Neonatal Chest Drain Insertion
advertisement

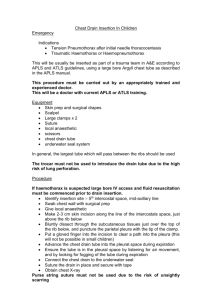
Department of Paediatrics Neonatal Chest Drain Insertion Indications Treatment of pneumothorax Treatment of pleural effusion Complications Haemorrhage may occur if the vascular bundle below the rib is damaged Distortion of breast growth Lung perforation (high risk if trocar is used) Pericardial damage Thoracic duct damage Phrenic nerve injury Diaphragmatic eventration The decision and plan for insertion of chest drain must be discussed with the consultant on call. Chest drain insertion should be performed by an experienced registrar who has previously carried out the procedure competently under consultant supervision. Alternatively the consultant should attend to insert the drain or directly supervise the ST doctor or ANNP. Consent This procedure usually needs to be done as an emergency and should not be delayed while explicit consent is obtained. Admission to NICU carries implicit consent for such emergency procedures. However, it does carry risks and parents need to be fully informed about the procedure at the first suitable opportunity, with full documentation in the notes of the discussion. In the event of the procedure being more elective, evidence of explicit parental consent should be documented in the notes. Equipment Sterile dressing pack and exchange transfusion pack Cleaning solution appropriate to gestation of baby (chlorhexidine 0.05% or saline) Lignocaine 1% with syringe and needles for preparation and injection Chest drains size FG 8, 10, 12 (use largest size possible depending on size of baby) Scalpel and fine straight blade (size 15) Underwater seal chest drainage bottle Pressure suction system Suture and tape for fixing Department of Paediatrics Preparation Give sucrose if time allows and no contraindications Confirm correct side of chest for insertion Aseptic technique Position baby with the affected side elevated 45º to the horizontal, with a roll under the back. The baby should be held with the ipsilateral arm above the head. Clean the skin and infiltrate with 0.125-0.25ml 1% lignocaine Calculate approximate length of insertion of chest tube as distance from insertion site to mid clavicle (term baby 3-4cm: preterm 2-3cm approx guide) Site Anterior axillary line between 4-6th intercostal space (ICS), to avoid unsightly scarring and disruption of breast tissue Some evidence suggests that breast tissue may extend beyond 4th ICS, therefore 5th ICS is preferable For drainage of free air, the drain should be sited anteriorly For drainage of fluid, the drain should be sited posteriorly Procedure (pneumothorax) In a baby you are unable to saturate at >90% you must perform needle thoracocentesis first, without delay, as an emergency. Make small incision, of similar size to diameter of the chest tube (0.51cm) in ICS, just above and parallel to the rib to avoid damage to the subcostal neurovascular bundle The tissues down to the pleura should be dissected bluntly using a curved haemostat or fine artery forceps. As the pleural space is reached a small ‘give’ may be felt and there may be a rush of air. The drain should be introduced into the pleural cavity with the aid of artery forceps to the calculated depth. The trocar must not be used to introduce the drain tube due to the risk of lung perforation. In bigger babies, it may be helpful to use the trocar to stabilise the chest tube, in which case a clamp must be put across the chest tube 12 cm from the end to prevent the end of the trocar advancing further. The chest drain should be advanced anteriorly and towards the apex. The end of the chest drain should be attached to an underwater seal, bubbles should appear indicating successful drainage of free air. Resolution of the pneumothorax will be aided by the application of suction at 5-15cm H2O Department of Paediatrics Fixation Purse string sutures are not recommended due the risk of unsightly scarring A suture should be placed across the wound to close the hole tightly around the drain. If the incision is larger, 2 sutures may be needed. The sutures should then be wrapped round the drain to secure it or inserted through a zinc oxide tape flag positioned round the drain close to its insertion. A transparent dressing should be applied. Aftercare Check that bubbling or oscillation of the water column is seen with every respiration Confirm tube position with chest X-ray (lateral and AP to confirm anterior positioning) Document procedure in notes, including site of insertion and batch number of equipment and method of fixing, with a signed, dated and timed entry Removal When no bubbling has been seen for 24 hours, suction can be discontinued and the drain clamped. Repeat AP chest X-ray at 4-6 hrs to ensure no re-accumulation Give sucrose if no contraindications Remove dressings and cut anchoring sutures Withdraw drain rapidly, while asking an assistant to hold the skin on either side of the drain site together to close the incision. Close the wound with steristrips, a suture is rarely necessary Close clinical observation after removal of drain is sufficient to diagnose re-accumulation of the air leak- routine Chest X-ray is not warranted. References Roberton’s Textbook of Neonatology 4th Ed Janet Rennie Archives of disease in childhood; fetal and neonatal edition;Vol92(1)January 2007pp F46-F48 Chest radiographs after removal of chest drains in neonates: clinical benefit or common practice? van den Boom, J1; Battin, M2 Pediatrics Vol 111 (1) Jan 2003 pp80-86 Breast deformity in adolescence as a result of pneumothorax drainage during neonatal intensive care. Rainer et al BAPM Consent in neonatal clinical care: Good practice framework October 2004 CC/LAW March 2009 (Review March 2011) Gosset guidelines/chest drain insertion