Neutrophil DNA damage in Insulin
advertisement

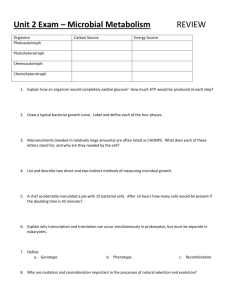
1 Title: Levels of peripheral blood cell DNA damage in Insulin Dependent Diabetes Mellitus (IDDM) human subjects. Running title: DNA damage in diabetic human subjects. 1 2 2 Mary P. A. Hannon-Fletcher , Maurice J. O’Kane , Ken W. Moles , Colin 1 Weatherup1, Christopher R. Barnett and Yvonne A. Barnett* 1 1 Cancer and Ageing Research Group, University of Ulster, Cromore Road, Coleraine, County Londonderry, Northern Ireland, BT52 1SA. 2 Altnagelvin Area Hospital, Glenshane Road, Londonderry, BT47 1SB. *Corresponding author ya.barnett@ulst.ac.uk Tel: +44-(0)-2870-324627 Fax: +44-(0)-2870-324965 2 Abstract Increased production of reactive oxygen species in vivo can lead to cellular biomolecule damage. Such damage has been suggested to contribute to the pathogenesis of IDDM. In this study we used the alkaline comet assay to measure DNA damage (single-stranded DNA breaks and alkali-labile sites) in freshly isolated whole blood, lymphocytes, monocytes and neutrophils from 23 subjects with IDDM and 32 age- and sex-matched controls. Analysis of the results showed elevated levels of DNA damage (expressed as % comet tail DNA) in the lymphocyte (4.10±0.47; 3.22±0.22), monocyte (4.28±0.47; 3.49±0.18) and whole blood (4.93±0.51; 4.51±0.23) fractions from IDDM subjects compared to controls, respectively, but the increases observed were not statistically significant. However, we found significantly elevated basal levels of DNA damage in the neutrophil fraction (8.38±0.64; 4.07±0.23; p<0.001, Mann-Whitney U test) in IDDM subjects compared to controls. Given these novel neutrophil findings we extended the study to include a total of 50 IDDM subjects and 50 age- and sex-matched control subjects, and determined basal levels of DNA damage in the neutrophils of all 100 subjects. We found significantly elevated mean levels of DNA damage (8.40±0.83; 4.34±0.27; p<0.001, MannWhitney U test) in the neutrophils from the IDDM subjects when compared to controls. Our results show that even with acceptable glycaemic control there is a significantly elevated level of DNA damage within diabetic neutrophils in vivo. Keywords: Alkaline comet assay, DNA damage, Neutrophils, IDDM, %Hba1c. 3 1. Introduction Insulin Dependent Diabetes Mellitus (IDDM) is associated with increased oxidative stress in vivo. Studies on diabetic subjects have demonstrated increased free radical production contributed to by hyperglycaemia resulting in glycosylated proteins and production of reactive oxygen species (ROS) [1]. In addition, superoxide anions produced during these reactions react with plasma lipids leading to the generation of chemotactic factors, which in turn are capable of stimulating neutrophils with subsequent release of enzymes stored in cytoplasmic granules and the additional production of ROS [2-4]. The oxidative stress is further exacerbated by decreases in antioxidant enzyme activity, including superoxide dismutase, catalase and glutathione peroxidase [3, 5-7]. Under conditions of oxidative stress damage to cellular biomolecules (lipids, proteins, carbohydrates and DNA) can occur. Until the late 90’s the main marker used as an index of in vivo oxidative damage in IDDM has been the detection of lipid peroxidation products in plasma and cell membranes [814]. Polyunsaturated fatty acids are among the most readily oxidised substrates in biological systems. A broad range of oxidation products have been described [15], including lipid peroxides, which are precursors to other reactive intermediates, such as alkoxyl radicals, and hydroxyalkenals formed in lipid peroxidation reactions, including malondialdehyde (MDA). A number of lipid peroxidation products mainly, MDA and 4-hydroxy-2-nonenal [16], are known to interact with DNA [17]. Such interaction can lead to cytotoxicity, genotoxicity and carcinogenicity [18]. More recently (1995) oxidative damage to DNA has been demonstrated by measuring levels of 8-hydroxydeoxyguanosine, a recognised biomarker of oxidant-induced DNA damage, in both mononuclear cells and sperm from diabetic subjects, using high performance liquid chromatography [19, 20]. Other groups have measured DNA 4 damage levels in mononuclear cells from IDDM subjects, using the comet assay/alkaline unwinding techniques. The results from these studies have shown increases, in subjects with poor glycaemic control [21,22] and no significant changes, in subjects with good glycaemic control [22, 23], in levels of DNA damage when compared to control subjects. Previous work in this laboratory [6] measured DNA damage (single-strand breaks and alkali-labile sites) using a sandwich ELISA described by van Loon et al. [24] in whole blood and phytohaemagglutinin (PHA)-stimulated lymphocytes from 20 IDDM subjects and from 11 control subjects. Results showed significantly increased basal levels of DNA damage in whole blood but not lymphocytes, from the IDDM subjects compared to controls. In light of this whole blood DNA damage data we decided to investigate the types of DNA damage and the levels of DNA damage present in the various different types of nucleated blood cells (lymphocytes, monocytes and neutrophils) from IDDM subjects. In this paper we report the results obtained from the analysis of levels of DNA damage. 2. Materials and Methods 2.1. Subjects 50 IDDM subjects (mean age 36.3 ± 1.95 years; 30 males and 20 females), were recruited from the Diabetic Clinic, Altnagelvin Hospital, Londonderry, Northern Ireland. Thirteen of the diabetic subjects presented with at least one complication (retinopathy, nephropathy, neuropathy and macrovascular disease) and 8 were smokers. The control group consisted of 50 healthy individuals recruited from the University of Ulster (mean age 37.6 ± 1.15 years; 22 females and 28 males, none of 5 whom were smokers, nor did they have a family history of diabetes). Ethical approval for this study was obtained from the University of Ulster Ethical Committee and from the Ethical Committee at Altnagelvin Hospital. All subjects gave their informed consent prior to enrolment into the study. 2.2. Collection and processing of blood samples 15 ml of peripheral blood was collected from each study subject. 10 ml was collected into lithium heparin-coated vacutainers® (Becton-Dickinson, UK) for subsequent determination of basal levels of DNA damage within nucleated blood cells. The remaining 5ml was collected into EDTA-coated vacutainers® (Becton-Dickinson, UK) for HPLC analysis of glycated haemoglobin (expressed as %HbA1c), using a method described by John et al. [25]. Analysis of DNA damage in the lymphocyte, monocyte and whole blood fractions was carried out on 23 diabetic subjects and 32 control subjects. Analysis of DNA damage in the neutrophil fraction was carried out on samples from 50 IDDM subjects and 50 control subjects. 2.3. Cell isolation and preparation for the comet assay 2.3.1. Whole blood 50 l of fresh whole blood was transferred to an eppendorf and washed twice, (700 x g for 5 min at 4OC) in 200 l of Ca++ and Mg++ free phosphate buffered saline (PBS, Sigma, Poole, UK.). The resulting cell pellet was re-suspended in 10l of PBS and stored at 4OC in the dark (to minimise additional DNA damage and repair), for use the same day in the comet assay. 6 2.3.2. Mononuclear cell isolation Mononuclear cells were isolated from whole blood using a method described by Böyum [26]. Essentially, whole blood was mixed 1:1 with RPMI 1640 (Gibco Life Technologies, UK) then 8 ml of diluted blood was layered onto 10 ml of Histopaque 1077 (Sigma, Poole, UK) in a sterile 25 ml universal container (Sterilin, UK), at room temperature. Following centrifugation at 700 x g for 30 min, the mononuclear layer (“buffy layer”) was carefully aspirated, mixed with 10 ml RPMI 1640 and centrifuged at 500 x g for 10 min. After an additional wash in RPMI 1640 the mononuclear cells were incubated for 4 hours in RPMI 1640 with 10% foetal calf serum, 200 µg/ml sodium pyruvate, 100 U/ml penicillin and 100 µg/ml streptomycin (BDH Laboratory Supplies, Poole, UK) at 37oC (5% CO2: air humidified atmosphere). Following incubation the medium, which contained the lymphocyte fraction, was decanted into a labelled centrifuge tube. The monocytes, which had adhered to the culture flask, were removed into a labelled centrifuge tube using cold PBS and a cell scraper. Both the lymphocyte and monocyte fractions were washed briefly (x 2) with PBS. The resulting cell pellets were re-suspended in 5 ml PBS and kept at 4oC in the dark, for use the same day in the comet assay. Cell viability was assessed by trypan blue exclusion following isolation, and was found to be >95%. 2.3.3. Neutrophil isolation Following the removal of the mononuclear layer the blood sample was further processed for the separation of neutrophils using a dextran sedimentation method described by Markert et al. [27]. Essentially, the Histopaque layer was carefully aspirated and discarded, 6 ml of PBS was added to the red cell-neutrophil mixture, 7 followed by 10 ml of the 2% dextran (Sigma, Poole, UK) in normal saline (0.9% (w/v) NaCl in distilled water). This suspension was well mixed and allowed to settle for 35-45 min at room temperature, after this time the suspension well have settled into two layers, an upper layer which consists mainly of neutrophils and a lower layer which contains the red cells. The upper layer was carefully removed and centrifuged at 500 x g for 10 min. The supernatant was discarded and 6 ml of ice cold sterile distilled water was added and mixed well for 20 sec, before adding 2 ml of PBS containing 3.4% NaCl (w/v) (BDH Laboratory Supplies, Poole, UK). This suspension was then centrifuged at 500 x g for 10 min and the resulting neutrophil pellet was re-suspended in 5 ml PBS and kept at 4oC in the dark, for use the same day in the comet assay. Cell viability was assessed by trypan blue exclusion following isolation, and was found to be >95%. 2.4. The alkaline comet assay The alkaline comet assay facilitates the detection of DNA strand-breakage, alkalilabile abasic sites, and intermediates in base- or nucleotide-excision repair. In the comet assay, DNA strand breaks allow DNA to extend from lysed and salt extracted nuclei, or nucleoids, to form a comet-like tail on alkaline electrophoresis. The slides are stained with ethidium bromide and comet “tails” viewed by fluorescence microscopy. In undamaged cells a bright fluorescent core is seen with a less intense edge of fluorescence facing the anode. If damage is present, fluorescence appears in a “tail” extending from the core towards the anode. In this investigation we measured basal levels of DNA damage in whole blood, freshly isolated lymphocytes, neutrophils and monocytes in IDDM and control subjects. 8 The alkaline comet assay procedure in this study was a modification of the method described by Singh et al. [28]. Essentially, 100 l of 0.5% normal melting point agarose (Sigma, Poole, UK) was pipetted onto frosted microscope slides and allowed to solidify under a coverslip, which was then carefully removed. Approximately 10,000 cells were suspended in 75 l low melting point agarose gel, the cell suspension was rapidly pipetted onto the first agarose layer, and gently spread by placing a coverslip on top. This was allowed to solidify on an ice tray for 5 min. After removal of the coverslip, the slide was immersed in freshly prepared lysing solution (2.5M NaCl, 100mM EDTA, and 10mM Tris, with 1% Triton X-100 and 10% DMSO) made up just before use and incubated overnight at 4oC. The slides were removed from the lysing solution, drained and placed in a horizontal gel electrophoresis tank. The tank was filled with fresh, cold electrophoresis solution (1mM EDTA and 300mM NaOH) to a level approximately 0.25 cm above the slides. The slides were left in the solution for 20 min to allow the unwinding of the DNA and expression of alkali-labile damage before electrophoresis. Electrophoresis was conducted at 4oC for 30 min using 25 V and a current of 300 mA. Following electrophoresis the slides were washed (x 3) in Tris buffer (0.4M Tris, pH 7.5) to neutralise the excess alkali. Finally, the slides were stained with 75 l ethidium bromide (20 g / ml; Sigma, Poole, UK 2.5. Image analysis of slides Slides were stored in a light-proof box containing tissues moist with PBS and viewed within 12 hours of staining. Observations were made using an Ophtiphot II compound microscope (Nikon) equipped with an epifluorescence mercury lamp 9 source (excitation filter 515, barrier filter 590 nm) and x 40 Nikon Fluor objective (numerical aperture 0.85), and Komet 3.0 image analysis programme (Kinetic Imaging Ltd, Liverpool, UK). 2.6. Analysis of DNA damage The image analysis software provides a full range of densitometric and geometric parameters describing the complete comet, as well as the head and tail portions. Since the comet assay essentially reflects the displacement of fluorescence from the head to the tail in damaged cells we used %tail DNA i.e. the percentage of total nuclear DNA that has migrated to the tail, as the parameter to quantify basal levels of DNA damage. Each blood/blood cell type sample was analysed in duplicate and 50 cells per slide were counted. 2.7. Statistical analysis Statistical analysis was performed using the SPSS statistical package to compare the variances of all parameters examined using Levene’s test of homogeneity of variances. Differences in measured parameters between normal and IDDM subjects were assessed by the Mann-Whitney U test, since the variances in the two samples were heterogeneous. Differences in the measured parameters between IDDM subjects with, and without, complications were measured using the Student’s t-test. The relationship between DNA damage and %HbA1c was analysed using least squares linear regression analysis. A p value of <0.05 was considered statistically significant. All results are expressed as mean ± standard error of the mean (SEM). 10 3. Results %HbA1c levels (Table 1) were significantly increased in IDDM subjects (7.71±0.03; n=50) in comparison to controls (4.28±0.06; n=50; p <0.001). The range of levels indicated that all IDDM patients were under acceptable clinical control. In the initial study group of 23 IDDM subjects and 32 controls we found increased levels of DNA damage (%tail DNA, Figure 1) in the lymphocyte (4.10±0.47 and 3.22±0.22), monocyte (4.28±0.47and 3.49±0.18) and whole blood (4.93±0.51 and 4.51±0.23) fractions of the IDDM subjects, respectively, when compared to controls. These increases were not statistically significant. However, there were significantly elevated basal levels of DNA damage in the neutrophil fraction of IDDM subjects, when compared to control subjects (8.38±0.64 and 4.07±0.23 respectively, p<0.001). These findings on DNA damage levels in neutrophils of IDDM subjects were further confirmed by increasing the number of subjects examined to 50 IDDM subjects and 50 control subjects. This extended study also revealed significantly elevated basal levels of DNA damage in the neutrophils from IDDM subjects compared to the control group, respectively (8.40±0.83 and 4.34±0.27; p<0.001, Figure 1). Of the 50 IDDM subjects, eight were smokers, three of the smokers also had at least one complication. Because of small numbers it was not possible to determine by statistical analysis if the values obtained for the various endpoints (%HbA1c and %tail DNA damage) were different in IDDM subjects who smoked compared to those who did not, but this did not appear to be the case. Thirteen of the IDDM subjects presented with at least one complication (retinopathy, neuropathy, nephropathy, ischemic heart disease). There were no significant differences in values of %HbA1c or %tail DNA damage measured in the IDDM subjects with complications compared to those who did not have complications. 11 There was no correlation between basal DNA damage levels (%tail DNA) and %HbA1c in the IDDM subjects. 4. Discussion IDDM is associated with increased oxidative stress in vivo [2, 3, 29, 30]. The elevated oxidative stress may be caused by; increased levels of free radicals due to their increased production, and/or decreases in the antioxidant defense systems [3, 57]. The increased oxidative stress together with poor metabolic control enhances lipid peroxidation in diabetic patients, which has been proposed to be associated with the aetiology of diabetic complications [12, 31, 32]. In the present study we used the alkaline comet assay to measure basal levels of DNA damage in freshly isolated whole blood and individual blood cell fractions from IDDM subjects. We found increased levels of DNA damage in the lymphocyte, monocyte and whole blood cell fractions from IDDM subjects, however the increases observed were not significantly different from controls. Conflicting reports regarding levels of DNA damage in mononuclear cells from diabetic subjects have been reported recently in the literature. Collins et al. [21] reported elevated levels of DNA damage in mononuclear cells from IDDM patients with poor glycaemic control (11.0±2.9 %HbA1c). Collins’ group measured DNA damage using both the alkaline comet assay and a modification of the assay which incorporates a digestion of nucleoid DNA with specific endonucleases which allows detection of specific types of damage such as; oxidised pyrimidines and purines. Lorenzi et al. [22] measured DNA damage, using the alkali unwinding assay, in mononuclear cells from patients with poor glycaemic control (12.9±2.4 %HbA1c) and found elevated levels of DNA damage. In the same study they also reported no significant changes in DNA damage 12 in subjects with good glycaemic control (%HbA1c 7.4±1.5%). In agreement with these findings, we [6], and Anderson et al. [23], did not find significant differences in levels of DNA damage in lymphocytes and mononuclear cells, respectively from IDDM subjects with good glycaemic control, when compared to controls. In our previous study [6] we measured levels of DNA damage in PHA-stimulated lymphocytes, which are more proficient at DNA repair than unstimulated lymphocytes (like many found in vivo) [33], and so the levels which we measured in vitro may not have been a true reflection of those existing in vivo. As glycaemic control plays an important role in the progression of IDDM and the development of secondary complications, it is perhaps not surprising that changes in the level of an index of biomolecule damage, in this case DNA damage in mononuclear cells, correlates with %HbA1c in diabetic patients, in some studies. As the subjects in our study and in both, Lorenzi et al. [22] and Anderson et al. [23], had good glycaemic control this may help explain why we could not detect significant increases in levels of DNA damage. In addition to measuring levels of DNA damage in the PHA-stimulated lymphocytes in our previous study we also measured basal levels of DNA damage in fresh whole blood using an ELISA [6]. We found significantly higher levels of DNA damage in whole blood from IDDM subjects when compared to controls. These findings do not agree with those of our present study. Discrepancies in the total amount of DNA damage detected by the ELISA and the comet assays have been reported previously [34] and are the likely cause of the different results between our two studies. The ELISA measures DNA strand breaks, including damage associated with dead, dying and apoptotic cells, to which the D1B antibody (raised against single-strand DNA) has bound. However, the alkaline comet assay depends on observations made on 13 individual cells with some degree of intact morphology, therefore dead, dying or apoptotic cells cannot be easily scored and so DNA damage levels would tend to be lower with the comet assay compared to the ELISA. What then are the likely causes and effects of the increased levels of DNA damage found in the neutrophils of the diabetic subjects? Neutrophils play an important role in host defence against bacterial infection. The suppression of neutrophil function could potentially exacerbate infection. Under normal circumstances stimulated neutrophils kill bacteria via the production of ROS (superoxide anion, hydroxyl radicals and hydrogen peroxide) during the ‘respiratory burst’ [35]. Disturbances in neutrophil function including abnormal chemotaxis [36, 37], phagocytosis [38-40], intracellular killing [39-42], and adherence [43-44] in diabetes have been well documented. A consequence of such inefficient neutrophil bactericidal mechanisms may be the increased susceptibility of IDDM subjects to certain bacterial and fungal infections [45]. In addition, diabetic subjects’ neutrophils are in a chronic state of activation generating increased levels of ROS [2, 41, 46]. It is well documented that ROS are capable of causing DNA damage [47-49] and it has been shown that neutrophils in a chronic low state of activation are capable of generating sufficient ROS to induce DNA damage in vitro [50]. We report for the first time that such chronic activation may result in elevated levels of DNA damage within neutrophils in vivo. Under normal circumstances activated neutrophils are protected from ROS-induced damage by increasing their intake of vitamin C by as much as ten-fold above the concentrations present in normal neutrophils. Extracellular and intracellular vitamin C are necessary for optimal bacterial killing by neutrophils in vitro and in vivo [51]. However, in diabetic subjects plasma and leucocyte levels of vitamin C have been 14 shown to be significantly reduced [7, 52-54]. The decreased protection afforded by vitamin C in the neutrophils of diabetic subjects is likely to contribute to the elevated levels of DNA damage, which we report here. There have been reports that neutrophil production of hypochlorous acid and Nchloramines inhibit DNA repair [49, 55]. Such inhibition of repair in vivo is likely to exacerbate levels of ROS-induced damage to DNA in neutrophils within diabetic subjects. Our data suggests that even with acceptable glycaemic control in IDDM subjects there is a significantly elevated level of DNA damage within diabetic neutrophils in vivo. The increased levels of basal neutrophil DNA damage in IDDM may contribute to the altered neutrophil function, reported elsewhere, in patients with IDDM and is worthy of further investigation. Acknowledgements This work was supported by a Department of Education Northern Ireland (DENI) Postgraduate Student Distinction Award to Mary P.A. Hannon-Fletcher. We would like to thank all the subjects who participated in the study. 15 References [1] J.V. Hunt, R.T. Dean, S.P. Wolff. Hydroxyl radical production and autoxidative glycosylation, Biochem. J., 256 (1988) 205-212. [2] D.A. Zozulinska, B. Wierusz-Wysocka, H. Wysocki, A.E. Majchrzak, A. Wykretowicz. The influence of insulin-dependent diabetes mellitus (IDDM) duration on superoxide anion and hydrogen peroxide production by polymorphonuclear neutrophils, Diab. Res. Clin. Practice., 33 (1996) 139-144. [3] B. Lacka, W. Grzeszcrzak, K. Strojek, K. Twardowska, J. Froehlich, A. Jendryczko. Pro-oxidant - antioxidant imbalance in insulin dependent diabetes mellitus, Diabetologia, 38 (1995) Suppl. 1:A40. [4] M. Vucic, B. Rocic, V. Bozikov, I. Pavlic-Renar, R. Mesic, J. Knezevic, Z. Metelko. Lymphocyte superoxide dismutase activity and total plasma antioxidants in type I diabetes, Diabetologia, 38 (1995) Suppl. 1:A252. [5] I. Akkus, S. Kalak, H. Vuralm, O. Caglayan, E. Menekse, G. Can, B. Durmus. Leukocyte lipid peroxidation superoxide dismutase glutathione peroxidase and serum and leukocyte vitamin C levels of patients with type II diabetes mellitus, Clin. Chim. Acta., 244 (1996) 221-227. [6] M.P.A. Hannon-Fletcher, C. Hughes, K.W. Moles, C.R. Barnett, Y.A. Barnett. An investigation of in vivo antioxidant status and DNA damage in patients with IDDM, in: T.K. Basu, N.J. Temple, and M. Garg (Eds.), Antioxidants in Human Health and Disease, CABI Publishing, Oxon, UK, 1999, pp.259-269. [7] K.H. Thompson, D.V. Godin. Micronutrients and antioxidants in the progression of diabetes, Nutr. Res., 15 (1995) 1377-1410. [8] T.J. Lyons. Oxidized low density lipoproteins. A role in the pathogenesis of arteriosclerosis in diabetes, Diabetic Med., 8 (1991) 411-419. 16 [9] S.K. Jain, R. McVie, J. Duett, J.J. Herbst. Erythrocyte membrane lipid peroxidation and glycosylated haemoglobin in diabetes, Diabetes, 38 (1989) 1539-1543. [10] B. Matkovics, S.Z.I. Varga, H. Witas. The effect of diabetes on the activities of the peroxide metabolism enzymes, Horm. Metabol. Res., 14 (1982) 77-79. [11] R. Kakkar, J. Kalra, S.V. Mantha, K. Prasad. Lipid peroxidation and activity of antioxidant enzymes in diabetic rats, Mol. Cell. Biochem., 151 (1995) 113-119. [12] D. Armstrong, F. Al-Awadi. Lipid peroxidation and retinopathy in streptozotocin-induced diabetes, Free Radical Biol. Med., 11 (1991) 433-436. [13] T. Koschinsky. Do lipoprotein glycation and peroxidation play a role in the development of macrovascular disease in young patients with diabetes? Structural and Functional Abnormalities in Subclinical Diabetic Angiopathy, in: B. Weber, W. Burger and T. Danne (Eds.), Paediatric Adolescent Endocrinology, Karger, Basel, 1992, pp. 32-43. [14] O.M. Panasenko, S.A. Evgina, R.K. Aidyraliev, V.I. Sergienko, Y.A. Vladimirov. Peroxidation of human blood lipoproteins induced by exogenous hypochlorite or hypochlorite generated in the system of “myeloperoxidase + H2O2 + C1-”, Free Radical Biol. Med., 16 (1994) 143-148. [15] O.J. Aruoma, B. Halliwell, M. Dizdaroglu. Iron ion-dependent modification of bases in DNA by the superoxide radical-generating system hypoxanthine/xanthine oxidase, J. Biol. Chem., 264 (1989) 13024-13028. [16] W.A. Pryor, N.A. Porter. Suggested mechanisms for the production of 4hydeoxy-2-noneal from autoxidation of polyunsaturated fatty acids, Free Radical Biol. Med., 8 (1990) 541-543. 17 [17] C.E. Vaca, J. Wilhelm, M. Harms-Ringdahl. Interaction of lipid peroxidation products with DNA. A review, Mutation Res., 195 (1988) 137-149. [18] H. Esterbauer, R.J. Schaur, H. Zollner. Chemistry and biochemistry of 4hydroxynonenal, malonaldehyde and related aldehydes, Free Radical Biol. Med., 11 (1991) 81-128. [19] P. Dandona, K. Thusu, S. Cook, B. Snyder, J. Makowski, D. Armstrong, T. Nicotera. Oxidative damage to DNA in diabetes mellitus, Lancet, 347 (1996) 444-445. [20] K. Thusu, T. Nicotera, A. Aljada, J. Makowski, P. Dandona. Oxidative damage to DNA in spermatozoa in diabetes mellitus, Diabetes, (1995) 44 Suppl. 1:112A. [21] A.R. Collins, K. Raslová, M. Somorovská, H. Petrovská, A. Ondrušová, B. Vohnout, R. Fábry, M. Dušinská. DNA damage in diabetes: correlation with a clinical marker, Free Radical Biol. Med., 25 (1998) 373-377. [22] M. Lorenzi, D.F. Montisano, S. Toledo, H.C. Wong. Increased single strand breaks in DNA of lymphocytes from diabetic subjects, J. Clin. Invest., 79 (1987) 653-656. [23] D. Anderson, T-W. Yu, J.Wright, C. Ioannides. An examination of DNA strand breakage in the Comet Assay and antioxidant capacity in diabetic patients, Mutation Res., 398 (1998) 151-161. [24] A.A.W.M. van Loon, R.H. Groenendijk, A.J. Timmerman, G.P. van der Schans, P.H.M. Lohman. R.A. Baan. Quantitative detection of DNA damage in cells after exposure to ionising radiation by means of an improved immunochemical assay, Mutation Res., 274 (1992) 19-27. [25] W.G. John, D.G. Bullock, F. MacKenzie. Methods for the analysis of glycated haemoglobins: What is being measured?, Diabetic Med., 9 (1992) 15-19. 18 [26] A. Böyum. Isolation of mononuclear cells and granulocytes from human blood, in: Norwegian Defence Research establishment Division for Toxicology Kjeller Norway. 1980, Paper iv: pp. 77-89. [27] M. Markert, C.A. Particia, B.M. Babior. Measurement of O2- production by human neutrophils. The preparation and assay of NADPH oxidised containing particles from human neutrophils, Method. Enzymol., 105 (1984) 358-362. [28] N.P. Singh, M.T. McCoy, R.R. Trice, E.L. Schneider. A simple technique for quantification of low levels of DNA damage in individual cells, Exp. Cell. Res., 175 (1988) 184-194. [29] A.S. Krolewski, J.H. Warram, L.I. Rand, C.R. Kahn. Epidemiological approach to the etiology of type I diabetes mellitus and its complications, N. Engl. J. Med., 317 (1987) 1390-1398. [30] F.A. Gries, H. Kolb, T. Koschinsky. Free radicals in the pathogenesis of diabetes and its complications, in: R.G. Cutler, L. Packer, J. Bertram and A. Moro (Eds.), Oxidative Stress and Aging. 1995, pp.91-200. [31] J.V. Hunt, S.P. Wolff. Oxidative glycation and free radical production: A casual mechanism of diabetic complications, Free Rad. Res. Commum., 12 (1991) 115-123. [32] A. Parthiban, S. Vijayalingam, K.R. Shanmugasundaram, R. Mohan. Oxidative stress and the development of diabetic complications - antioxidants and lipid peroxidation in erythrocytes and cell membrane, Cell. Biol. Int. 19 (1995) 987993. [33] A.R. Collins, M. Ai-Guo, S.J. Duthie. The kinetics of repair of oxidative DNA damage (strand breaks and oxidised pyrimidines) in human cells, Mutation Res., 336 (1995) 69-77. 19 [34] I.D. Logan, Y.A. Barnett. A comparison between the application of the comet assay and an immunochemical DNA damage assay on the level of DNA damage within X-ray irradiated human whole blood, Biochem. Soc. Trans., 86 (1998) 26. [35] V. Esman. The polymorphonuclear leucocyte in diabetes, Fresen. J. Anal. Chem. 311 (1982) 344-348. [36] A.G. Mowat, J. Baum. Chemotaxis of polymorpher leucocytes from patients with diabetes mellitus, N. Engl. J. Med. 284 (1971) 621-27. [37] P-A. Oldenborg, J. Sehlin. D-glucose but not insulin reduces N-formylmethionyl-leucyl-phenylalanine (fMet-leu-phe)-induced shape changes in suspended human neutrophils, Bioscience Rep. 17 (1997) 475-486. [38] J.D. Bagdade, R.K. Root, R.J. Bulger. Impaired leukocyte function in patients with poorly controlled diabetes, Diabetes 23 (1974) 9-15. [39] B. Wierusz-Wysocka, H. Wysocki, A. Wykretowicz, A. Szczepanik, H. Siekierka. Phagocytosis bactericidal capacity and superoxide anion (O2-) production by polymorphonuclear neutrophils from patients with diabetes mellitus, Folia. Haematol. Leipzig 112 (1985) S658-668. [40] R.M. Wilson W.G. Reeves. Neutrophil phagocytosis and killing in insulindependent diabetes, Clin. Exp. Immunol. 63 (1986) 478-484. [41] B. Wierusz-Wysocka, A. Wykretowicz, H. Byks, K. Sadurska, H. Wysocki: Polymorphonuclear neutrophils adherence superoxide anion (02-) production and HbA1 level in diabetic patients, Diab. Research & Clin. Practice 21 (1993) 109114. [42] J.S. Tan, J.L. Anderson, C. Watanakunakorn, J.P. Phair: Neutrophil dysfunction in diabetes mellitus, J. Lab. Clin. Med. 85 (1975) 26-33. 20 [43] B. Andersen, G.H. Goldsmith, P.J. Spagnuolo. Neutrophil adhesive dysfunction in diabetes mellitus: The role of cellular and plasma factors, J. Lab. Clin. Med. 111 (1988) 275-285. [44] J.A. Olson, C.M. Whitelaw, K.C. McHardy, D.W.M. Pearson, J.V. Forrester. Soluble leucocyte adhesion molecules in diabetic retinopathy stimulate retinal capillary endothelial cell migration, Diabetologia, 40 (1997) 1166-1171. [45] G.F. Thornton: Infections and diabetes, Med. Clin. N. Am. 55 (1971) 931-938. [46] S-H. Ihm, H.J. Yoo, S.W. Park, C.J. Park. Effect of tolrestat and aldose reductase inhibitor on neutrophil respiratory burst activity in diabetic patients, Metabolism, 46 (1997) 634-638. [47] M. Dizdaroglu, Z. Nackerdien, B-C. Chao, E. Gajewski, G. Rao. Chemical nature of in vivo DNA base damage in hydrogen peroxide-treated mammalian cells, Arch. Biochem. Biophys. 285 (1991) 388-390. [48] O.I. Aruoma, B. Halliwell, E. Gajewski, M. Dizdaroglu. Damage to the bases in DNA induced by hydrogen peroxide and ferric ion chelates. J. Biol. Chem. 264 (1989) 20509-20512. [49] R.W. Pero, Y. Sheng, A. Olsson, C. Bryngelsson, M. Lund-Pero. Hypochlorous acid/N-chloramines are naturally produced DNA repair inhibitors, Carcinogenesis, 17 (1996) 13-18. [50] S.A. Weitzman, L.I. Gordon. Inflammation and cancer: Role of phagocytegenerated oxidants in carcinogenesis, Blood, 76 (1990) 655-663. [51] P.W. Washko, Y. Wang, M. Levine. Ascorbic acid recycling in human neutrophils, J. Biol. Chem., 268 (1993) 15531-15535. [52] J. Lysy, J. Zimmerman. Ascorbic acid status in diabetes mellitus, Nutr. Res., 12 (1992) 713-720. 21 [53] G. Seghieri, L. Martinoli, M. Miceli, M. Ciuti, G. D’Alessandri, A. Gironi, L. Palmieri, R. Anichini, G. Bartolomei, F. Franconi. Renal excretion of ascorbic acid in insulin dependent diabetes mellitus, Int. J. Vitam. Nutr. Res., 64 (1993) 119-124. [54] A.M. Bode, C.R. Yavarow, D.A. Fry, T. Vargas. Enzymatic basis for altered ascorbic acid and dehydroascorbic acid levels in diabetes, Biochem. Biophys. Res. Commun. 191 (1993) 1347-1353. [55] T. Ogino, L. Packer, J.J. Maguire. Neutrophil antioxidant capacity during the respiratory burst: loss of glutathione induced by chloramines, Free. Radical Biol. Med. 23 (1997) 445-452. 22 Table 1. Glycated haemoglobin (%HbA1c) levels in blood from IDDM and control subjects. %HbA1c Control IDDM (n = 50) (n = 50) 4.28 ± 0.06 *7.71 ± 0.03 Values are Mean ± SEM in all groups. *p<0.0001 when compared to control. 23 Figure 1. Basal levels of DNA damage (%tail DNA) in lymphocyte, monocyte, neutrophil and whole blood fractions from IDDM and control subjects 10.00 * 9.00 Control Type I diabetic subjects 8.00 7.00 6.00 DNA damage (%tail DNA) 5.00 4.00 3.00 2.00 1.00 0.00 Lymphocytes Monocytes Neutrophils Whole blood Values are Mean ± SEM for all groups. *p<0.001 when compared to control. Analysis of DNA damage within whole blood, lymphocyte and monocyte cell fractions was carried out on 32 control subjects and 23 IDDM subjects. Analysis of DNA damage within the neutrophil cell fraction was carried out on 50 control and 50 IDDM subjects.