swelling mg
advertisement
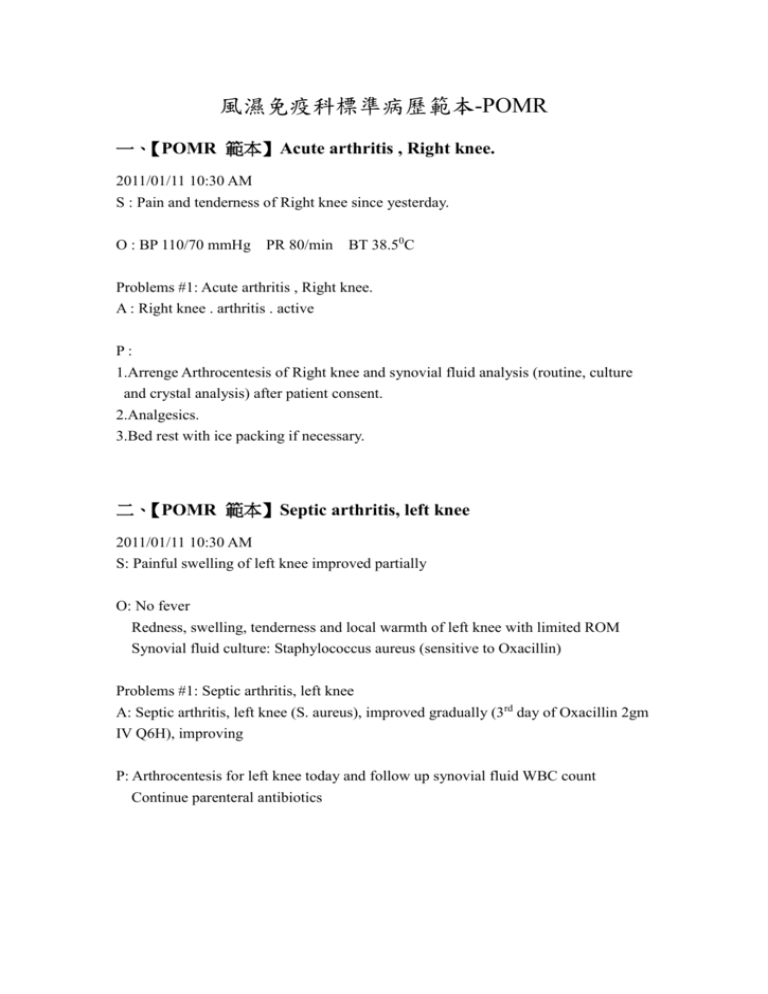
風濕免疫科標準病歷範本-POMR 一、【POMR 範本】Acute arthritis , Right knee. 2011/01/11 10:30 AM S : Pain and tenderness of Right knee since yesterday. O : BP 110/70 mmHg PR 80/min BT 38.50C Problems #1: Acute arthritis , Right knee. A : Right knee . arthritis . active P: 1.Arrenge Arthrocentesis of Right knee and synovial fluid analysis (routine, culture and crystal analysis) after patient consent. 2.Analgesics. 3.Bed rest with ice packing if necessary. 二、【POMR 範本】Septic arthritis, left knee 2011/01/11 10:30 AM S: Painful swelling of left knee improved partially O: No fever Redness, swelling, tenderness and local warmth of left knee with limited ROM Synovial fluid culture: Staphylococcus aureus (sensitive to Oxacillin) Problems #1: Septic arthritis, left knee A: Septic arthritis, left knee (S. aureus), improved gradually (3rd day of Oxacillin 2gm IV Q6H), improving P: Arthrocentesis for left knee today and follow up synovial fluid WBC count Continue parenteral antibiotics 三、【POMR 範本】Gouty arthritis, right ankle 2011/01/11 10:30 AM S: Right ankle pain with difficult walking for one day O: No fever Big tophi at bilateral 1st MTP joint Swelling, local warmth and tenderness of right ankle Synovial fluid analysis: WBC 12000/cumm, MSUM crystal (+) Pending the result of bacterial culture (blood and synovial fluid) Lab: Cr 1.6mg/dl, uric acid 10mg/dl Problems #1: Acute gouty arthritis, right ankle A: Acute gouty arthritis, right ankle, still active joint inflammation P: Bed-resting; ice packing for right ankle(prn) Consult a dietitian for low purine diet education Add colchicine 0.5mg 1# bid, sulindac 200mg 1# bid 四、【POMR 範本】Chronic polyarthritis 2011/01/11 10:30 AM S: Persistent painful swelling of multiple hand and foot joints with stiffness for 3 months. O: No fever, no skin rashes, no tophi. Swollen, tender bilateral MCP, wrist and MTP joints with pain on flexion and extension; warmth and tenderness of the knees with moderate-sized effusions Lab: WBC 9700/cumm with 80% neutrophils, 16% lymphocytes Platelet count 450K/cumm; ESR 65mm/hr; CRP 80mg/L ANA/Rheumatoid factor: pending the result X ray of both hands: soft tissue swelling of MCP and wrist joints. No bone erosion or joint space narrowing Problems #1: Chronic polyarthritis A: Chronic polyarthritis, suspect rheumatoid arthritis, suspect other autoimmune rheumatic disease, suspect polyarticular gout P: Arrange sono of joints for further assessment Arthrocentesis for both knee joints for synovial fluid analysis and culture Pursue the result of ANA and rheumatoid factors Keep sulindac 200mg 1# bid and Panadol 500mg 1# tid 五、【POMR 範本】Urticaria 2011/01/11 10:30 AM S: Generalized itching erythematous skin rashes for one week. No history of recent sea food ingestion or prior drug exposure. No dyspnea or dysphagia. O: BP 136/76mmHg, PR 96/min, RR 18/min, BT 36.6℃ No respiratory distress. No swelling of eyelids or lips. Clear breathing sound. No wheezing. Erythematous wheal-like skin lesions at trunk and four limbs. Problems #1: Acute urticaria A: Acute urticaria without associated angioedmea. No signs of anaphylaxis. P: Add zyrtec 10mg 1# bid, prednisolone 5mg 2# bid 六、【POMR 範本】Stevens-Johnson syndrome 2011/01/11 10:30 AM S: Progressive bullous and erythematous pruritic skin rashes at face, trunk and limbs for 3 days. The symptoms started after taking Tegretol for 2 weeks, which had been prescribed with the diagnosis of epilepsy. O: Fever (BT 38.3℃). No respiratory distress Injected conjunctiva of both eyes Edema of lips and eyelids Superficial erosions of the oral mucosa Erythematous maculopapular rashes at face, neck, trunk and four limbs Bullous formation at abdominal wall and back An ulceration on the penile meatus Lab: WBC 12000/cumm with 70% neutrophils, 10% lymphocytes, 14% eosinophils BUN 40mg/dl, Cr 1.3mg/dl, GOT 80 U/L, GPT 120 U/L Problems #1: Stevens-Johnson syndrome A: Stevens-Johnson syndrome, suspected Tegretol related drug eruption, active P: DC Tegretol Solumedrol 40mg IV Q6H, zyrtec 10mg 1# bid Consult ophthalmologist Wound and mouth care Blood culture for 2 sets 七、 【POMR 範本】Systemic lupus erythematosus with nephritis and nephrotic syndrome 2011/01/11 10:30 AM S: Leg edema O: She was hypertensive (blood pressure 170/90 mmHg) and had faint heart sounds and bilateral leg pitting edema. A biopsy-proven diffuse proliferative glomerulonephritis (WHO class IV) and hypocomplementemia. The laboratory studies disclosed leukocytes 15,900 /mm3, hemoglobulin 7.2 g/dl, platelets 179,000 /mm3, serum albumin 2.5 g/dL, C-reactive protein 2.2 mg/dL, positive ANA and anti-dsDNA antibodies, and low serum complement (C3: 29 mg/dL; C4: 7 mg/dL). Anti-cardiolipin antibodies were negative and coagulation tests were normal. Problems #1: Lupus nephritis A: Active lupus nephritis and nephrotic syndrome with hypoalbuminemia P: Methylprednisolone pulse therapy followed by high doses of prednisolone 八、【POMR 範本】Systemic lupus erythematosus with flare-up 2011/01/11 10:30 AM S: Low-grade fever last night O: Malar rashes, polyarthritis of hand joints, ascites. Hypertension (190/130 mmHg). The initial laboratory evaluations disclosed a leukocyte count of 5,900/mm3 with normal differential, hemoglobulin 9.7 g/dl, platelet count 111,000/mm3, BUN 32 mg/dl, creatine 2.1 mg/dl, serum albumin 3.4 g/dl, and C-reactive protein 4.6 mg/dl. The urinalysis revealed heavy proteinuria and gross hematuria. The chest radiogram showed marked enlargement of the cardiac silhouette. Problems #1: Systemic lupus erythematosus A: Flare-up of disease activity P: Treated with prednisolone 30 mg/day Problems #2: Proteinuria and hematuria A: Lupus nephritis, active P: Collect 24-h urine and arrange renal sonography 九、【POMR 範本】Systemic lupus erythematosus with fever 2011/01/11 10:30 AM S: Fever up to 39 C in this morning O: Pulse rate: 88/min, respiratory rate: 18/min, blood pressure: 120/70 mmHg. The laboratory evaluations showed a leukocyte count of 15,900/mm3, creatine 1.5 mg/dl, and C-reactive protein 12.6 mg/dl. The urinalysis revealed heavy pyuria. The chest radiogram showed no abnormalities. Problems #1: Urinary tract infection A: active infection P: Collect urine for bacterial culture and use empiric antibiotics therapy Problems #2: Systemic lupus erythematosus A: no active disease activity P: Treated with prednisolone 10 mg/day 十、【POMR 範本】Polymyositis 2011/01/11 10:30 AM S: Generalized weakness today O: No fever and no respiratory distress. Pulse rate: 80 per minute Unable to stand up from ground. Thigh muscle power: 4, upper arm muscle power: 4. High creatine kinase level at initial laboratory evaluations Problems #1: Polymyositis A: Newly diagnosed P: Arrange EMG for differential diagnosis of myopathy and use methylprednisolone 120 mg/day therapy 十一、【POMR 範本】Vasculitis 2011/01/11 10:30 AM S: Red papules over feet. O: Several 0.5–1 cm palpable non-thrombocytopenic purpuras appeared on the lower extremities; left foot drop was found at the same time. The physical examination was unremarkable except for some dry rales in the lower lung fields. The laboratory data disclosed a WBC count of 14,700/mm, a haemoglobulin level of 10.6 g/dL, a platelet count of 379,000/mm, an erythrocyte sedimentation rate of 118 mm/h, and a positive reaction of rheumatoid factor. Serum biochemistry profile and urinalysis were within normal limits, except for a low serum albumin level An electromyographic study revealed the typical changes of MNM involving the bilateral tibial, peroneal, sural, and left median nerves. A left sural nerve biopsy showed severe axonal degeneration and a marked non-uniform loss of myelinated fibres, which were compatible with the findings of ischaemic neuropathy with active axonopathy. Problems #1: Vasculitis A: Mononeuropathy multiplex P: The dose of prednisolone (60 mg daily) was used.