Post San Antonio Breast Cancer Symposium Briefing
advertisement

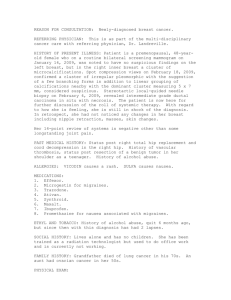
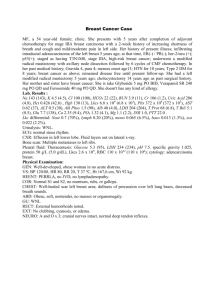
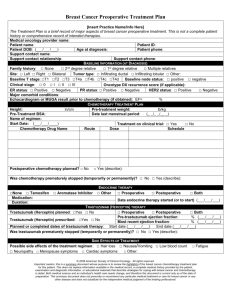
Post San Antonio Breast Cancer Symposium Briefing 時間:2013年1月5日(六)地點:澄清醫院 時間 12:50 | 13:00 13:00 | 13:40 13:40 | 14:20 14:20 | 15:00 15:00 | 15:20 15:20 | 16:00 16:00 | 16:40 16:40 | 17:20 17:20 | 18:10 18:10 | 18:20 議程 講師 俞志誠 理事長 Opening 臺灣乳房醫學會 曾令民 醫師 Targeted Therapy: Update 臺北榮總 楊陽生 醫師 Chemotherapy: Update 台中榮總 王惠暢 陳達人 陳偉武 醫師 Hormonal Therapy: Update 台大醫院雲林分院 Break Screening and Molecular Image of Breast Cancer Local Regional Treatment for Breast Cancer Advances in Basic Breast Cancer Research Summary of SABCS 2012 Discussion & Closing 葉名焮 主任 中國附醫 陳火木 主任 台北市立聯合醫院 戴明燊 醫師 陳守棟 葉大成 三軍總醫院 郭文宏 醫師 台大醫院 張金堅 院長 澄清醫院 摘要及CV 講師 CV 曾令民醫師 學歷 國防醫學院醫學系 經歷 台北榮民總醫院一般外科主治醫師 國立陽明大學醫學院 外科助理教授 美國德州休士頓 MD Anderson 癌病中心研究員 台灣乳房醫學會秘書長 台灣癌症臨床研究合作組織乳癌研究委員 楊陽生醫師 學歷 中國醫藥大學醫學系畢業 經歷 台中榮民總醫院血液腫瘤科總醫師 台中榮民總醫院血液腫瘤科主治醫師 陳偉武醫師 學歷 臺北醫學大學醫學系畢業 經歷 台大醫院腫瘤醫學部總醫師 台大雲林分院腫瘤醫學部主治醫師 葉名焮醫師 學歷 國立陽明大學醫學系醫學士 英國南安普敦大學 腫瘤暨免疫治療醫學博士 英國南安普敦大學 癌症科學研究員 經歷 中國醫藥大學附設醫院乳房外科主治醫師 高雄榮民總醫院一般外科主治醫師 台灣乳房醫學會 監事 陳火木主任 學歷 台灣大學醫學院畢業 經歷 台大醫院外科總醫師 台北市立聯合醫院婦幼院區主治醫師 台北市立聯合醫院婦幼院區外科主任 台北市立聯合醫院婦幼院區乳房外科專任主治醫師兼任乳房外科部部長 戴明燊醫師 學歷 英國倫敦大學皇后瑪麗學院癌症研究中心 博士班畢業 經歷 三軍總醫院血液腫瘤科總醫師 三軍總醫院內科部總醫師 國防醫學院醫學系 內科學科助理教授 郭文宏醫師 學歷 國立台灣大學醫學系畢業 國立臺灣大學醫學院臨床醫學研究所博士班 經歷 台大醫院一般外科專任主治醫師 國立台灣大學醫學院臨床助理教授 課程摘要 Targeted Therapy: Update Advances in systemic therapy over the last 40 years have significantly improved outcomes for breast cancer patients as a whole, but we are still in the beginning stages of being able to optimize treatment for individual patients. This task centers on 2 questions: who should receive therapy, and which therapy will give the best results. The initial question is especially problematic in patients with minimal disease (T1a,bN0M0), many of whom have an excellent prognosis and would do well with local therapy alone. The second question requires an understanding of complex biochemical pathways by which individual cells might respond to a particular drug. A number of presentations at the 2008 SABCS addressed 1 or both of these questions. HER2 STATUS IN EARLY-STAGE DISEASE HER2 is correlated with poorly differentiated tumors, a high proliferation rate, and poor outcomes. Ronjay Rakkhit,MD, from the University of TexasM.D. Anderson Cancer Center presented results from a study looking at HER2 positivity as a prognostic factor in 965 patients with T1a,bN0M0 breast cancer at a median follow-up time of 74 months.18 Of these patients, 77% were hormone- receptor positive, 13% were triple negative (TN), and 10% were HER2-positive. Patients were excluded from the study if they had received chemotherapy or trastuzumab. A validation set of 350 cases with the same inclusion criteria and a similar median follow-up time was obtained from collaborators at other institutions. Both RFS and distant recurrence-free survival (DRFS) were significantly worse in patients with HER2-positive disease (P<.0001). After adjustment for hormonereceptor status, age at diagnosis, tumor grade, and tumor stage, HER2 status remained a significant prognostic indicator in this patient group, with a HR of 2.68 for RFS (P=.0002) and 5.30 for DRFS (P=.0002). A preliminary analysis of the cases from the other institutions showed a significant difference in 5-year RFS (87.4% for HER2-positive vs 97% for HER2-negative, P=.043) but not for 5-year DRFS (92.3% and 97.0%, respectively; P=.449). However, this second analysis was based on only 10 events, compared with 106 events in the M.D. Anderson group. These data suggest that patients with early-stage, node-negative breast cancer, who are HER2 positive, may have a poor prognosis, and should be considered for treatment with anti-HER2 therapies. PREDICTORS OF RESPONSE TO ANTHRACYCLINES The anthracyclines have proven to be powerful additions to the chemotherapy armamentarium, but they can have severe side effects. Thus, markers for treatment response to anthracycline therapy would be of considerable value. HER2 and topoisomerase-2 (TOPO2) have been implicated in response to anthracyclines in previous studies, but the results have been mixed. These genes are located on chromosome 17, which also contains other genes associated with breast cancer, including BRCA1 and TP53. In addition, polysomy 17 is a frequent event in breast cancer cells. John M.S. Bartlett, PhD, from the Endocrine Cancer Group at Edinburgh University presented the results of a study examining HER2 amplification, TOPO2 amplification and deletion, Ki67, and chromosome 17 polysomy as prognostic and predictive markers in the UK National Epirubicin Adjuvant Trial (NEAT).19 This trial compared the efficacy of epirubicin followed by CMF compared with CMF alone.Of the patients randomized in the NEAT study, 819 patients in the CMF arm and 806 patients in the CMF plus epirubicin arm were available for this study. In this patient group, HER2 amplification or 3+ positivity and TOPO2deletion were strongly prognostic for poor RFS and OS (P<.001), but no individual marker showed a significant predictive value for response to anthracycline treatment. On the other hand, polysomy 17 had a significant treatment interaction (HR=0.59, P=.04), and patients with tumors polysomic for chromosome 17 had significantly greater benefit from anthracycline This raises the possibility that the unifying predictive marker for anthracycline response may be polysomy 17, rather than HER2 or TOPO2, perhaps as an indication of chromosome nstability. The authors also suggest that previous studies examining the usefulness of HER2 and TOPO2, some of which reported a strong association between these markers and anthracycline response, may have been underpowered Addressing this possibility, Angelo Di Leo, MD, PhD, and coworkers from the HER2-TOPO2Meta-Analysis Study Group conducted a meta-analysis of phase 3 trials examining anthracycline-based therapy with CMF in early-stage breast cancer patients with available primary tumor samples. The studies included were the Belgian 3-arm trial, the Canadian NCIC CTG trial, the Danish DBCG trial, and the UK NEAT trial. The planned interim analysis presented at the 2008 SABCS included 1944 patients.20 The results of the meta-analysis show that HER2 and TOPO2have a modest and statistically borderline value in predicting sensitivity to anthracyclines. A caveat attached to this study is the lack of reproducibility in TOPO2scores by FISH in 30.8% of cases submitted to a central lab for verification. In addition, the patient groups used for this analysis were highly heterogeneous with regard to systemic therapies and patient/tumor characteristics. Importantly, thisanalysis currently includes only about one-third of the eligible patients from the UK NEAT trial (590/1625). The final analysis for this study will be done when the remainder of these patients are incorporated. Since HER2 and TOPO2showed no treatment interaction with anthracyclines in the Bartlett study, it is likely that the final analysis will show a reduction in the already borderline value of HER2 and TOPO2for the prediction of anthracycline response. Chemotherapy: Update Taxanes in adjuvant chemotherapy The taxane drugs, which block cell cycle progression by stabilizing microtubules, were originally developed for use as cross-over therapy in patients who failed to respond to standard chemotherapy regimens containing doxorubicin/epirubicin and cyclophosphamide. They are now routinely used in combination with these drugs as adjuvant treatment for patients with node-positive primary breast cancer. One study presented SABCS showed results from a first-generation trial investigating the efficacy of docetaxel in a specific subgroup of intermediate risk patients, and 2 studies presented results from second-generation trials designed to optimize dosing of docetaxel for node-positive patients with operable breast cancer. Hormonal Therapy: Update Because of their demonstrated efficacy in the prevention of both recurrences and new primaries, as well as their favorable side-effect profiles compared with chemotherapy, increasing interest has focused on the use of hormonal agents for systemic adjuvant therapy in hormone-receptor–positive women. The “gold” standard in this category is the selective estrogen response modifier, tamoxifen. For postmenopausal women, the third-generation aromatase inhibitors (AIs) have compared favorably with tamoxifen in terms of survival outcomes, but present a very different side-effect profile. Several studies presented at the 31st Annual San Antonio Breast Cancer Symposium (SABCS) presented outcomes of randomized trials comparing tamoxifen and AIs, examined quality of life (QoL) measurements associated with the 2 drug regimens, and investigated whether the addition of an agent that interacts with the human epidermal growth factor receptor 2 (HER2) pathway can increase the clinical efficacy of an AI. Comparing tamoxifen with AIs Tamoxifen Exemestane Adjuvant Multinational (TEAM) prospective randomized phase 3 trial in hormone- sensitive postmenopausal women with earlystage breast cancer.1 This study was originally designed to compare tamoxifen as monotherapy with the AI exemestane as monotherapy, but the study design was later amended to evaluate sequential therapy with 2.5 to 3 years of tamoxifen followed by exemestane compared with exemestane as monotherapy for 5 years. The analysis presented by Dr Jones focused on tamoxifen vs exemestane as monotherapy at 2.75 years, which marked the average time of crossover to exemestane. In comparison with the tamoxifen/ exemestane arm, the exemestane only arm showed a trend towards improved disease-free survival (DFS) (hazard ratio [HR]=0.89; adjusted log rank P=.12) and a significant improvement in relapse-free survival (RFS) (HR=0.85; P=.05) and time to distant metastasis (TDM) (HR=0.81; P<.03). Because early discontinuation from tamoxifen occurred at a high rate, a separate analysis looked at endpoints only in preswitch patients who were verified to be in compliance with their drug regimens. This analysis showed a significant benefit in DFS for patients in the exemestane arm (HR=0.83, adjusted log rank P=.02) Gynecologic adverse events, hot flashes, and thromboembolic events were significantly more common in the tamoxifen/ exemestane arm, while patients receiving exemestane alone were more likely to experience hypertension and musculoskeletal events, including arthralgia, arthritis, and osteoporosis. There were no significant differences between treatment groups in cardiac events or reported fractures. Results of a meta-analysis of studies involving monotherapy with the third-generation AIs anastrozole, exemestane, or letrozole compared with tamoxifen were reported by James Ingle, MD, from the Aromatase Inhibitors Overview Group.2 For this analysis, cohort 1 contained studies in which all drugs were given as monotherapy for 5 years, and used results from the ATAC and BIG 1-98/IBCSG 18-98 trials. Cohort 2 contained studies in which AIs were given in sequential therapy after 2 or 3 years of tamoxifen, and used results from the GABG/ARNO, IES/BIG 2-97,ITA, and ABCSG VIII trials. Cohort 1 included 9856 patients at an average follow-up time of 5.9 years. Patients receiving AIs for 5 years showed a superior benefit in recurrence rate compared with patients receiving tamoxifen at follow-up times of 5 years (9.6% vs 12.6%) and 8 years (15.3% vs 19.2%) (logrank 2 P<.00001.) There were no significant differences between treatment groups in breast cancer mortality, death without recurrence, or any death. Cohort 2 included 9015 patients at an average follow-up time of 3.9 years. Again, there was a significant benefit in recurrence rates associated with using AIs. Patients switching to AIs showed lower recurrence rates compared with patients receiving tamoxifen alone at 5 years (5.0% vs 8.1%) and 8 years (12.0% vs 16.1%) (log rank 2 P<.00001) Compared with patients who switched to an AI for the last 3 to 5 years, patients receiving tamoxifen alone had significantly higher rates of breast cancer mortality and death from any cause, and a trend towards higher death without recurrence. However, the absolute difference in mortality rates was low (1.6% at 6 years for breast cancer mortality, 0.7% for death without recurrence, and 2.2% for any death). In particular, there was minimal association of any treatment strategy with nonbreast- cancer–related death, suggesting that the regimens are generally safe. In both cohorts, there appeared to be little benefit in extending treatment beyond 5 years, questioning the value of longer AI therapy. QoL issues associated with hormonal therapy Although most trials are now showing a fairly consistent picture of improved clinical outcomes with AIs com pared with tamoxifen as adjuvant therapy, these drug modalities have very different adverse event profiles. Thus, although recurrence rates or survival might be improved with AIs, drug compliance might be affected by QoL issues, especially given the extended treatment periods that are used for hormonal therapies.Janine van Nes, on behalf of the TEAM trial, presented results of a QoL study on a subset of 742 patients participating in this trial.3 QoL was assessed at 1 year and 2 years after randomization, using the European Organization for Research and Treatment of Cancer (EORTC) QLQ C30 and the EORTC BR23 questionnaires supplemented with Functional Assessment of Cancer Therapy Endocrine Subscale (FACT-ES). The QLQ C30 assesses functional skills, symptoms, and global health status. The BR23 was especially formulated for breast cancer patients; for this study, questions related to chemotherapy symptoms (eg, hair loss) were excluded. There were no significant differences in global health status/QoL between different treatment times, treatment arms, or in the interaction between treatment time and treatment. Patients receiving tamoxifen showed improved emotional and sexual functioning and decreased fatigue, dyspnea, and insomnia compared with patients receiving tamoxifen and exemestane, while patients receiving both drugs showed improvement in future perspective and arm symptoms compared with patients receiving tamoxifen alone. The only clinically relevant difference between the 2 treatment groups was increased insomnia in the groups receiving both drugs vs the group receiving tamoxifen alone Shozo Ohsumi, MD, PhD, and colleagues from the NHO Shikoku Cancer Center in Matsuyama, Japan, initiated a study assessing health-related QoL and psychological distress in patients from the NSAS BC03 trial.4 For this trial, recurrence-free postmenopausal breast cancer patients who had received tamoxifen for 1 to 4 years after surgery were randomized to continue tamoxifen or to switch to anastrozole for the remainder of a 5-year period. Patients were asked to complete patient-administered instruments—FACT-B (breast cancer scale),FACT-ES (endocrine symptom scale), and CES-D(Center for Epidemiological Studies Depression scale)— at baseline (randomization) and at 3 months, 1 year, and 2 years after randomization. The total scores in FACT-G and FACT-ES and the scores of the FACT-G physical well-being subscale were significantly better in the tamoxifen group compared with the anastrozole group (P=.042, .038, and .005, respectively). Total scores in FACT-B were marginally better in the tamoxifen group. There were no significant differences in scores from the CES-D scales or in other subscales of any of the FACT instruments. Several individual items in the FACT-ES scale showed significant differences between the 2 treatment groups. Hot flashes and vaginal discharge were worse in the tamoxifen group, while dizziness, diarrhea, and headache were worse in the anastrozole group. These results indicate that patients continuing on tamoxifen may have a slightly better health-related QoL than patients switching to anastrozole. Combining a HER2 pathway inhibitor with an AI Current endocrine therapies for metastatic breast cancer are limited by de novo or subsequent acquired resistance. Because cross-talk between growth factor and steroid receptor pathways has been implicated in this endocrine resistance, Stephen Johnston, MD, and colleagues initiated the EGF30008 trial to see if the addition of lapatinib to the AI letrozole would improve outcomes in postmenopausal women with hormonereceptor– positive metastatic breast cancer.5 Lapatinib is a small molecule tyrosine kinase inhibitor that competes with ATP for binding to specific tyrosine residues in the intracellular catalytic kinase domain of the HER2 molecule, inhibiting the downstream reactions in the pathway. Dr Johnston presented the first results from the EGF30008 trial at the 31st Annual SABCS. The trial included 1286 patients randomized to oncedaily treatment with lapatinib and letrozole or letrozole and placebo. Of the total, 219 patients were HER2- positive by immunohistochemistry or FISH. Median progression-free survival (PFS) in this subgroup was significantly increased in the patients receiving lapatinib plus letrozole compared with patients receiving letrozole alone (8.2 months vs 3 months, respectively; HR=0.71, P=.019) There was no significant difference between treatment arms in the HER2negative patient group. The benefit of adding lapatinib was confirmed for the HER2-positive patients by multivariate analysis using a pre-planned Cox regression, with age, ECOG status, and serum baseline HER2 extracellular domain measurement as covariates. Overall response rate was also significantly increased in the HER2-positive population receiving lapatinib plus letrozole vs letrozole alone, but there was no difference between treatment arms in the HER2-negative patients.The combination of drugs was well tolerated. The results of this study demonstrate that lapatinib can significantly improve the clinical efficacy of letrozole in patients with known HER2-positive, hormone-receptor–positive metastatic breast cancer. Screening and Molecular Image of Breast Cancer FUNCTIONAL/MOLECULAR IMAGING Breast imaging can provide several types of information. Screening information allows the detection of cancer in asymptomatic individuals. Diagnostic information can improve patient outcome by improving selection for breast conserving surgery, refining the definition of tumor extent and thereby reducing reexcision rates, synchronously identifying contralateral cancer, and decreasing the rate of local recurrence. Treatment response information can monitor the effectiveness of a specific therapy, and help in determining when a switch to a different treatment regimen is appropriate. Different imaging modalities vary in how effective they are in supplying these various types of information. Presentations at the 2008 SABCS reviewed the current status of several forms of functional/molecular imaging; that is, imaging that relies on in vivo tumor biology rather than anatomic measurements of the tumor. This includes established technologies (magnetic resonance imaging [MRI] and positron emission tomography [PET] imaging), as well as new approaches to imaging currently under development (dynamic molecular imaging and optical tomography). Magnetic resonance imaging (MRI) Monica Morrow, MD, from Memorial Sloan- Kettering Cancer Center presented an overview of the evidence related to the use of MRI for diagnostic imaging.31 There is no question that MRI finds cancers that are not detected by physical examination, mammography, or ultrasound, and it has always been assumed that finding these MRI-detected cancers had a clinical benefit for the patients.However, this assumption may not be valid. For example, in comparing surgical outcomes in breast conserving surgery between patients who received an MRI compared with those who did not, there were no significant differences in the rate of conversion from breast conservation to mastectomy or in the percentage of patients with positive margins after first excision.32 This is especially noteworthy because the selection of women to receive MRIs is generally biased towards those who would be expected to benefit, for example, younger women, those with dense breasts, patients with lobular carcinoma, or those who had a difficult mammogram. These findings drawn from retrospective studies have been confirmed in the first retrospective study to look at this question, which reported no significant difference in reoperation rates within 6 months in patients who received MRIs compared with those who did not.33 MRIs have also shown no benefit in the detection of contralateral cancer. A recent study by Solin and colleagues34 showed no difference in the incidence of contralateral cancer at a median follow-up of 8 years in patients who received MRIs compared with those who did not. This study also showed no difference in LR rates between these 2 groups (3% vs 4%, respectively; P=.51). In all published series, patients with lobular cancer were not at higher risk for local recurrence, even though more disease was apparent on MRI with lobular carcinoma compared with invasive ductal carcinoma Dr Morrow concluded that neither short-term surgical outcomes nor long-term local control or contralateral cancer rates are improved with MRI, suggesting a questionable patient benefit associated with the increased mastectomy rate found with MRI. There are, however, instances where MRI is of value. This includes: wise occult disease in internal mammary nodes or at distant sites. Routine systemic staging is not indicated for asymptomatic early-stage breast cancer, where the incidence of distant metastases is low and the chance of false positives is very high. In addition, for the type of low-volume axillary disease that we can detect easily with sentinel lymph node biopsy in earlyknown or suspected BRCA1/2 carriers not undergoing mastectomy; presentation as axillary adenopathy with occult primary; assessment of response to neoadjuvant chemotherapy; and in a situation where physical examination, mammography, and ultrasound produce significantly discrepant results. Positron emission tomography (PET) In PET, a positron-emitting radiopharmaceutical (usually fluorodeoxyglucose [FDG]) is injected into the patient. FDG is a tracer of glucose metabolism in metabolically active cells. A scanner collects the pairs of photons that come out of a positron emission and uses these data to reconstruct an image of tracer concentration in quantitative terms. In recent years, PET has been used in combination with CT to allow the simultaneous measurement of anatomic and functional images in the same imaging session. A review of the current status of PET imaging was presented by David Mankoff, MD, PhD, from the University of Washington in Seattle.35 The current clinical applications for FDG PET in breast cancer are for staging of recurrent or metastatic breast cancer and for treatment response assessment. In single-center trials, the sensitivity of FDG PET for systemic staging in recurrent/ metastatic breast cancer has ranged from 85% to 93%, with reasonable specificity that has been improved by the addition of CT One of the areas in which FDG PET has been especially helpful is in the detection of mediastinal lymph node metastases, even in cases that are CT-negative. FDG PET can also be helpful in the detection of lytic bone metastases, but may not be as useful for sclerotic lesions. An emerging clinical application where FDG PET will be very helpful is in the staging of locally advanced breast cancer, where it can identify other Local Regional Treatment for Breast Cancer Sentinel Lymph Nodes Indication for SLNB Pre-operative evaluation and detection Intra-operative assessment Predictive value of sentinel lymph nodes Prediction of the status of Non-SLN Sentinel lymph nodes biopsy after neoadjuvant chemotherapy Evaluation of prognosis by sentinel lymph nodes status Others Pre-SLNB Evaluation and Detection Ultrasound +/- Fine needle aspiration cytology (FNA) CT based lymphatic mapping and localization PET with SPET-CT lymphoscintigraphy Intra-operative assessment and technique SLN number for processing Programmed training Reagents Indocyanine green (ICG) fluoresecence Lymphazurin Blue Touch imprint cytology GeneSearch BLN Assay Meta-analysis UK NEW START training program >80% UK surgeons registered Models of training Mentorship model: for SLNB naïve breast units and surgeons, first 5 cases supervised by an expert trainer in the trainees hospital, SLNB and then ALND for 30 cases Apprenticeship model: for SLNB naïve surgeons in breast units where SLNB was standard of care. 30 cases performed under direct supervision of a NEW ATART accredited trainer, SLNB only 99% localization rate FNR<10% Index quadrant injection technique is easy to learn and is associated with low failed localization and false-negative rates even in inexperienced hands No learning curve was identified for successful sentinel node identification and false-negative rate Identifying multiple SLNs when they exist reduces the false-negative rate. These data suggest that the upper threshold for the number of SLNs that should be removed is 5 Advances in Basic Breast Cancer Research While work continues on optimizing treatment regimens for hormonal and chemotherapy-based adjuvant therapy, there continue to be patients who either do not respond or who develop resistance to these therapies. Targeted biologic agents hold the promise of fine-tuning therapy based on specific attributes of the individualtumor. The first such therapy to come into wide use was trastuzumab (Herceptin®), which targets the HER2 receptor and has shown clinical activity against breast cancers with a mutation of the HER2 gene or an amplification of its gene product. Although trastuzumab administered as a single therapy did not turn out to be the magic bullet that was originally hoped for, it has proven to be very effective when used in combination with other drugs, especially in neoadjuvant therapy. Two papers from the 2008 SABCS presented results from studies where trastuzumab was used in combination with anthracycline-taxane therapy for neoadjuvant treatment of breast cancer patients. TRASTUZUMAB The NOAH (NeOAdjuvant Herceptin) trial is the largest neoadjuvant study to evaluate the addition of trastuzumab to anthracycline- and taxane-based chemotherapy for patients with HER2-positive locally advanced breast cancer (LABC). Primary efficacy analysis of this trial was reported by Luca Gianni, MD, from the Instituto Nazionale Tumori in Milan, Italy.11 Patients were treated with chemotherapy (ATx3, Tx4, CMFx3; n=113) or with chemotherapy and trastuzumab (n=115). A control group of HER2-negative patients with LABC received chemotherapy only (n=99). The primary endpoint was EFS, with a median follow-up time of 3 years. EFS was significantly improved in HER2-positive patients who received chemotherapy and trastuzumab, compared with HER2-positive patients who received chemotherapy only (70.1% vs 53.3%, respectively; HR=0.56, P=.006.) Subgroup analysis showed a treatment advantage for trastuzumab, not only for the entire patient series, but for all subgroups of patients (non-inflammatory vs inflammatory, ER/PgR positive vs ER/PgR negative, clinically node-negative vs clinically node-positive, pCR vs nonpCR OS, a secondary endpoint, was also improved in patients receiving trastuzumab, but the difference was not significant (85.3% vs 80.4%, respectively; HR=0.65, P=.18). EFS was similar in the HER2-positive arm treated with chemotherapy alone and the HER2-negative control arm over the first 18 months, but showed a divergence in favor of HER2-negative patients over a longer period of time. Adverse events from the 2 therapy regimens, including cardiac toxicity, were within acceptable limits. These data support the use of trastuzumab with chemotherapy as a standard treatment option in women with HER2-positive LABC. Professor Gunter von Minckwitz presented results of an integrated meta-analysis of 6402 patients with primary breast cancer receiving neoadjuvant anthracyclinetaxane therapy with or without trastuzumab.12 The integrated meta-analysis was based on individual data from the studies that were included. The analysis defined pCR as no invasive residual disease in the excised tissue of breast and axillary lymph nodes. For HER2-positive patients, the pCR rate nearly doubled in patients treated with trastuzumab plus chemotherapy compared with patients treated with chemotherapy alone. (41.1% vs 22.7%, respectively; P<.001) patients treated with trastuzumab were excluded from the analysis, duration of treatment (> 18 weeks vs 8-12 weeks) was also a significant contributor to increase of pCR rates over time. Patient characteristics associated with a high probability of pCR were: young age, small tumor size, node-negative disease, negative hormone-receptor status, positive HER2 status, and histologic tumor grade. Summary of SABCS 2012 MBC Management and Clinical Trials: Chemotherapy + Targeted therapy when endocrine-therapy is not a choice Outline: Chemotherapy targeted agents, An Update from SABCS Chemotherapy in EBC and MBC Docetaxel adjuvant in EBC (poster) – Cooling gel pad for skin and nail toxicity (poster) Docetaxel + capecitabine vs docetaxel + epirubicin in MBC (poster) CA 163-132: Ixabepillone (poster) HER2 + MBC: to be continued…… HER2 - MBC AVADO: Bevasizumab for first-line ATHENA: Bevasizumab + taxanes (poster) Bevasizumab + paclitaxel (poster) Bevasizumab + Weekly TG (poster) RIBBON-2: Bevasizumab for second-line NU 07B1: Sorafenib + Paclitaxel SOLTI-0701: Sorafenib+ Capecitabine CIRG/TORI 010: Motesanib + Paclitaxel AVADO : Conclusions Updated results confirm the initial analyses Bevacizumab 15mg/kg q3w significantly improves PFS and ORR Limited impact on the known safety profile of docetaxel No difference in OS between study arms Impact of subsequent therapies Bevacizumab use with later lines of therapy may influence OS estimates