SUPPLIMENTARY 1 Blood Flow Model Estimation of Blood Flow
advertisement

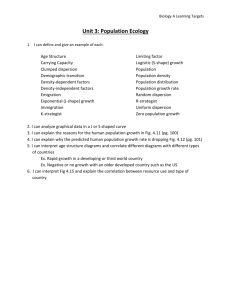
SUPPLIMENTARY 1 Blood Flow Model Estimation of Blood Flow and VT using [15O]-water PET is based on a single tissue compartmental model [1] where the rate of change in the concentration of tracer in the tissue at time (t) is given by: (dCT(t)/dt = K1CA(t) – k2CT(t) (1) Where CA(t) and CT(t) are the concentration time courses of radioactivity in arterial blood and tissue respectively. K1 equals flow (F) multiplied by the extraction fraction for water (E), which in turn is a function of F and the permeability surface product (PS), as given by the Renkin-Crone equation: K1 = E*F = (1 - e-PS/F)*F (2) As [15O] water is freely diffusible, PS is much greater than F. Hence, in [15O] water PET studies, K1 is flow limited. Equation 1 may then be re-written: dCT(t)/dt = FCA(t) – (F/VT)CT(t) (3) where VT is the distribution volume of water, corresponding to the equilibrium partition coefficient of water between blood and tissue. This then gives a solution: CT(t) =Fexp(-(F/VT)t) CA(t) (4) Where denotes convolution. A correction for the tissue blood volume fraction(vb) can be incorporated into equation 4. The form of the correction depends on whether the arterial input function is derived from the image (IDIF), in which case [2]: CT(t) =(1-vb)Fexp(-(F/VT)t) CA(t) + vb.CA(t) (5) It is very important to note that a large apparent blood volume term can also arise in the operational equation when the arterial blood is measured on-line, due to dispersion of the blood in the cannula, and that failure to take this into account leads to large errors in the estimated blood flow. When arterial blood is sampled continuously from an indwelling cannula, there are delay and dispersion effects dependent on the length of the cannula. The input function can be shifted in time with decay correction to account for the delay. Dispersion is usually modelled as a convolution of the ‘true’ input curve (CA(t)) with an exponential ‘smear’ (exp(-t/d)) to give the measured blood time activity curve (CM(t)). Incorporation of delay and dispersion effects into equation 4, replacing CA(t) with CM(t), gives the operational equation CT(t) = (F.d).CM(t) + F(1-( F.d)/VT) )exp(-(F/VT)t) CM(t) Where d is the dispersion time constant. This model of dispersion therefore gives rise to an additional ‘pseudo’ tissue blood volume term (F.d). This can often be estimated when fitting ROI data. Alternatively a standard dispersion correction can be applied. In any case this draws attention to a need to keep the cannula as short as possible and with a fixed distance between the arterial sampling point (e.g. wrist) and the in line detector loop. Measuring blood volume directly It is possible to measure blood volume in tumours directly using 11 C or 15 O labelled Carbon Monoxide [3]. Most such studies have, however, been carried out in normal brain tissue in conjunction with 15O-water and 15O2 to study oxygen metabolism. Labelled Carbon Monoxide strictly measures red cell volume, so the ratio of tissue to large vessel haematocrit may vary. Measuring the distribution volume of water There are a variety of ways of fitting PET data to these operational equations, either at the voxel level or in regions of interest [2]. For studies of normal healthy tissue, e.g. brain, the assumption of a fixed value of VT allows for a very simple quantitative ‘autoradiographic’ or basis function approaches. However, for tumours, estimation of both F and VT in regions of interest using a nonlinear least squares fit of the full model to the measured tissue timeactivity curves gives valuable extra information. e.g. Breast tumours have relatively high and variable fat content, so tend to have lower VT values [4], as the hydrophobic nature of fat reduces [15O] water accessibility. It has also been suggested that fibrosis, necrosis, occlusion of vessels or increased intercapillary distance may decrease tumour VT values [2, 5]. Tumour perfusion can be modulated by anti-vascular agents or anti-angiogenic agents. Perfusion can be readily calculated from a [15O] water PET study and used to evaluate the efficacy of an experimental agent; in a phase I setting, these data can be used to optimise the drug dose and/or schedule. Perfusion data can also be used in early phase studies identify non-responders at an early phase in the treatment cycle. Changes in VT values during a serial study may also be useful for demonstrating the efficacy of some experimental therapeutics; anti-vascular agents but not anti-angiogenic therapies, are expected to decrease VT values due to increased necrosis or increased intercapillary distance [2]. In contrast, [15O] water PET does not measure vascular permeability, so can not be used to study how this parameter is affected by drugs such as bevacizumab[6]. REFERENCES 1. KETY SS (1951) The theory and applications of the exchange of inert gas at the lungs. Pharmacol Rev 3:1-41 2. De Langen AJ, Van Den Boogaart VEM, Marcus JT, Lubberink M (2008) Use of H2 15OPET and DCE-MRI to measure tumor blood flow. Oncologist 13:631-644 3. Lammertsma AA, Frackowiak RSJ, Hoffman JM et al (1989) The C15O2 build-up technique to measure regional cerebral blood flow and volume of distribution of water. Journal of Cerebral Blood Flow and Metabolism 9:461-470 4. Wilson CBJH, Lammertsma AA, McKenzie CG, Sikora K, Jones T (1992) Measurements of blood flow and exchanging water space in breast tumors using positron emission tomography: A rapid and noninvasive dynamic method. Cancer Res 52:1592-1597 5. Laking GR, Price PM (2003) Positron emission tomographic imaging of angiogenesis and vascular function. Br J Radiol 76:S50-S59 6. Willett CG, Boucher Y, Di Tomaso E et al (2004) Direct evidence that the VEGF-specific antibody bevacizumab has antivascular effects in human rectal cancer. Nat Med 10:145-147