PHT 453 Practical Notes
advertisement

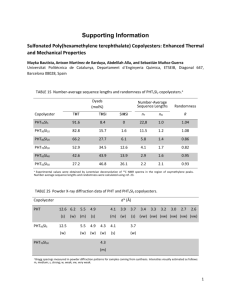
بسمة الدوسري.أ PHT 453 laboratory PHT 453 practical notes Lab. #1 Preparations : 1. chloramphenicol suspension ------------------ 25 ml 2. paracetamol elixir ------------------------------- 50 ml SUSPENSIONS suspensions : are dispersions of finely divided insoluble material (the dispersed phase ) which is randomly distributed into the liquid medium ( the continueous phase ) . they can be classified into : Coarse susp. : when particles size is larger than 1 mM in diameter. Colloidal susp. : when particles size is less than 1 mM in diameter. Suspensions can be used either internally or externally. Oral suspensions are liquids containing one or more active ingredients suspended in a suitable vehicle. Suspended solids may slowly separate on standing but easily redispersed by simple shaking. CHLORAMPHENICOL SUSPENSION U.S.P. Rx *F Chloramphenicol palmitate Glycerin Arabic gum ( acacia ) Favouring agent Simple syrup Water to Fiat : susp. Mitte: 25 ml Sig. : 1 tsp q 6 hrs. N.B. : sp. Gr. Of glycerine = 1.25 sp. Gr. Of simple syrup =1.3 4g 20 g 10 g q.s. 50 g 100 ml 1g 5 g = 4 ml 2.5 g q.s. 12.5 g = 9.6 ml 25 ml Calculations : F = 25/100 = 0.25 Volume of glycerin = 5 / 1.25 = 4 ml Volume of syrup = 12.5 / 1.3 =9.6 ml Amount of vehicle = 25 – (4 + 9.6 ) = 11.4 ml of water Procedure: 1. triturate Chloramphenicol palmitate with Glycerin and acacia in a mortar to give a smooth pourable paste. 2. dilute the paste with simple syrup ( 5ml ) , mix. 1 بسمة الدوسري.أ PHT 453 laboratory 3. transfere to a cylinder , then add the rest amount of the syrup and add the flavor. 4. complete to volume with water. 5. transfere to a clean bottle and fix a white label. Label : White Shake The Bottle Before Use Chloramphenicol Palmitate Suspension One teaspoonful to be taken every six hours Name: Date: Uses: 1. Chloramphenicol is a broad spectrum antibiotic which is effective against both gram +ve and gram –ve organisms. 2. palmitate ester is used in the susp. ( NOT succinate ) because : a. palmitate is insoluble for oral suspensions. b. Succinate is water soluble which form a clear solution , so it can be used in injections. c. Palmitate aster is more palatable than succinate. 3. glycerin : a wetting agent. 4. acacia : a suspending agent. 5. syrup : a sweetening agent. 6. water : a vehicle. Dose : Chloramphenicol wether administered by mouth or IV it is given for adults as 50 – 100 mg / Kg / day in 4 divided doses( every six hours ), depending on the seriousness of the infection and sensitivity of bacteria. --------------------------------------------------------------------------------------------------- ELIXIRS: ELIXIRS: are aromatic liquid preparations which form a convwnient mean of administering potent or nauseous medicaments in a palatable form and in a small dose- volumes . the solvent frequently contains a high proportion of alcohol and / or syrup with or without glycerin. PARACETAMOL ELIXIR ( Martindale 28 th , p. 33 ) Rx paracetamol ethanol (90%) propylene glycol water glycerin to Fiat : elixir Mitte: 50 ml Sig. : 1 tsp qid x 4 / 7 prn. *F 120 mg 0.7 ml 0.5 ml 0.5 ml 5 ml 2 1200mg ( 1.2 g ) 7 ml 5 ml 5 ml 50 ml بسمة الدوسري.أ PHT 453 laboratory Calculations : F = 50 / 5 = 10 Vehicle ( glycerin ) = 50 – (7+5+5) = 33 ml Procedure: 1. in a small beaker , dissolve paracetamol in ethanol and propylene glycol. 2. add ½ amount of glycerin. Dissolve well using a glass rod. 3. transfer to a cylinder 4. add water , and mix. 5. complete to volume (50 ml ) with glycerin. 6. transfer to a clean bottle and fix a white label . Label : White Paracetamol Elixir One teaspoonful to be taken four times daily For four days when necessary. Name: Date: Dose : (120 mg / 5 ml) 2.5 – 5 ml ( for child up to 1 year) 5 – 10 ml ( for child 1-4 years). Uses: 1. Paracetamol is an analgesic and antipyretic used to relief mild to moderate pain. 2. ethanol : a solvent to dissolve paracetamol. 3. propylene glycol : a co-solvent. 4. glycerin: a co-solvent and a sweetening agent. --------------------------------------------------------------------------------------------------- 3 بسمة الدوسري.أ PHT 453 laboratory PHT 453 practical notes Lab # 2 ORAL EMULSIONS are liquids containing one or more active ingredients , they are stabilized oil- in – water dispersions , either or both phases of which may contain dissolved solids. Solids may also be suspended in oral emulsions. MINERAL OIL EMULSION (USP 23, P.1029 , Matindale 29 th, p.1322) Rx *F Mineral oil 500 ml Acacia (very fine powder) 125 g Syrup 100 ml Vanillin 40 mg Alcohol 60 ml Purified water to 1000 ml Fiat : oral emulsion Mitte: 25 ml Sig. : ½ fz BID x 3/7. 12.5 ml 3.125 g 2.5 ml 1 mg 1.5 ml 25 ml Calculations : F = 25/1000 = 0.025 Vehicle = 25 – (12.5+1.5+2.5) = 8.5 ml Procedure : 1. mix mineral oil with acacia in a dry mortar. 2. add 6 ml water all at once, and emulsify the mixture ( by strong ,rapid trituration using the pestle ) until a smooth, creamy mass which produce a clicking sound is obtained ( primary emulsion ). 3. dissolve vanillin in alcohol , then add to a mixture of syrup and 2 ml of water. 4. add the mixture in step # 3 to the emulsion formed in step #2. the addition should be gradual , in divided portions and trituration is performed after each addition. 5. transfere to a cylinder , and adjust to volume with water. Mix. 6. transfere to a clean dry bottle and fix a white label. N.B., vanillin may be replaced by not more than 1 % of any other flavouring agents. For a 100 ml emulsion, 6ml of sweet orange peel tincture, or 200 mg benzoic acid may be used as a preservative in place of alcohol. Label : White Shake Before Use Liquid Paraffin Oral Emulsion One tablespoonful to be taken two times daily for three days. Name: Date: 4 بسمة الدوسري.أ PHT 453 laboratory Uses: This emulsion is used as laxative. Liquid paraffin acts as a lubricant to keep the stools soft. It is employed in chronic constipation, especially in presence of hemorrhoids. The mixture should not be taken within 30 min. of meal times and preferably on an empty stomach. Role of each ingredient: 1. mineral oil : a laxative . 2. acacia : a natural emulsifying agent. 3. syrup: a sweetening agent. 4. vanillin: a sweetening and flavouring agent. 5. alcohol: to dissolve vanillin, preservative. Dose: Up to 45 ml is to be given daily , either in divided doses or at bed time. LIQID PARAFFIN ORAL EMULSION ( BP ,1980 ,p.559) Rx *F Liquid paraffin Vanillin Chloroform Benzoic acid solution Methyl cellulose 20 Saccharine sodium Water to Fiat : oral emulsion Mitte: 25 ml Sig. : ½ fz BID x 3/52. Calculations : F = 25/1000 = 0.025 Vehicle = 25 – (12.5+0.065+0.5) = 500 ml 500 mg 2.5 ml 20 ml 20 g 50 mg 1000 ml 12.5 ml 2.5 mg 0.065 ml 0.5 ml 0.5 g 1.25 mg 25 ml Procedure : 1. heat abut 8 ml of water until it boils, then sprinkle methyl cellulose on the surface and mix. Allow to stand for 30 min. to hydrate the powder . 2. add a sufficient water in the form of cold water (ice ) and stir mechanically until the mucilage is homogenous. 3. dissolve vanillin in a mixture of the benzoic acid solution and chloroform ( because it is more soluble in organic solvents). Add the solution to the mucilage and stir for 5 min. the small amount of Saccharine sodium may be dissolved in water then added to the mucilage. 4. to prepare the emulsion, add together equal volumes of liquid paraffin and the mucilage with constant stirring. ( or try to use a clean dry bottle and emulsify by shaking ). 5. fix a white label. Label : White Shake Before Use Liquid Paraffin Oral Emulsion One tablespoonful to be taken two times daily for three weeks. 5 بسمة الدوسري.أ PHT 453 laboratory Name: Date: Uses: This emulsion is used as laxative. The mixture should not be taken within 30 min. of meal times and preferably on an empty stomach. 1. liquid paraffin : a laxative . 2. vanillin: flavoring and sweetening agent. 3. chloroform: a preservative and a flavoring agent. 4. benzoic acid solution: a preservative. 5. methyl cellulose : an emulgent. 6. saccharine :a sweetening agent. Storage : Store in a cool place but do not allow to freeze. --------------------------------------------------------------------------------------------------- LINIMENTS Liniments are liquid or semi-liquid preparations which are intended for external application . They may contain substances possessing analgesic, soothing or stimulating properties. They should be applied to the intact skin and labeled with ‘ For External Use Only’. METHYL SALICYLATE LINIMENT ( BP 1980, P.681) Rx *F Methyl salicylate 25 ml Arachis oil to 100 ml Fiat :liniment Mitte: 25 ml Sig. : apply to the affected skin BID x 2/52. 6.25 ml 25 ml Calculations : F = 25/100 = 0.25 Vehicle (arachis oil) = 25 – 6.25 = 18.75 ml Procedure : 1. in a mortar, mix methyl salicylate with ½ amount of arachis oil . mix well using the pestle. 2. transfer to a cylinder, and complete to volume with the oil. 3. transfer to a clean bottle, fix a red label. Label : Red Shake Before Use Methyl Salicylate Liniment Apply to the affected skin two times daily for two weeks. Name: Date: 6 بسمة الدوسري.أ PHT 453 laboratory Uses: Methyl salicylate is absorbed through the skin and is applied in liniments or ointments to relief pain in rheumatic conditions. --------------------------------------------------------------------------------------------------- LINCTUSES Linctuses are viscous liquid preparations having demulcent, expectorant or sedative properties. They are given in doses of small volume to be swallowed slowly without the addition of water. They are usually used for the relief of cough. SIMPLE LINCTUS ( Martindalle 29 & 28 ,p. 1276) Rx Citric acid monohydrate Conc. Anise water Amaranth solution Syrup to Fiat :linctus Mitte: 50 ml Sig. : 1 fz swallowed slowly undiluted TID.. *F 125 mg 0.05 ml 0.1 ml 5 ml 1.25 g 0.5 ml 1 ml 50 ml Calculations : F = 50/5 = 10 Vehicle (syrup) = 50 –( 1+0.5 ) = 48.5 ml Procedure : 1. dissolve citric acid in about 20 ml of the syrup. 2. add the conc. Anise water & amaranth sol. 3. transfer to a cylinder, and complete to volume with the syrup. 4. transfer to a clean bottle, fix a white label. Label : White Simple Linctus One teaspoonful to be swallowed slowly undiluted three times daily. Name: Date: Uses: Demulcent. Role of each ingredient: 1. conc. Anise water: flavouring agent. 2. amaranth sol. : coloring agent. 3. syrup: a vehicle & sweetening agent. Dose: 5 – 10 ml . 7 بسمة الدوسري.أ PHT 453 laboratory simple linctus ( BP 1980, p.680): Rx Citric acid monohydrate Conc. Anise water Amaranth solution Chloroform spirit Syrup to 25 g 10 ml 15 ml 60 ml 1000 ml N.B. the BP formula is the same as martindale formula except for the presence of Chloroform spirit ( as a preservative & flavouring agent) in the BP prescription. --------------------------------------------------------------------------------------------------- 8 بسمة الدوسري.أ PHT 453 laboratory PHT 453 practical notes Lab # 3 LOTIONS: Lotions are liquid preparations intended for application to the skin. They may contain aqueous alcoholic or emulsified vehicles. They are applied without friction. They should be generally dispensed in coloured bottles , and the container labeled with ‘ For External Use Only’. PHENOLATED CALAMINE LOTION (BP,1988,P.702 + Marindale 28 th, p.491) Rx *F Calamine 150 g Zinc oxide 50 g Bentonite 30 g Sodium citrate 5g Liquefied phenol 5 ml Glycerol 50 ml Purified water to 1000 ml Fiat : lotion. Mitte: 100 ml Sig. : MDU. Calculations : F = 100/1000 = 0.1 Vehicle = 100 – (5+0.5) = 94.5 ml 15 g 5g 3g 0.5 g 0.5 ml 5 ml 100 ml Procedure : 1. dissolve sodium citrate in about ½ amount of water. 2. triturate calamine , zinc oxide and bentonite with the solution of sodium citrate. 3. add liq. Phenol and glycerol. 4. transfer to a cylinder and adjust to 100 ml with water. 5. transfer to a clean bottle and fix a red label. Label : Red Shake Well Before Use Phenolated Calamine Lotion To be used as directed. Name: Date: Uses: Calamine is mainly used as mild astringent, and protective and sooyhing for sunburns. Dose: It is applied topical to the skin , in various concentrations as a lotion or ointment. Role of each ingredient : 1. zinc oxide: astringent. 9 بسمة الدوسري.أ PHT 453 laboratory 2. 3. 4. 5. bentonite: dispersing agent. sodium citrate : anti-clotting agent. liq. Phenol: disinfectant. glycerol: humectant. N.B. : Calamine (BP) is a basic zinc carbonate with a small proportion of ferric oxide which give the pink or reddish – brown colour , while Calamine (USP) is zinc oxide with small proportions of ferric oxide. CALAMINE LOTION (USP ) Rx Calamine Zinc oxide Glycerin Bentonite magma Calcium hydroxide solution to 80 g 80 g 20 ml 250 ml 1000 ml Procedure: 1. in a beaker, dilute bentonite magma with an equal volume of calcium hydroxide sol. 2. in a mortar, mix calamine ,ZnO with glycerin. Then add a portion of the diluted magma triturating well until a smooth, uniform paste is formed. 3. incorporate the remainder of the diluted magma gradually. 4. transfere to a cylinder and complete to volume with calcium hydroxide sol. 5. transfere to a clean bottle. Fix a red label PHENOLATED CALAMINE LOTION (USP ) Rx Liquefied phenol Calamine lotion 10 ml 990 ml Procedure: Mix liq. Phenol with calamine lotion. Shake thoroughly before dispensing. --------------------------------------------------------------------------------------------------- 10 بسمة الدوسري.أ PHT 453 laboratory IODINE OINTMENT (BPC, 1949) Rx *F Iodine Potassium iodide Water Yellow simple ointment Fiat : ung. Mitte: 25 g Sig. : Ut.Dict. Calculations : F =25/100 = 0.25 4g 4g 4 ml 88 g 1g 1g 1 ml 22 g PREPARATION OF YELLOW SIMPLE OINTMENT (BP 1980, P.701) *F Wool fat 50 g 1.1 g Hard paraffin 50 g 1.1 g Cetostearyl alcohol 50 g 1.1 g Yellow soft paraffin 850 g 18.7 g Prepare 22 g. Calculations : F =22/1000 = 0.022 Rx Procedure : 1. in a porcelin dish, melt cetostearyl alcohol, hars paraffin, wool fat and yellow soft paraffin over a water bath. 2. when completely melted, discontinue heating and stir until the mixture begins to congeal. 3. powder iodine crystals in a glass mortar ( not too much) . 4. dissolve KI in water , then add iodine and dissolve. 5. incorporate the solution of iodine (in # 4 ) gradually into the ointment base prepared in step # 2. 6. transfer to a clean container and fix a red label . Label : Red Iodine Ointment To be used as directed. Name: Date: Uses: Iodine is a local antibacterial used for disinfecting the unbroken skin before operations. Iodine is also effective against fungi & protozoa. Role of each ingredient : 1. iodine : the active ingredient. 2. KI : aid in dissolving of iodine. --------------------------------------------------------------------------------------------------- 11 بسمة الدوسري.أ PHT 453 laboratory SULFUR OINTMENT ( BP 1980, p.701) Rx *F Precipitated sulfur 100 g Simple ointment 900 g Fiat :Ung. Mitte: 30 g Sig. : Ut.Dict Calculations : F =30/1000 = 0.03 3g 27 g PREPARATION OF SIMPLE OINTMENT: Rx *F Wool fat 50 g 1.35 g Hard paraffin 50 g 1.35 g Cetostearyl alcohol 50 g 1.35 g White soft paraffin 850 g 22.95 g Prepare 27 g. Calculations : F =27/1000 = 0.027 Procedure : 1. in a porcelin dish, melt cetostearyl alcohol, hard paraffin, wool fat and soft paraffin over a water bath . 2. remove from the heat and stir until cold. 3. powder ppt. Sulfur in a mortar , then incorporate with a portion of the simple ointment until smooth. 4. gradually add the remainder of simple ointment and mix thoroughly. 5. transfer to a clean container and fix a red label. Label : Red Sulfur Ointment 10% To be used as directed. Name: Date: Uses: Sulfur is a keratolytic and a mild antiseptic. It is widely employed in the form of lotions or ointments, in the treatment of acne, dandruff, seborrhoeic conditions and scabies. --------------------------------------------------------------------------------------------------- 12 بسمة الدوسري.أ PHT 453 laboratory PHT 453 practical notes Lab # 4 CREAMS Creams are semi-solid emulsions, which are intended for application to the skin. They usually consist of solutions or dispersions of one or more active ingredients in a suitable base. They may be water – miscible (o/w emulsions) described as aqueous creams or oil – miscible (w/o emulsions) described as oily creams. Creams should be kept and stored in well closed containers which prevent evaporation and kept below 25 oC. They should be labeled with “ For External Use Only”. ZINC AND ICHTHAMMOL CREAM (BP 1980,p.548 + Matindale 29th,p.936) Rx *F Ichthammol Cetostearyl alcohol Wool fat Zinc cream to Fiat : oily cream. Sig. : Ut.Dict. 50 g 30 g 100 g 1000g Mitte: 20 g 1g 0.6 g 2g 20 g Calculations : F =20/1000 = 0.02 Vehicle (zinc cream) = 20-(2+0.6+1) = 16.4 g Procedure : 1. in a porcelin dish, melt wool fat and cetostearyl alc. (use cetyl alc. Instead) over a water bath. 2. when completely melted, triturate and mix with the calculated amount of zinc cream. 3. incorporate ichthammol ,stir well. 4. transfere to a clean container and fix a red label . Label : Red Zinc and Ichthammol Cream To be used as directed. Name: Date: Uses: ichthammol is a local antibacterial used for treatment of skin disorders such as psoriasis, and promote healing of chronic inflammation. Dose : Topical to the skin as 5-10 % ointment or cream. 13 بسمة الدوسري.أ PHT 453 laboratory Storage: In cool place and well-closed containers which prevents evaporation and contamination. Role of each ingredient : 1. ichthammol: a slight bacteriostatic for treating of dermatitis and eczema. 2. zinc cream: mild astringent and protective . it is also widely employed in other official creams. ZINC CREAM (BP 1980,p.548) Rx Zinc oxide , finely sifted Calcium hydroxide Oleic acid Arachis oil Wool fat Purified water to Fiat : cream. Mitte: 25 g *F 320 g 0.45 g 5 ml 320 ml 80 g 1000 g 8g 0.01 g 0.125 ml 8 ml 2g 25 g Calculations : F =25/1000 = 0.025 Vehicle (water) = 25-(0.125+8) = 16.875 ml Procedure : 1. mix zinc oxide and calcium hydroxide. 2. triturate to a smooth paste with a mixture of oleic acid and arachis oil. 3. incorporate the wool fat. Stir well. 4. add gradually with stirring the calculated amount of water to make 25 g. 5. weigh the required amount (16.4 g) of the resulted zinc cream and use in the above prescription. Role of each ingredient : 1. zinc oxide : is applied externally as a mild astringent for the skin, and as a soothing and protective application in eczema . 2. arachis oil : emollient and soothing to inflamed surface , to soften skin in eczema and psoriasis. --------------------------------------------------------------------------------------------------- 14 بسمة الدوسري.أ PHT 453 laboratory OINTMENTS Ointments are semi-solid preparations consisting of a medicament or mixture of medicaments dissolved or dispersed in a suitable base. They are used as emollients or protective preparations on the skin. They are water-immiscible . Emulsifiable bases make the ointment miscible with tissue exudates and are more readily removable from the skin by washing. CETRIMIDE EMULSIFYING OINTMENT ( BP 1980,p.697 + Martindale 29th,p.954) Rx *F Cetrimide 30 g Cetostearyl alcohol 270 g Liquid paraffin 200 g White soft paraffin 500 g Fiat : oint. Mitte: 25 g Sig. : MDU. 0.75 g 6.75 g 5g 12.5 g Calculations : F =25/1000 = 0.025 Procedure : 1. in a porcelin dish, melt cetostearyl alc. (use cetyl alc. Instead) over a water bath. Then add white soft paraffin to melt. Finally, add liquid paraffin. 2. when completely melted, add cetrimide and stir well. 3. remove from water bath and stir until cold. 4. transfer to a clean container and fix a red label . Label : Red Cetrimide Emulsifying Ointment To be used as directed. Name: Date: Uses: Cetrimide is a quaternary ammonium ( cetyltrimethylammonium bromide) disinfectant. It is employed for cleansing the skin , wounds, and burns because of its bactericidal activity. It is mainly used as a cream containing 0.5% concentration. --------------------------------------------------------------------------------------------------- 15 بسمة الدوسري.أ PHT 453 laboratory PHT 453 practical notes Lab # 5 EYE OINTMENT These are prepared using aseptic techniques under conditions appropriate for the preparation of sterile products. The medicament is finely powdered , thoroughly levigated with small quantity of the sterile melted base, and then incorporated with the remainder of the base. The finished product is packed into sterile small collapsible tubes which must be free from dirt and metallic particles. ATROPINE SULFATE EYE OINTMENT 1% (BP 1980,p.690) Rx *F Atropine sulfate 1g 0.2 g Liquid paraffin 10 g 2g Wool fat 10 g 2g Yellow soft paraffin 80 g 16 g Fiat : ung. Mitte: 20 g Sig. : Ut.Dict Calculations : F =20/100 = 0.2 Procedure : 1. in a porcelin dish, melt yellow soft paraffin over a water bath. Then add wool fat to melt. Stir until liquefied. Finally, add liquid paraffin. 2. when completely melted, discontinue heating , stir until cold. 3. add atropine sulfate and stir the mixture until it begins to congeal. 4. pack into a suitable container and fix a red label . Label : Red Atropine Sulfate Eye Ointment To be used as directed. Name: Date: Uses: Atropine sulfate is used to: 1. dilate (enlarge) the pupil before eye examination. Dilatation of the pupil occurs in ½ to 1 hour following one local application and last for a week or more. 2. treatment of closed-angle glaucoma. Role of each ingredient: 1. liquid paraffin : used externally as an ophthalmic lubricant. 2. yellow soft paraffin: is used in eye ointments because the bleached white soft paraffin is irritant to the eye. Dose: It is applied topically into the conjunctival sac as 0.5-2% ointment , once for ophthalmic testing and 3 – 4 times a day for treating acute inflammation. --------------------------------------------------------------------------------------------------- 16 بسمة الدوسري.أ PHT 453 laboratory EYE DROPS Eye drops are aqueous or oily solutions or suspensions for instillation into the eye . They should be sterile and prepared under conditions appropriate for the preparation of sterile products (aseptic conditions). The method of sterilization is stated in each monograph. For aqueous solutions, water for injection should be used. Eye drops should be prepared in a vehicle which is bactericidal and fungicidal. They should be isotonic with lachrymal secretions (which is equivalent to 0.9% NS). Dropper plastic bottles are suitable for packing eye drops. Label should instruct the patint to discard the unused eye drops no longer than one month after opening the container. BENZALKONIUM CHLORIDE SOLUTION (Martindale 28th & 29th ,p.952) ( Hard contact lens solution ) or ( EDTA eye drops ) Rx *F benzalkonium chloride solution disodium edetate sodium chloride water for injection to Fiat :sol. Mitte: 20 ml Sig. : Ut.Dict 0.02 ml 50 mg 900 mg 100 ml 0.004 ml 10 mg 180 mg 20 ml Calculations : F =20/100 = 0.2 Procedure : 1. mix benzalkonium chloride solution , disodium edetate and sodium chloride in about 2/3 the amount of vehicle (water for injection). 2. transfere to a cylinder and complete to volume with WFI. 3. transfere into a suitable container and fix a red label . Label : Red benzalkonium Chloride Solution To be used as directed. Name: Date: Uses: Antiseptic with bactericidal and bacteriostatic activities. Role of each ingredient: 1. benzalkonium Chloride : active ingredient, preservative for some eye drops in 0.015 solutions, and antiseptic. 2. disodium edentate: inactivation of bacterial collagenase so it enhances the bactericidal activity of benzalkonium Chloride. 3. sodium chloride : to adjust isotonicity. 4. water: vehicle. Notes : 1. sterilized by autoclaving ( because it is an eye drop preparation). 17 بسمة الدوسري.أ PHT 453 laboratory 2. 3. 4. 5. 6. store in airtight containers, protect from light. it is incompatible with eye drops containing local anaesthetics. incompatible with some rubber containers (produce deposits). loss of activity when in contact with plastic materials ,e.g., polyvinyl chloride. loss of activity in presence of cotton. --------------------------------------------------------------------------------------------------- CHLORAMPHENICOL EYE DROPS (Martindale 28th & 29th ,p. 192) Rx *F Chloramphenicol Boric acid Borax Phenylmercuric nitrate Water for injection to Fiat :eye drops. Mitte: 20 ml Sig. : Ut.Dict 0.5 g 1.5 g 0.3 g 0.002 g 100 ml 0.1 g 0.3 g 0.06 g 0.0004 g 20 ml Calculations : F =20/100 = 0.2 Procedure : 1. dissolve Chloramphenicol, Boric acid, Borax, and Phenylmercuric nitrate in about 2/3 the amount of vehicle. 2. transfere to a cylinder and complete to volume with WFI. 3. transfere into a suitable container and fix a red label . Label : Red Chloramphenicol Eye Drops To be used as directed. Name: Date: Uses: Wide spectrum antibiotic used for the treatment of acute bacterial infection of the external eye. Role of each ingredient: 1. Boric acid and borax : to adjust the isotonicity. 2. Phenylmercuric nitrate: preservative. 3. water: vehicle. Notes : 1. sterilize by heating at 98 o to 100 oC for 30 min. 2. store in airtight containers, below 25 oC and used within three months. Storage at 2-8 oC prolong the shelf life to 12 months. 3. it should be protected from light. --------------------------------------------------------------------------------------------------- 18 بسمة الدوسري.أ PHT 453 laboratory PHT 453 practical notes Lab # 6 PASTES Pastes are solid preparations intended for external application . They usually contain a high proportion of medicaments which are not intended to be absorbed. ZINC GELATIN U.S.P. (USP+ Martindale 28th & 29th,p.936) “ UNNA,S PASTE “ Rx *F Zinc oxide, finely sifted 10 g 5g Gelatin sheets 15 g 7.5 g Glycerin 40 g 20 g Water 35 g 17.5 g , Fiat : Unna s paste . Mitte: 50 g Sig. : Ut.Dict N.B. sp.gr. of glycerin = 1.3 Calculations : F =50/100 = 0.5 Volume of glycerin = 20/1.3 = 15.4 ml. Procedure : 1. cut gelatin sheets into small pieces , after getting rid of the rigid edges. 2. weigh the amount of gelatin required and soak in water. Allow to stand for 15 min. 3. add ½ amount of glycerin to the soaked gelatin in a porcelin dish, and place the dish on water bath until all gelatin is well dissolved. 4. levigate zinc oxide in the remaining amount of glycerin, then add to the gelatin solution. 5. stir gently with a glass rod in cross-lines ( to avoid air entrapment) until a smooth gelly results and a drop of the solution becomes a line or a thread. 6. pour the paste while hot on a glass slide and allow to set and cool . 7. cut the paste into small pieces and pack in a suitable container. Fix a red label. Label : Red Zinc Gelatin USP To be used as directed. Name: Date: Uses: Zinc gelatin is used as a protective and supportive dressing for varicose ulcers. Role of each ingredient: Zinc oxide : a mild astringent and absorptive. Advice to patient when dispensed: 1. clean the leg or foot thoroughly. 2. apply a dusting powder ,e.g., talc powder. 3. the paste is previously melted and warmed. 4. apply the paste with a brush to the affected part. 5. cover the paste with a gauze bandage. 19 بسمة الدوسري.أ PHT 453 laboratory 6. apply another layer of the paste (until the third layer of bandage). 7. leave the dressing for three days to two weeks. 8. remove by soaking in warm water. Dose: It is applied externally , as an occlusive bandage ‘ dressing ’. Container: the preparation is divided into small pieces before packing in a jar so that the patient can melt an appropriate number for each treatment. Storage: Store in a cool place. Notes: 1. the paste should be free from air bubbles. 2. the paste should be smooth ‘ free from gritty particles of zinc oxide and particles of gelatin ‘. FORMULA OF THE BRITISH PHARMACOPEIA: ZINC GELATIN (BP) “ UNNA,S PASTE “ Rx *F Zinc oxide, finely sifted Gelatin sheets Glycerin Water 15 g 15 g 35 g 35 g 7.5 g 7.5 g 17.5 g 17.5 g --------------------------------------------------------------------------------------------------- COMPOUND BENZOIC ACID OINTMENT ( Whitfield,s ointment) (BP 1980 ,p.697) Rx *F Salicylic acid (fine powder) 30 g Benzoic acid (fine powder) 60 g Emulsifying ointment 910 g Fiat :Ung. Mitte: 25 g Sig. : Ut.Dict Calculations : F =25/1000 = 0.025 0.75 g 1.5 g 22.75 g PREPARATION OF EMULSIFUING OINTMENT: Rx *F Emulsifying wax 300 g 6.825 g White soft paraffin 500 g 11.375 g Liquid paraffin 200 g 4.55 g Prepare 22.75 g. Calculations : F =22.75/1000 = 0.02275 20 بسمة الدوسري.أ PHT 453 laboratory PREPARATION OF EMULSIFUING WAX: Rx *F Cetostearyl alcohol 90 g 6.12 g Sod. Lauryl sulfate 10 g 0.68 g Water 4 ml 0.272 ml Prepare 6.83 g. Calculations : F =6.83/100 = 0.068 Procedure : 1. in a porcelin dish, melt cetostearyl alcohol over a water bath ,then add sod. Lauryl sulfate and mix . add water , heat and stir vigoursly until frothing ceases. ( emulsifying wax). 2. to the emulsifying wax (in step # 1), add white soft paraffin , and stir well to mix . then add liquid paraffin and mix until cold ( emulsifying ointment). 3. in a mortar, triturate salicylic acid and benzoic acid into fine powders. 4. gradually add a smaller portion of the melted emulsifying ointment , stir until smooth. 5. add the remainder of emulsifying ointment and mix thoroughly. 6. transfer to a clean container and fix a red label. Label : Red Compound Benzoic Acid Ointment To be used as directed. Name: Date: Uses: Benzoic acid: is an antibacterial and antifungal agent. Salicylic acid ; is a keratolytic agent. --------------------------------------------------------------------------------------------------- 21 بسمة الدوسري.أ PHT 453 laboratory LYSOL SOLUTION Lysol solution consists of a mixture of cresol and soap solution . It is used as : general disinfectant for hospital use , and as antiseptic solution in vaginal douches in a conc. Of 1:500. Formulation: Lysol solution consist of cresol, soap solution in addition to electrolytes ( e.g., sod chloride, sod. Benzoate, sod. Salicylate) and non-electrolytes (e.g., alcohol, glycerol). Cresol is a substance with a characteristic odour resembling phenol, but more tarry. (caustic substance). Soap; is prepared by interaction of fixed oil (castor oil or olive oil) and fatty acids (oleic acid) with the aid of KOH or NaOH together with water. 22 بسمة الدوسري.أ PHT 453 laboratory PARENTRAL ADMIXTURES AND INCOMPATIBILITIES IV Admixtures: The combination of parenteral dosage forms for administration as single entity is called an ‘ admixture’ . Reasons for Rx admixture: Several drugs are combined and administered together for: 1. The convenience and time saving. 2. Reduction of number of injections. 3. Provide treatment for several conditions simultaneously. 4. Provide ability to give drugs in controlled increments. Parenteral Incompatibilities: When one or more additives are combined with an IV fluid, their presence together may modify the inherent characteristics of the drug substances present. In other words, these incompatibilities take place when drugs are mixed with others to produce a product unsuitable for administration to the patient. i.e., patient may receive subtherapeutic or toxic levels of a drug, and if precipitation occur, it will cause irritation to the vein and occlusion of vessels. Incompatibilities can be classified into three categories: 1. Therapeutic incompatibilities: occur when two or more drugs are administered concurrently resulting in undesirable antagonistic (under dose) or synergistic (over dose) pharmacological action. Adverse drug reactions may be considered as therapeutic incompatibilities. This type of incompatibility is difficult to detect by clinical studies (in vitro & in vivo). Examples of antagonistic effects: Chloramphenicol and penicillin: Penicillin antagonizes the effect of heparin and produces a misleading picture of anticoagulant effect of heparin. Gentamicin and penicillin: ------- in vitro inactivation of each other. Examples of synergistic effects: Folic acid and methotrexate. Calcium ion and digoxin. 2. Physical incompatibilities: occur when the combination of two or more drugs results in a change in the appearance of the solution, such as a change in the color , formation of turbidity or precipitate, or the evolution of a gas . This type of incompatibilities is easily detected by visual detection. Examples: Salts of weak acid Phenobarbital precipitate as free acids in IV solutions having an acidic pH. Cephalothin + gentamicin ------- yellow ppt. Valium (Diazepam), which require a special diluent for solubilization, will precipitate when added to an aqueous solution due to low water solubility. 23 بسمة الدوسري.أ PHT 453 laboratory 3. Chemical incompatibilities: occur when the combination of two or more drug solutions results in degradation of drugs due to hydrolysis, oxidation, reduction, or complexing. This type of incompatibilities is difficult to detect and need suitable analytical methods. Examples: Tetracycline + calcium ------ complex (inactive form). Ampicillin + D5W ----------- hydrolysis. Therefore: 1. Ampicillin should be diluted with normal saline (NS). This sol. Is most stable at pH 7.5, (chemical degradation increases with increasing or decreasing pH. Ampicillin solution is stable: for 8 hr at room temperature, for 48 hr under refrigeration when reconstituted with WFI, for 72 hr under refrigeration when reconstituted with NS. Dextrose solution should be avoided. 2. for Bactrim ( trimethoprim + sulfamethoxazole ): Dextrose is preferred if a dilution of 1:10 ( v/v ) is desirable. D5W or NS is preferred if a dilution of 1:25 ( v/v ) is desirable. An important factor in causing parenteral incompatibilities is a change in the acid-base environment. The solubility and stability of the drug may vary as the pH of the solution changes. The effect of pH on the stability is illustrated in case of penicillin. The antibiotic remains active for 24 hr at pH 6.5, but at pH 3.5 it is destroyed in a short time. Potassium penicillin G contains a citrate buffer and is buffered at pH 6.0 to 6.5 when reconstituted with sterile WFI, dextrose injection, or sodium chloride injection. When this reconstituted solution is added to IV fluid such as dextrose injection or sodium chloride injection, the normal acid pH of the solution is buffered at pH 6.0 to 6.5, thus assuring the activity of the antibiotic. Minimization of incompatibilities: 1. Proper selection of diluents ( either WFI, NS, D5W, LR(lactated Ringer’s) ) 2. Drug concentration: dilution may prevent incompatibility, e.g., erythromycin lactobionate is incompatible with electrolytes in concentrated form. However, it is compatible when properly diluted. Erythromycin + small volume 0.9% NaCl ------ solid gel. Erythromycin + 1 L bottle of 0.9% NaCl -------- will dissolve completely. 3. Increase knowledge of parenteral admixtures and incompatibilities : this is could be made by : Continuous education, especially for IV staff,. Make physician aware of possible incompatibility and always be ready to suggest alternative approaches (either selecting another rout of administration, site of administration, or change the drug involved). Learning to utilize available sources of information , either: Computer system, during entering drug to the patient profile. 24 بسمة الدوسري.أ PHT 453 laboratory 4. 5. 6. 7. Using Micromedex for complete drug monograph. Using available books, e.g., handbook on injectable drugs. Using the paflet of the drug provided by the company. Using available chart alert. Modify the order of mixing. Appropriate storage conditions (at room temp., refrigerated, frozen). Selection of proper container (glass or plastic). For example, diazepam loses 38% of its activity after two hours storage in plastic packages. Periodical observation of running tubes. Tutorial on Handbook of Injectable Drugs: Each drug monograph contains 5 tables: 1. Table 1: solution compatibility for IV administration. 2. Table 2: reconstitution solution for drugs. 3. Table 3: additive compatibility. 4. Table 4: drug in syringe compatibility. 5. Table 5: y-site injection compatibility. Using the Handbook of Injectable Drugs, check the stability of : 1. Ampicillin in D5W. 2. Ampicillin in NS. 3. Hydralazine in LR. 4. Gentamicin in NS. 5. Penicillin G in NS. 6. Clidamycin with penicillins. 7. Insulin with TPN # 9. 8. Morphine and Phenobarbital. Using the drug interaction alert, discuss the drug interaction of the following: 1. Triamterene + enalapril. 2. Lanoxin + inderal. 3. Tyramine + MAO inhibitors. 4. Cold remedies + MAO inhibitors. 5. Aspirin + insulin. 6. Vaccines + corticosteroids. 7. Aspirin + ciprofloxacin. 8. Insulin + thyroid hormone. 9. Ciprofloxacin + digoxin. 10. Theophyllin + propranolol. 11. Imipramine + carbamazepine. 12. Aspirin + probencid. 25 بسمة الدوسري.أ PHT 453 laboratory 13. Indomethacin + frusemide. 14. Verapamil + diazepam. 15. Frusemide + methyl dopa. 16. Gentamicin + ethacrynic acid. 17. Guanethidine + tolbutamide. 18. Amoxycillin + probencid. 19. Aspirin + warfarin. 26 بسمة الدوسري.أ PHT 453 laboratory Using the Handbook of Injectable Drugs, check the stability of: 1. Ampicillin in D5W. 2. Ampicillin in NS. 3. Hydralazine in LR. 4. Gentamicin in NS. 5. Penicillin G in NS. 6. Clidamycin with penicillins. 7. Insulin with TPN # 9. 8. Morphine and Phenobarbital. Using the drug interaction alert, discuss the drug interaction of the following: 1. Triamterene + enalapril. 2. Lanoxin + inderal. 3. Tyramine + MAO inhibitors. 4. Cold remedies + MAO inhibitors. 5. Aspirin + insulin. 6. Vaccines + corticosteroids. 7. Aspirin + ciprofloxacin. 8. Insulin + thyroid hormone. 9. Ciprofloxacin + digoxin. 10. Theophyllin + propranolol. 11. Imipramine + carbamazepine. 12. Aspirin + probencid. 13. Indomethacin + frusemide. 14. Verapamil + diazepam. 15. Frusemide + methyl dopa. 16. Gentamicin + ethacrynic acid. 17. Guanethidine + tolbutamide. 18. Amoxycillin + probencid. 19. Aspirin + warfarin. 27