Anatomy And Physiology
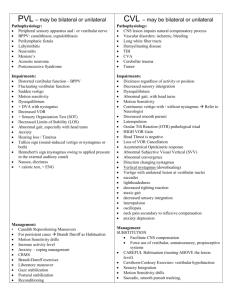
advertisement

Anatomy and Physiology Vestibular Training The 90 Minute Guide SCC: rotational movement. Saccule: Linear movement Utricle: gravity movement Otolinths: “crystals” • • • • By Jillian Fontana, PT, DPT, CTRS Updated 8/22/14 Objectives • Brief review of the Anatomy and Physiology of the Vestibular System • Identify and appraise the difference between central disorders, peripheral disorders and BPPV through patient’s History and Special Tests. • Identify effective treatment based upon positive tests and differential diagnosis. • Navigate a cheat sheet to assist you in practice. Functions of the Vestibular System Senses and perceives body position and self-motion. Enables gaze stability. Statically aligns the head and body to vertical. Detects the direction of gravity and helps to maintain the orientation of the whole body to vertical (Postural Stability) • Selects appropriate sensory cues for postural orientation in different sensory environments. • Assists in controlling the position of the body’s center of mass both for static positions and dynamic movements. • Stabilizes the head during postural movements. • • • • From Heather Dillon Anderson’s Vestibular Rehab lecture PT, DPT, NCS Quick Reminders: Terms to Know Anatomy and Physiology • http://www.youtube.com/watch?v=BbKU0Ab bARg • This video illustrates a quick review of the vestibular system. • Nystagmus – “a term to describe fast, uncontrollable movements of the eyes that may be: – Side to side (horizontal nystagmus) – Up and down (vertical nystagmus) – Rotary (rotary or torsional nystagmus)” • Vertigo: “a sensation of motion in which the individual or the individual's surroundings seem to whirl dizzily” http://www.merriam-webster.com/dictionary/vertigo Vertigo vs. Light headedness – “Spinning” vs. “floating” Aural Fullness: feeling of ears needing to pop like descending from airplane Oscillopsia: objects moving in visual field Tinnitus: ringing in the ear VOR – Vestibular Ocular Reflex http://www.nlm.nih.gov/medlineplus/ency/article/003037.htm • • • • • 1 Quick Reminder: Concepts to Know Vestibular Exam: History • Essential to categorize sx - • Alexander’s Law; • “Jerk nystagmus worsens when gazing in the direction of the fast component.” If it switches direction it is a central disorder. http://medical-dictionary.thefreedictionary.com/Alexander+law • http://www.youtube.com/watch?v=mghGeKkNBzQ • Vestibular Crisis: • Sudden dizziness, loss of balance, nausea, vertigo lasting 1-4 days associated with head motion. (Patient upstairs this past week was in vestibular crisis) – – – – – • Characteristics and timing of Sx important – Frequency – Length? – Triggers? • Explore Psych Component (H/o panic attacks, recent increase in stress? ) • Anything ruled out? (MRI, Neurology/Cardiac work-up) Examination • The key to determining type of dysfunction is the interview. • Red Flags? – New onset of Sx which may represent stroke (dysphagia, diplopia, dysarthria) – Constant, unremitting symptoms – Progressive/worsening symptoms – Patients without any previous medical tests (if you cannot produce any symptoms) • Previous Tests? Previous Treatment? • Reminder: Your patient may not be able to tolerate a complete examination in one session. true vertigo vs. dizzy Light-headedness vs. spinning Episodic-spontaneous vs. motion provoked? Continuous exacerbations? Other sx: Panic attacks? Headaches? Mood Swings? Vestibular - Examination • Differential Diagnosis: – Orthostatic Hypotension • B.P supine sitting standing – Wait 5 minutes between each reading (Dr. D) – – – – – – Hyperventilation Vasovagal Attack – (vagus nerve stimulated – brief syncope) Cardiac Dysfunction Anxiety/Panic Attacks Lab values (hypoglycemia or hyponatremia [low NA+]) Drug Toxicity (Dilantin causes nystagmus) The Big Four Problems • Unilateral Vestibular Hypofunction (Peripheral Disorder) • Bilateral Vestibular Hypofunction (Peripheral Disorder) • BPPV (Peripheral Disorder) • Central Vestibular Disorder (CVD) Need to differentiate which of these the patient has for effective treatment. Reminder: One patient can have more than one of these at the same time. (For example, BPPV common in women beginning in 4th and 5th decades of life. A 49 year old female may have an underlying BPPV and then have a pontine stroke leading to positive results for both BPPV and CVD. Central • Causes: – – – – – – – – – – – Brainstem and cerebellar lesions Demyelinating diseases Epilepsy Head injury Motion Sickness Structural Malformation (Arnold Chiari) Post Concussive Syndrome Trauma Tumor (Posterior Cerebrum or Cerebellar) Vascular insufficiency Vestibular migraine 2 Central • Hx: – – – – Persistent Other Sx and complaints Vague Symptoms Symptoms occur more often and are more lingering. • Tests: – – – – – Smooth Pursuit Saccades VOR Cancellation Slow VOR Gaze Stabilization (Can be Peripheral or Central – Central does NOT follow Alexander’s Law) Peripheral Dysfunction • Three types: – Unilateral Vestibular Hypofunction – Bilateral Vestibular Hypofunction – BPPV (technically a Peripheral Disorder but think of it as an entirely different entity) Central Peripheral • History: • Findings: – Purely horizontal or vertical nystagmus – Nystagmus that changes direction (does not follow Alexander’s Law) – Often diffuse balance difficulty – Unremitting positional nystagmus (peripheral disorders nystagmus with stop in 2-3 minutes) – – – – – Involves vertigo (“spins”) Sx triggered by change in head position or head movement Sx fluctuate Sudden onset Can include vestibular crisis • Tests: – – – – Head Thrust Head Shaking Dynamic Visual Acuity Gaze Stability – follows Alexander's Law Central • Plan of Care – 1-3 visits per week for 8 – 15 weeks (depending on setting and co-morbidities) – Goals: • Habituation exercises for rehabilitation of system. • Substitution exercises in case of permanent disaiblity. – D/C: • HEP • modifications for lifestyle and safety. – Prognosis: • Dependent upon severity. Peripheral • Causes: – – – – – – – – – Barotrauma BPPV Cervical vertigo/cervicogenic dizziness Meniere’s Disease Perilymphatic fistula Ototoxic drugs Toxic chemicals Tumor (Acoustic neuroma or vestibular schwaroma) Vestibular Neuritis 3 Peripheral • Findings: – Nystagmus follows Alexander’s Law – Impaired VOR (key for peripheral dysfunction) – BPPV Peripheral – Bilateral Vestibular Hypofunction: • Treatment: – Determine if this is a complete loss or incomplete loss. • Complete loss = Substitution Exercises • For incomplete loss Return to unilateral treatment. – Gait Training – Functional Activities • Will have difficulty flying planes, riding bikes or swimming (especially in murky water). • Utilize night lights at home. – Bilateral Complete Loss will not get better • Teach to move slower, limit head and body movement. • Move eyes, then head and finally turn body when turning. • Train remaining balance systems (somatosensory and vision) Peripheral – Unilateral Vestibular Hypofunction • Treatment: – Adaptation – retraining of the system • Goal: gaze stability to see clearly with head movement and “postural control under static and dynamic conditions” • VOR x 1 VOR x 2 (know how to progress) • Balance Exercises, Functional Activities and HEP – Motion Sensitivity: • Can use Motion Sensitivity Quotient to determine symptoms that provoke individual patient. – – – – Sx should last less than a minute. Do not perform another movement until Symptoms dissipate. Change speeds of movements. Do not overstimulate. Unilateral Peripheral • POC: – Approximately 1-2 visits per week for 4 to 8 weeks – Goal: Rehabilitation of system – D/C: • HEP • Activities involving head motion • Prognosis: – Excellent prognosis – Return to PLOF Peripheral – Bilateral Vestibular Hypofunction • POC: – 1-3 visits/week for 8 – 15 weeks – Goal of substitution for missing vestibular system and training visual/somatosensory systems. – D/C: • Will most likely need modifications of lifestyle for safety – Night lights, reflective stickers for stairs. • Prognosis: – Fair to return to PLOF. Peripheral: Benign Paroxysmal Positional Vertigo (BPPV) • Considered a “Peripheral nystagmus but best to think of it as a third entity” • Fun Facts: – If it is truly BPPV, nystagmus with stop. – 48% of those with otologic cause of dizziness is BPPV – Found in approx ½ population over 65 y/o. – Most individuals require 3-5 physician visits before they are properly diagnosed. – Sx remit with one treatment approx. 85% of time. 4 Peripheral - BPPV Peripheral - BPPV • Clinical Assessment: • Occurs when the “crystals” are displaced into the semi-circular canals. • This gives a false sense of vertigo secondary to head position and can cause dizziness and nausea. • Can be spontaneously • May follow head trauma, labyrinthitis or ischemia in the vestibular system. – Dix-Hallpike (Test for Anterior and Posterior Canals) – Sidelying Test (Test for Ant/Post canals for patients unable to handle cervical extension) – Notes: Peripheral - BPPV Peripheral - BPPV • Physiology: (6 types) – Must distinguish to treat correctly. – Cupulotithiasis: The otoconia are held to the cupula of one of the SCC. • Anterior Canal • Posterior Canal • Horizontal Canal – Canalithiasis: The otoconia are free floating in the canals within the endolymph. • Anterior Canal • Posterior Canal • Horizontal Canal Peripheral - BPPV • Classic Symptoms: – Brief episodes of vertigo (true spinning) – typically less than 1 minute – may be longer with trauma. – Associate with changes in head position relative to gravity. • Lying down, raising from horizontal orientation, rolling over in bed. • Bending over • Looking up. • Associated Symptoms: – – – – Sense of imbalance (>50% of patients) General Motion Sensitivity Anxiety Restriction of Movement • Typical Nystagmus – Latency of 1 – 30 seconds. (if it occurs right away, it is probably not BPPV) – Duration generally < 1-2 minutes » Canalithiasis < 60 seconds » Cupulolithiasis > 60 seconds. – Fatigues – If it does not fatigue it is not BPPV. – Involved side will have stronger nystagmus and patient will c/o vertigo. • Eye Movements for Anterior and Posterior Canal : – Posterior: canalith or cupulolisthiasis torsional nystagmus toward involved side (99% downward ear) and up-beating. – Anterior : canalith or cupulolisthiasis torsional nystagmus toward involved side (99% downward ear) and down-beating. – Central Disorder = Positional nystagmus occurs immediately and does not fatigue! Symptoms do not decrease with repeated maneuvers. Peripheral - BPPV • Treatment in Anterior and Posterior Canals: (Canal and Cup) – Goal: Return otoconia to the vestibule via vestibular maneuvers. – Determine which canal is involved to perform the correct manuever. – Re-test if time allows. – Pt. Education is KEY! – • Provide post-maneuver instructions is essential to successful treatment. – Follow up with patient after 48 hours to 1 week. – Progress to balance training and habituation if needed. – Encourage pt. to return to daily activity involving head motion after precautionary period is reached. – Treat BPPV 1st – once you fix this other co-morbidities won’t be as bad (i.e. balance or anxiety) 5 Peripheral - BPPV • Treatment Maneuvers: – Ant/Post Canalithiasis: • Best: Canal Repositioning Technique (CRT) (AKA Modified Epley or Canal Repositioning Maneuver (CRM) • Other options: – Brandt-Daroff exercises – Self CRT – Ant/Post Cupulolithiasis: • Best = Liberatory Maneuver • Other option = Brandt- Daroff Exercise Peripheral - BPPV • Treatment of Horizontal Canalithiasis – Bar-B-Que Roll / Log Roll • AKA Lempert Maneuver or modified CRT – Forced Prolonged Position (FPP): Patient instructed to lie in sidelying with unaffected ear down for 8 – 12 hours – Best practice to use FPP following BBQ roll. – Liberatory maneuver (AKA Appiani) • Treatment of Horizontal Cupulolithiasis: – Rapid BBQ roll – Liberatory maneuver for horz. Cup (AKA Casani) Peripheral - BPPV • Post Maneuver: – Instructions: • Avoid sleeping on involved side • Sleep with an extra pillow • Avoid extreme head positions. – Protocol: • Provide patient education regarding BPPV. The more they understand, the better outcomes you have. • If BPPV is bilateral, completely treat one side before addressing other. • Teach self CRT or Brandt-Daroff exercises if appropriate. • Address secondary issues after BPPV addressed (balance, central dysfunction, etc.) Peripheral - BPPV • Post Maneuver Instructions – Do not bend over, move head up or down or tilt head to either side for rest of day. – Avoid sleeping on involved side – Sleep with an extra pillow – Avoid extreme head positions. Peripheral - BPPV • Evaluating Horizontal Canal (Lateral Canal) BPPV: – Evaluation: Roll Test – Horizontal Canalithiasis: (Horizontal Geotrophic) • Nystagmus beats toward downward ear/ground* most common. • You will see nystagmus when testing both ears. • Involved side will have stronger nystagmus. • Nystagmus fatigues. – Horizontal Cupulolithiasis (Horizontal Ageotrophic) • • • • Nystagmus beats away from downward ear You will see nystagmus when testing both ears. Involved side will have weaker response. Nystagmus persists. (Exception to the Rule: Only test in which nystagmus persists and it does not mean central disorder) Vestibular - Evaluation • Other Tests: Can be used with Central, BPPV and Peripheral signs. – Balance Tests and Measures: • • • • • Static Standing: NBOS, Rhomberg, SLS, etc. Sensory Integration: Modfied CTSIB Reactive Balance: Nudge or posterior tug test Reduction in limits of stability: functional reach < 10” Anticipatory Balance: picking up objects, getting out of chairs. – FGA, DGI, modified CTSIB, BERG, 10 meter walk test. – Outcome Measures: • Motion Sensitivity Quotient (MSQ) • Dizziness Handicap Inventory (DHI) • Activities-Specific Balance Confidence Scale (ABC) – Fuduka Step* - The cheat test – This will tell you which side the impairment is on. Patient will turn to side of impairment with vestibular impairment. If they move more than 20 inches, they are unable to ambulate in the dark. 6 Vestibular Lab: Eval 1. Occular ROM/Smooth Pursuit (Central) – Pen 18 – 24” from face – Have patient follow with eyes, without moving head. – Test in all planes (horizontal, vertical and diagonal). – Watch both eyes move together (smoothly) through full ROM. – Abnormal: eyes moving in jerking or saccadic fashion, eyes not staying together, decreased ROM, nystagmus (note presence of nystagmus and direction) – Reminder: have patient focus on cap of highlighter/marker to give a single point Vestibular Lab: Eval 5. Slow VOR (central test) – Grasp patients head with both hands on either side of temples – (do not grab jaw) – flex patient’s head 20 – 30 degrees. – Instruct patient to focus on target (your nose) and slowly rotate patient’s head from side to side and then up and down. 4 Hz or 20 head turns in 10 seconds. – Watch to make sure your patient’s eyes maintain gaze on target. – Normal Result: Patient able to focus on therapists nose. – Abnormal Test: Patient cannot maintain gaze or closes eyes, c/o of dizziness. Vestibular Lab: Eval 2) Gaze Holding (central or peripheral) – Hold pen at approx. 25% before end or range and observe for nystagmus in all directions. – Do not go to end range – This can cause nystagmus normally (false positive) – Abnormal Test: Direction changing nystagmus or purely vertical nystagmus is a central sign. – Abnormal test: Horizontal nystagmus consistently beating in same direction with increased intensity toward direction of nystagmus (Alexander’s Law) = peripheral sign. Vestibular Lab: Eval 6. Rapid VOR/Halgami Head Thrust (peripheral test) – Begin with slow VOR. – Without telling patient, rapidly thrust patient’s head to one side and hold. – Watch to make sure patient’s eyes maintain gaze on target (therapist’s nose). – Resume slow VOR and then randomly perform head thrusts to either side (multiple times each for confirmation) – Do no make a pattern so patients do not have a false negative with anticipating your movements. – Normal result: Pt. will maintain gaze fixation/ no c/o of dizziness. – Abnormal result: Unable to maintain gaze or saccade seen to correct gaze. Note side head thrust in – this is the involved side. Vestibular Lab: Eval Vestibular Lab: Eval 3. Vergence (Central Test) – – – Hold pen approx. 24” in front of patient and ask to focus on pen while you move it toward their nose. Normal: Eyes should converge and pupils constrict – double vision is normal near nose. Abnormal result: Eyes moving at different speeds (possible CN injury). 4. Saccades: (Central Test) – – – – Hold 2 pens (or pen and therapist nose) one centered and other approx. 6 – 10 inches horizontally, vertically and diagnoally. Ask patient to look from one target to another testing all directions and repeating several times. Normal: Eyes should move smoothly between targets without stopping or overshooting. Abnormal Result: More than 2 eye movements required to get to target or over shooting or under shooting target consistently. 7. VOR Suppression/Cancellation Test (central) – – – Ask the patient to fixate and track a small target that moves synchronously with head movement. Normal: subjects eyes stay focused on target without difficulty. Abnormal: “catch-up” saccades or nystagmus – unable to suppress VOR reflex. 8. Dynamic Visual Acuity Test (Peripheral Test) – – – Have the patient read an eye chart with clinician performing a slow VOR on patient. Normal: 1 -2 line difference in acuity or no change. Abnormal: A 3 or more line decline 7 Vestibular Lab: Eval 9. Dix-Hallpike (BPPV) – Passively turn patient’s head 45 degrees while sitting in long sitting. – Move patient into supine with head extended rapidly. – Nystagmus seen 1 - ~30 seconds after positional movement. Vertigo and nystagmus will fatigue if truly BPPV. Vestibular Lab: Treatment • Adaptation continued: – Gaze stabilization • Use with impaired smooth pursuit or saccades. • Have patient practice whichever tests are impaired multiple times per day. • What you may see in my charts: – – – – Circles Sheet b, p, q, d sheet Where’s Waldo? How to progress? Vestibular Lab: Eval 10. Roll Test (BPPV) – Perform head thrust in supine with head flexed approximately 20 – 30 degrees. – Horizontal Canalithiasis: (Horizontal Geotrophic) • • • • Nystagmus beats toward downward ear/ground* most common. You will see nystagmus when testing both ears. Involved side will have stronger nystagmus. Nystagmus fatigues. – Horizontal Cupulolithiasis (Horizontal Ageotrophic) • • • • Nystagmus beats away from downward ear You will see nystagmus when testing both ears. Involved side will have weaker response. Nystagmus persists. (Exception to the Rule: Only test in which nystagmus persists and it does not mean central disorder) Vestibular Lab • Substitution • For use when adaptation does not work or bilateral complete loss. – Imaginary Target Viewing: • Focus on a target close eyes turn head open eyes Focus on new target. • Repeat in multiple directions. – Viewing Between 2 Targets: • To focus on new object, look with eyes first then head then body (if needed) • Repeat in different directions. • Progress: add walking, unstable surfaces, etc. Vestibular Lab: Treatment Vestibular Lab • Adaptation Exercises: – VOR x 1 • Can be used with Unilateral Vestibular Hypofunction or incomplete bilateral hypofunction. • Pt. flexes head 30 degrees and focus on thumb approximately 3 feet away. • Pt turns head as if shaking head no (horizontally) to each side. • Repeat Vertically. (as if shaking head yes) • Goal to perform quickly (approximately 4 times a second.) – How to adapt: • Vary speed of movement (too hard go slower), vary distance. • Progression: add foam, change position of feet, walking, etc. • Habituation: – Base of what provides symptoms for patient (can use MSQ to help) – Start with tolerable exercises – Repeating motion should improve tolerance of that situation. – Progress based on response/patient tolerance. – VOR x 2 • Same conditions as VOR x 1 except add target to move in opposite direction as head 4x per second. • Repeat vertically. 8 Balance Activities • Squats on BOSU Squats on Dynadiscs (progress with eyes closed) • ½ roll leg swivels (progress to eyes closed) • ABCs [NBOS SLS Airex NBOS Airex SLS Eyes closed (EC) NBOS EC SLS Airex EC NBOS Airex EC SLS] • Ball Toss [ NBOS SLS Airex NBOS Airex SLS] Case Study Negative • Smooth Pursuit • Vergance • Sacaddes • Gaze Stability • Slow VOR • Head thrust • VOR Supression BPPV Treatment Maneuvers • • • • • Canalith Repositioning Technique* Self CRT Brand-Daroff Exercises for BPPV Semont or Liberatory Maneuver BBQ Roll/Log Roll How I would treat • CRT or Epley • VOR x 1 VOR x 2 • Balance Ther Ex – Remember: 28 year old dancer – start fairly high up • Probably start with eyes open vs. closed since she moved up 4 feet with eyes closed. References Case Study • • 28 y/o female H/o frequent ear infections as child, failing hearing tests for low sounds in teens, dizziness disturbances with changes in head position. Does not like swimming secondary to pain in ear when submerged in water. Balance generally good to general pop, however, patient was a dance minor and reports had worst balance in program. (habituation) Reports occasionally has headaches and at times has sensitivity to sound. Can have nausea with headaches associated with loud noises. Cannot remember the last time she hasn’t had aural fullness in left ear. + for tinnitus in Left 1-2 times a week, occasionally will have it in right. • What are you leaning towards based on history? • • • • • Positive • Fuduka step – 4 feet forward and 45 degree left turn. • Rapid VOR – reports dizziness after 10 seconds. • Dynamic Visual Acuity – change greater than 3 lines. • And test on next slide. • Heather Dillon Anderson, PT, DPT, NCS 4 weeks of notes from Neumann University/ Good Shepherd Penn Partners Vestibular Specialist – Referenced Following Lectures: • • • • • • • • • • • • • Vestibular Rehabilitation 5/19/2012 PT 737 Vestibular Examination and Interventions 6/2/2012 PT 737 Evaluating and Treating BPPV 6/9/12 PT 737 Vestibular Lab 1: 6/2/2012 PT 737 Vestibular Lab 2: Vestibular BPPV Lab 6/9/2012. PT 737 Various websites included in slides for definitions only. Youtube for vestibular anatomy videos and Alexander’s Law videos. Herdman, Susan. Vestibular Rehabilitation. Third Edition. Philadelphia, PA. FA Davis Co, 2007. Farrel, L. Peripheral Versus Central Disorders. Neurology Section Fact Sheet. American Physical Therapy Association. www.APTA.org Accessed 1/31/14. Lowrie, M. Vestibular Disease: Anatomy, Physiology and Clinical Signs. Compendium: Continuting Education for Veterinarians”. July 2012. Umphred, Darcy. Neurologic Rehabilitation, fourth edition. Mosby, St. Louis, MI. 2001. Zapanta, P. Vestibular Rehabilitation. Emedicine.medscape.com/article/883878-overview. Accessed 1/31/14. Updated March 12, 2012. Thompson, T and Amedee, R. Vertigo: A Review of Common Peripheral and Central Vestibular Disorders. Ochsner Journal. 2009 Spring; 9(1): 20-26. 9