the projected number of participants for interview, but there was no margin for dropout or extending the sample should the data be insufficient. Sample size gave a representative figure of the group concerned (Taylor, 2001, Polit & Hungler, 1997), and the sample was relative to the phenomenon to be researched (Sandelowski, 1995), as volume of data was gained from small numbers (Sim, Wright, 2000). However a larger choice for sample would have improved the potential for richer data. 53 It was a ‘purposive’ sample (Dawkins & May, 2002, Sim, Wright, 2000, Corben, 1999, Sandelowski, 1995), as all participants had direct personal experience and knowledge of patients with chronic low back pain. All five participants were enthusiastic, committed to their work, and more than willing to facilitate the researcher. A broader range of clinical grades may have provided a greater contrast of experience. Data collection The researcher was dependent on the data supplied by the sample, although there was no guarantee about the accuracy (Parahoo, 1997). Two collection tools prolonged the collection process. The survey was more prescriptive, as it relied on the validity and reliability of the questionnaire to elicit the direct responses and interpretations of the participants. It was also employed to identify a volunteer, purposive sample for interview (Ballinger & Davey, 1998, Foulder-Hughes, 1998). The open questions provided unpredicted additional information, which actually enhanced the credibility of the overall data. Storage of these results enabled the researcher to focus on the interview. The interview may have been lengthened or expanded by a more experienced interviewer. The Survey Questionnaire No existing survey was found for this study, but the pilot study confirmed the validity and reliability of the questionnaire design, and there was no reason to query this in the main study. The postal questionnaire accessed a larger group of therapists and was easier to administer (Ballinger & Davey, 1998), although the coding demanded vigilance to assure confidentiality of identity and data received. Vigilance was rewarded when a second mail shot went smoothly. The questionnaire had twenty six 54 questions and a few were only partially completed, whether due to the respondents’ knowledge of low back pain, waning interest (Walker, 1996, Ballinger & Davey, 1998), or lack of time, is not clear. The closed questions had a better response rate possibly because the responses were limited to epidemiological data or multiple choice questions. The majority of the completed questions fell at the beginning before interest or patience may have wavered, although McGibbon (1997) actually recommended that open questions be placed either in the middle or the last quarter of the questionnaire. A shorter questionnaire would have failed to elaborate on more than the aims of the study. Open questions often take longer to complete (McGibbon, 1997), as respondents have to think more carefully about their response. However the majority of informants reported a wealth of experiences, suggesting that the requirement was not over taxing. Closed questions on the same topics may have been constrained (Walker, 1996), and possibly biased, resulting in invalid description of real experiences. Employing an interview only for experiences of occupational therapists, while employing the survey only for demographic information and selection of a sample for interview would have ignored the opportunity to improve trustworthiness through triangulation. The first questionnaires were despatched during the summer months when therapists may have been on vacation, although the follow up elicited fewer replies. Recipients have choices, and response rates are always unpredictable. However the spasmodic return of the questionnaire facilitated an organised recording system. There was no explanation for the dearth of responses from therapists in Trust hospital departments. Many therapists work single-handed in rural areas and time is precious. The change in health care structure to Local Health Boards in April 2003 has enforced reorganisation, and lists of therapists may have been incomplete. Observation of 55 colleagues suggests that questionnaire responses depend on their clinical commitments at the time of receipt. The Telephone Interview Each interview was a unique interaction which was not replicable (Parahoo, 1997) and was a reflective process for researcher and participant (Finlay, 1999). The dialogue yielded mainly conversation to elaborate the data, not just question and answer. The researcher was concerned to allow the participant to take the lead (Parahoo, 1997). Two short interviews may have been influenced by clinicians taking their interventions for granted (Guidetti & Tham, 2002), and failure of the researcher to interject appropriately (Hand, 2003), as well as an unexpected problem with the equipment in the first interview. Interviews of less than thirty minutes may not actually get beyond the civilities (Parahoo, 1997). The formalities had been discussed when arranging the telephone interview and the scribed texts suggested that the introductory question opened up the interviews straight away. Extra trigger words on the interview schedule would have facilitated the researcher’s probing skills as would prior experience and practice in this type of interviewing. A pilot study would have highlighted these issues and is recommended for future study. Semi-structured telephone interviews encouraged the participant free expression while putting them at their ease. Selected topics on the interview schedule helped to keep the sessions on track as some structure and rapport was essential (Sim, Wright, 2000, Parahoo, 1997). Verbal rapport was enhanced as participants settled into the discussion, while body language and physical presentation had no influence, enabling the researcher to focus on the content of the interchange. The researcher was tempted to join in discussion using her own experiences, but the reflective diary evidenced that her expectations were based on her therapeutic environment. Three 56 of the interviews concluded on a less formal note, exchanging views on professional issues. This indicated a co-participation of researcher and participant towards a greater understanding of the phenomenon (Lowes, Prowse, 2001). In retrospect, the employment of an external observer to report on the researcher’s interview style may have contributed to reflexivity. The experience of the researcher was enhanced by practice. Although she is an experienced counsellor and therapist, interviewing for research was a new venture until she realised that it did not have to be significantly different. She was able to bring interviewees back on track by focussing on the subject for debate. Versatility and flexibility were essential but the process was not always easy to assess during the interview (Parahoo, 1997). The scripts of the member checked texts gave a clearer account of the process, and clarified the researcher’s description of her approach. Data analysis This was a lengthy and time consuming process due to the quantity and quality of the data collected. Interpretation was the sole responsibility of the researcher and had to be her interpretation alone. The experience of the survey analysis proved helpful when it came to analysing the interview data. Longer interviews, although desirable for richer data, may have impeded completion to date and the analyst was learning the job. A personalised method proved more productive and expansive. Adhering to established approaches (Finlay, 1999) would have impeded the researcher’s process. The results emerged systematically, reflecting the perceptions of the participants (Bowman, 1994), emulating a phenomenological trait (Polit & Hungler, 1997). Contrary to expectation the author was not aware of engaging in self- 57 discussion or opining during the process, but focussed on the written data, which was absorbing and demanded a disciplined approach. Intuiting (Grbich, 1999, Polit & Hungler, 1997) was about being open to the participants’ point of view, but the reader has to rely on the interpretation of the analyst (Polit & Hungler). Objectivity during analysis was questioned (Lowes, Prowse, 2001), as the author wanted to work with the written data without distortion (Grbich, 1999). The early data came from the survey, and the phenomenological principles did not directly apply, but the compilation of the results was an individual interpretation and reduction of all the responses. In alternative circumstances the researcher would have emulated Foulder-Hughes (1998) and invited a colleague to explore the response categories independently, to improve rigour. Limitations The interview sample was a small group of senior grades only and was drawn from a small rural area. Although the participants had a varied clinical background they were not necessarily representative of the general population of occupational therapists working with chronic low back pain in primary care. Access to a larger potential sample and a more experienced interviewer may have elicited broader data. The participants verified the text, but the results relied on their reflections and accounts, as telephone interviews prevented observation of participants in action. Another researcher may have interpreted the themes differently (Henare et al., 2003), and the interpretations were dependent on the personal and professional integrity of the researcher to give as true an interpretation as possible. The account was somewhat reductionist (Finlay, 1997), as the analysis followed the same formula for survey and interview. The time constraints were always in consideration, but there was also the unfulfilled desire to further explore methodological discussion within the study. 58 Initially expectations of the outcome may have been biased and cautious, but acknowledging the qualitative clinical input of the participants dismissed this. Recording early expectations in the reflective diary at the outset and debriefing with peers facilitated objectivity, separating any personal expectations of the study from the experiences of the participants. This researcher acknowledged that there were inconsistencies in her study whilst recognising the experience she was gaining. Honest evaluation of her methods helped create a reflective learning process about the methodology and research design employed. Conclusions This study demonstrated a small competent experience of occupational therapists working in primary care with low back pain and identification of their expertise and interest is encouraging. The study found that there was no specialist occupational therapy input for this condition but there was: 1. Competent assessment and intervention for patients. 2. No knowledge of clinical guidelines. 3. A strong probability that therapists contributed to disability prevention 4. Multi-disciplinary working, but that did not discredit lone intervention. Those who were working with the client group were able to identify the debilitating effects of the condition and had the knowledge to facilitate patients to live with the pain, by adopting physical and emotional strategies. Their input was often limited because of the demands of their more general caseload. Due to the statistical evidence on the prevalence of low back pain there would seem to be a need for more specific services to reduce the statistics. Based on the findings of this initial study it would seem that occupational therapists are qualified to intervene with these patients, employing their holistic and occupational performance expertise, and that full use should be made of their expertise. Occupational therapists are requested to 59 reflect on this small study to consider the future of occupational therapy and low back pain in primary care. Recommendations Further exploration is required to explore the wider experiences and perspectives of occupational therapists to support these findings, and alert occupational therapists to their potential individual clinical input with chronic low back pain. Interviewing reliable patients with low back pain about their experiences of occupational therapy in primary care would provide the consumers’ point of view, and provide evidence to improve services to the increasing patient group. There is evidence that occupational therapists are particularly qualified to assess the effects of low back pain at an early stage, to prevent future disability and chronicity. Inclusion of occupational therapists in the working parties of clinical guidelines would exploit occupational therapy to a higher level, as it is already recognised by the Pain Society as an integral contributor of a multi-disciplinary pain management programme. Knowledge of clinical guidelines, would enable occupational therapists to recognise their skills to identify that low back pain can be alleviated through the practical problem solving approaches that demonstrate the full philosophy of occupational therapy. Most additional training had been at the therapists’ own instigation. Further opportunities and provision would heighten interest as well as improve basic skills. This study has heightened the researcher’s awareness, but more evidence is needed to heighten interest and enable occupational therapy practice with chronic low back pain in primary care. The provision of a National Framework for Pain, planned for the future, may go some way to heightening the awareness of not only occupational therapists, but other members of multi-disciplinary teams, and contribute to reducing the unnecessary effects of chronic low back pain. 60 REFERENCES Annells, M. (1999) Evaluating phenomenology: usefulness, quality and philosophical foundations Nurse Researcher. 6 (3): 5-19 Ballinger, C.& Davey, C. (1998) Designing a Questionnaire: an Overview British Journal of Occupational Therapy 61 (12): 547-550 Bandolier (1995) Back Pain 19-21 http://cymruweb.wales.nhs.uk/bandolier/E3126.htm October 2000 Baptiste, S. (1988) Muriel Driver Memorial Lecture Chronic Pain, Activity and Culture Canadian Journal of Occupational Therapy 55 (4): 179-184 Barbour, R. (2001) Checklists for improving rigour in qualitative research: a case of the tail wagging the dog British Medical Journal 322: 1115 -1117 Beck, CT. (1994) Phenomenology: its use in nursing research International Journal of Nursing Studies 31 (6): 499-510 Birkholz, M. Aylwyn, L. (2000) Occupational Therapy in chronic pain management: a specialist area. Occupational Therapy News 8/11: 26 -27 Bowman, J. (1994) Experiencing the Chronic Pain Phenomenon: A Study. Rehabilitation Nursing 19 (2): 91-95 Brown, C A. (2002) Occupational Therapists’ beliefs regarding treatment options for people with chronic pain British Journal of Occupational Therapy 65 (9): 398-404 61 Buchbinder, R. Jolley, D. & Wyatt, M. (2001) Population based intervention to change back pain beliefs and disability; three part evaluation. British Medical Journal 322: 1516-1520 Butler, J. (2003) Research in the workplace – some ethical issues Occupational Therapy News June: 16 (abridged article first published in the Bulletin of Medical Ethics 2003. 185. pp 21-3 and appears with permission from the editor, Dr. Richard Nicholson) Carruthers, C. (1997) Developing a pain management programme British Journal of Occupational Therapy 60 (5): 221-222 Carruthers, C. Madeley, D. (1997) Chronic Pain Management: response Letter British Journal of Occupational Therapy 60 (7): 331-332 Chesney, A B. Brorsen, N E. (2000) Occupational therapist’s role in managing chronic pain. Occupational Therapy Practice 5 (20): 10-13 Clinical Standards Advisory Group (1994) Back Pain: Report of a CSAG committee on back pain London: HMSO College of Occupational Therapists (2003) Research Ethics Professional Standards for Occupational Therapy Standards Conneeley, L. (2002) Methodological Issues in Qualitative Research for the Researcher Practitioner British Journal of Occupational Therapy 65 (4): 185-190 62 Corben, V. (1999) Misusing phenomenology in nursing research: identifying the issues Nurse Researcher 6 (3): 52-66 Croft, PR. Macfarlane, GJ. Papageorgiou, AC. Thomas, C. Silman, A. (1998) Outcome of low back pain in general practice: a prospective study British Medical Journal 316: 1356-1359 Crotty, M. (1998) The Foundations of Social Research. Meaning and Perspective in the Research Process London: Sage Crotty, M. (1996) Phenomenology and Nursing Research Melbourne: Churchill Livingstone Curtin, M. & Jaramazovic, E. (2001) Occupational Therapists’ Views and Perceptions of Evidence Based Practice British Journal of Occupational Therapy 64 (5): 214-222 Davis, A. (1996) Primary care management of chronic musculoskeletal pain Nurse Practitioner 21 (8): 72-82 Dawkins, Helen & May, Esther (2002) The lived experience of doing a higher degree in Occupational Therapy from the perspective of the graduate: A phenomenological study Australian Occupational Therapy Journal 49: 128-137 Finlay, L. (2000) Multiple Voices, Multiple Paths: Choosing between Qualitative Traditions British Journal of Occupational Therapy 63 (12): 580-582 Finlay, L. (1999) Applying phenomenology in research: problems, principles and practice British Journal of Occupational Therapy 62 (7): 299-305 63 Finlay, L. (1998) Reflexivity: an essential component for all research? British Journal of Occupational Therapy 61 (10): 453-456 Finlay, L. (1997) Good patients and bad patients: how Occupational Therapists view patients/clients British Journal of Occupational Therapy 60 (10): 440-446 Fisher, A. & Savin-Baden, M. (2001) The Benefits of Young People Experiencing Psychosis and their Families, of an Early Intervention Programme: Evaluating a Service from the Consumers’ and the Providers’ Perspective British Journal of Occupational Therapy 64 (2): 58-65 Flower, A. Naxon, E. Jones, RE. Mooney, V. (1981) An occupational therapy programme for chronic back pain American Journal of Occupational Therapy 35 (4): 243-248 Foulder-Hughes, L. (1998) The Educational Needs of Occupational Therapists Who Work With Adult Survivors of Childhood Sexual Abuse British Journal of Occupational Therapy 62 (2): 68-74 Frost, M. Gough, M. Hafner, C. Hine, I. & Lode, Y. (2001) How useful is the Welsh Inpatient Pain Management Centre? Unpublished Internal Report Gaynord, B. (1996) Case studies: Primary care occupational therapy: Paula and Jack British Journal of Therapy and Rehabilitation 3 (7): 386-388 Gibson, L & Strong, J. (1998) Assessment of psychosocial factors in functional capacity evaluation of clients with Chronic Back Pain British Journal of Occupational Therapy 61 (9): 399-404 64 Giles, GM. Allen, ME. (1986) Occupational therapy in the treatment of the patient with chronic pain British Journal of Occupational Therapy Jan: 4-8 Gough, M. & Frost, M. (1996) Should Multi-disciplinary Pain Management Programmes Attempt to Reduce Self-Reported Pain in Patients with Chronic Back Pain? The Experience of a Welsh Inpatient Programme British Journal of Occupational Therapy 59 (9): 411-414 Grbich, C. (1999) Qualitative Research in Health London: Sage Publications Guidetti, Susanne. Tham, Kerstin. (2002) Therapeutic strategies used by occupational therapists in self-care training: A qualitative study Occupational Therapy International 9 (4): 257-276 Hafner, CD. (1999) Do health professionals, through their information giving, contribute towards chronicity and disability in-patients with low back pain? Unpublished Dissertation submitted for the degree of MSc in Pain Management. Hammell, KW. (2002) Informing Client-Centred Practice through Qualitative Inquiry: Evaluating the Quality of Qualitative Research British Journal of Occupational Therapy 65 (4): 175-184 Hand, H. (2003) The mentor’s tale: a reflexive account of semi-structured interviews Nurse Researcher 10 (3): 15-27 Heck, S. (1987) The effect of purposeful activity on pain tolerance American Journal of Occupational Therapy 42 (9): 577-581 65 Helm, T. Dickerson, AE, (1995) The effect of hand therapy on a patient with Colles Fracture: A phenomenological study Occupational Therapy in Health Care 9 (4): 6977 Henare, D. Hocking, C. Smythe, L. (2003) Chronic Pain: Gaining understanding through the use of art British Journal of Occupational Therapy 66 (11): 511-518 Jones, D. Ravey, J. Steedman, W. (2002) Developing a measure of beliefs and attitudes about chronic non malignant pain: A pilot study of occupational therapists Occupational Therapy International 7 (4): 232-245 Kelly, G. (1996) Understanding Occupational Therapy: a Hermeneutic Approach British Journal of Occupational Therapy 59 (5): 237-242 Koch, T. Harrington, A. (1998) Reconceptualising rigour: the case for reflexivity Journal of Advanced Nursing 28 (4): 882-890 Koch,T. (1995) Interpretive approaches in nursing research: the influence of Husserl and Heidegger Journal of Advanced Nursing 21: 827-836 Koes, BW. van Tulder, M W. Ostelo, R. Burton, K A. Waddell, G. (2001) Clinical guidelines for the management of low back pain in primary care: an international comparison Spine 1 (26): 2504 - 13 Krefting, L. (1991) Rigor in Qualitative Research: The Assessment of Trustworthiness The American Journal of Occupational Therapy 45 (3): 214-222 66 Little, P,.Smith, L. Cantrel,l T. Chapman, J. Langridge, J. Pickering, R. (1996) General practitioners’ management of acute back pain: a survey of reported practice compared with clinical guidelines British Medical Journal 312: 485-488 Lowes, L. Prowse, Morag A. (2001) Standing outside the interview process? The illusion of objectivity in phenomenological data generation International Journal of Nursing Studies 38: 471-480 Mays, N. Pope, C. (2000) Assessing quality in qualitative research British Medical Journal 320: 50-52 Mays, N. Pope, C. (1995) Qualitative Research: Rigor and qualitative research British Medical Journal 311: 109-112 McCormack, G. (1990) Psychophysiologic theories of pain and implications for treatment Occupational Therapy Practice 1 (3): 1-10 McCormack, G. (1988) Pain management for occupational therapists American Journal of Occupational Therapy 42 (9): 582-590 McGibbon, G. (1997) How to avoid the pitfalls of questionnaire design Nursing Times 93 (19): 49-51 Moran, M. & Strong, J. (1995) Outcomes of a Rehabilitation Programme for Patients with Chronic Back Pain British Journal of Occupational Therapy 58 (10): 435-438 Newton, R. Scott, C. Edwards, C. Staniszewska, S. & Crombie, V. (1999) Services for Patients with Pain Clinical Standards Advisory Group. Department of Health. 67 NICE (2003) Acute Low Back Pain – Referral – Practice – Version Under Pilot http://www.nice.org.uk/article.asp?a=10554 (September, 2003) O’Hara, P. (1996) Pain Management for Health Professionals London: Chapman & Hall. Palmer, K T. Walsh, K. Bendall, H. Cooper, C. Coggin, D. (2000) Back pain in Britain: comparison of two prevalence surveys at an interval of 10 years British Medical Journal 320: 1577-1578 Parahoo, K. (1997) Nursing Research. Principles, Process and Issues Basingstoke: Macmillan. Pearce, S. Richardson, A. (1996) Fatigue in cancer: a phenomenological perspective European Journal of Cancer Care 5: 111-115 Polit, D F & Hungler, B P. (1997) Essentials of Nursing Research Methods, Appraisal and Utilisation Fourth Edition New York: Lippincott Pope, C. Ziebland, S. Mays, N. (2000) Qualitative research in health care Analysing qualitative data British Medical Journal 320: 114-116 Racher, F. (2003) Using conjoint interviews to research the lived experience of elderly rural couples Nurse Researcher 10 (3): 60-71 Reynolds, Frances (2003) Exploring the meanings of artistic occupation for women living with chronic illness: a comparison 68 of template and interpretative phenomenological approaches to analysis British Journal of Occupational Therapy 66 (12): 551-558 Reynolds, Frances & Prior, Sarah (2003) ‘A lifestyle coat-hanger’: a phenomenological study of the meanings of artwork for women coping with chronic illness and disability Disability and Rehabilitation 25 (14): 785-794 Royal College of General Practitioners (1999). Clinical Guidelines for the Management of Acute Low Back Pain London, Royal College of General Practitioners Sandelowski, M. (1995) Sample size in qualitative research Research in Nursing and Health 18: 179-83 Savin-Baden, M. & Fisher, A. (2002) Negotiating ‘Honesties’ in the Research Process British Journal of Occupational Therapy 65 (4): 191-193 Schroder, N. Merrill, J. Crabtree, J. Lyall-Watson, S. (2002) British Journal of Occupational Therapy 65 (2): 75-80 Seale, JK,.Barnard, S. (1999) Ethical considerations in therapy research British Journal of Occupational Therapy 62 (8): 371-375 Seymour, J. & Clark, D. (1998) Phenomenological approaches to palliative care research Palliative Medicine 12: 127-131 69 Shannon, E. (2002) Reflections on clinical practice by occupational therapists working in multi-disciplinary pain management programmes in the UK and the USA Australian Journal of Occupational Therapy 49: 48-52 Sheperd, KF. Jensen, GM. Schmoll, BJ. Hack, L. Gwyer, J. (1993) Alternative Approaches to Research in Physical Therapy: Positivism and Phenomenology Physical Therapy 73 (2): 88-101 Silverman, D. (1993) Interpreting Qualitative Data Sage London Sim, J. Wright, C. (2000) Research in Health Care Cheltenham: Nelson Thornes. Steuart-Corry, L. Dear, J. & Lattimore, E. (1997) Chronic Pain Management Programmes Letter. British Journal of Occupational Therapy 60 (7):331 Strong, J. Tooth, L. Unruh, A. (1999) Knowledge about pain among newly graduated occupational therapists: Relevance for curriculum development Canadian Journal of Occupational Therapy 66 (5): 221-228 Strong, J. (1998) Incorporating Cognitive Behaviour Therapy with occupational therapy: a comparative study with patients with LBP Journal of Occupational Rehabilitation 8 (1): 61-71 Strong, J. (1996) Chronic Pain The Occupational Therapist’s Perspective New York: Churchill Livingstone Strong, J. (1987) Chronic pain management: the occupational therapist’s role British Journal of Occupational Therapy 50 ((8): 262-3 70 Taylor, CM. (2001) Independence and Empowerment: Evidence from the Student Perspective British Journal of Occupational Therapy 64 (5): 245-251 Taylor CM (2000) Evidence Based Practice for Occupational Therapists Oxford: Blackwell Science The Royal College of Anaesthetists and the Pain Society (2003) Pain Management Services Good Practice The Pain Society (1997a) Desirable Criteria for Pain Management Programmes The Pain Society (1997b) Provision of Pain Services Thomas, E. Silman, Alan J, Croft, Peter R. Papageorgiou, Ann C. Jayson, Malcolm I V. Macfarlane, Gary J. (1999) Predicting who develops chronic low back pain in primary care: a prospective study British Medical Journal 318: 1662-1667 Tryssenaar, J. (1999) The Lived Experience of Becoming an Occupational Therapist British Journal of Occupational Therapy 62 (3): 107-112 Turner, A. (1996) Educational and behavioural interventions for back pain in primary care Spine 21 (24): 2851-2859 Udell, L. & Chandler, C. (2000) The role of the Occupational Therapist in addressing the spiritual needs of clients British Journal of Occupational Therapy 63 (10): 489494 71 Unruh, AM. Strong, J. Wright, A. 2002 Chapter 1 Introduction to Pain in Strong, J. Unruh, AM. Wright, A. Baxter, GD eds (2002) Pain A Textbook for Therapists Edinburgh: Churchill Livingston Van Tulder, MW. Ostelo, RWJG. Vlaeyen, JWS. Linton, SJ. Assendelft, WJJ. (2000) Behavioural treatment for chronic low back pain Cochrane Library Waddell, G. McIntosh, A. Hutchinson, A. Feder, G. Lewis. M, (1999) Low Back Pain Evidence Review London: Royal College of General Practitioners Waddell, G. (1987) A new clinical model for the treatment of low back pain Spine 12 (17): 632-644 Walker, EM. (1996) Questionnaire design in practice British Journal of Therapy and Rehabilitation 3 (4): 229-233 Wall, Patrick D, Melzack, Ronald (Eds) (1999) Textbook of Pain (4th ed) Edinburgh: Churchill Livingstone Williams, A,C de C. Richardson, P.H. Nichols, H.K. Pither, C.E. Harding, V.R. Ridout, K.L. Ralphs, J.A. Richardson, I.H. Justins, D.H. & Chamberlain, J.H. (1996) Inpatient vs. outpatient pain management: results of a randomised controlled trial Pain 66: 1222 72